Usually without ocular symptoms. Floaters, flashing lights, or loss of vision with advanced disease. Systemically, patients often have painful crises with severe abdominal or musculoskeletal pain. Patients are typically of African or Mediterranean descent.
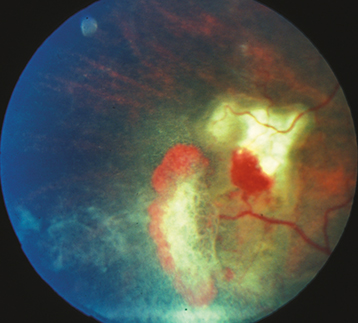
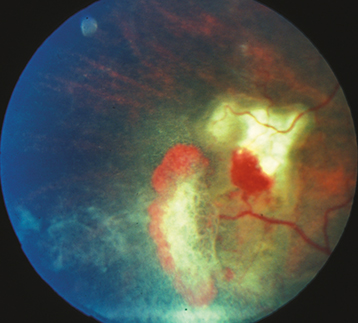
(See Figure 11.20.1.)
Figure 11.20.1: Sickle cell retinopathy neovascular sea fan with associated vitreous hemorrhage.
Critical
Peripheral retinal neovascularization in the shape of a fan (“sea fan sign”), sclerosed peripheral retinal vessels, or a dull gray peripheral fundus background color as a result of peripheral arteriolar occlusions and ischemia.
Other
Venous tortuosity, midperipheral fundus pigmented lesions with spiculated borders (black sunbursts), superficial intraretinal hemorrhages (salmon patch), refractile (iridescent) intraretinal deposits following hemorrhage resorption, angioid streaks, comma-shaped capillaries of the conjunctiva (especially along the inferior fornix). VH and traction bands, RD, CRAO, macular arteriolar occlusions, and enlargement of the foveal avascular zone occasionally develop.
Staging
Stage 1: Peripheral arteriolar occlusions.
Stage 2: Peripheral arteriovenous anastomoses (hairpin loop).
Stage 3: Neovascular proliferation (sea fan).
Stage 4: VH.
Stage 5: RD.
Differential Diagnosis of Peripheral Retinal Neovascularization
Sarcoidosis: Peripheral sea fan neovascularization often associated with uveitis. Increased frequency in young patients of African descent.
Diabetic retinopathy: Posterior pathology more prominent. Associated dot-blot hemorrhages. See 11.12, Diabetic Retinopathy.
Embolic (e.g., talc) retinopathy: History of intravenous drug abuse. May see refractile talc particles in macular arterioles. See 11.33, Crystalline Retinopathy.
Eales disease: Peripheral retinal vascular occlusion of unknown etiology; diagnosis of exclusion.
Others: Retinopathy of prematurity, FEVR, chronic myelogenous leukemia, radiation retinopathy, pars planitis, carotid–cavernous fistula, OIS, collagen vascular disease, hypercoagulable state. See specific sections.
Medical history and family history: Sickle cell disease, diabetes, or known medical problems? Intravenous drug abuse?
Dilated fundus examination using indirect ophthalmoscopy.
Sickledex, sickle cell preparation, and hemoglobin electrophoresis.
|
 NOTE NOTEPatients with sickle cell trait (i.e., HbSC), as well as hemoglobin C disease, may have a negative Sickledex preparation. Retinopathy is most common with HbSC (most severe) and HbS-Thal and less common with HbSS (sickle cell disease). |
Consider ultra widefield IVFA to assess retinal perfusion and neovascularization, especially in the periphery. OCTA can identify vascular density loss corresponding to areas of retinal thinning.