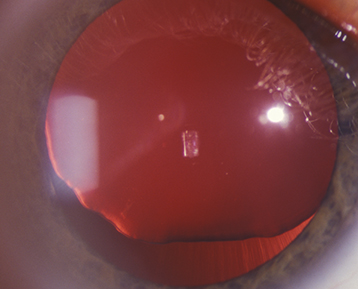
(See Figure 13.2.1.)
Decentered or displaced lens, iridodonesis (quivering of the iris), and phacodonesis (quivering of the lens).
Change in refractive error, marked astigmatism, cataract, angle-closure glaucoma as a result of pupillary block, vitreous in the anterior chamber, and asymmetry of the anterior chamber depth.