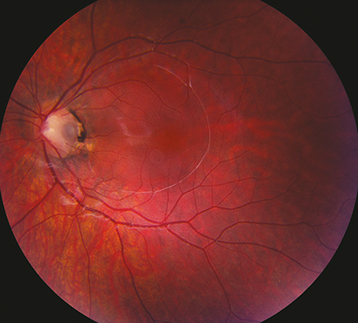
(See Figure 11.34.1.)
Small, round depression (usually gray, yellow, or black in appearance) in the nerve tissue of the optic disc. Most are temporal, approximately one-third are central, but may be present anywhere on the nerve head.
Peripapillary atrophy, white or gray membrane overlying pit, rarely RAPD, various visual field defects. May develop localized detachment of the sensory retina and/or retinoschisis extending from the disc to the macula, usually unilateral.