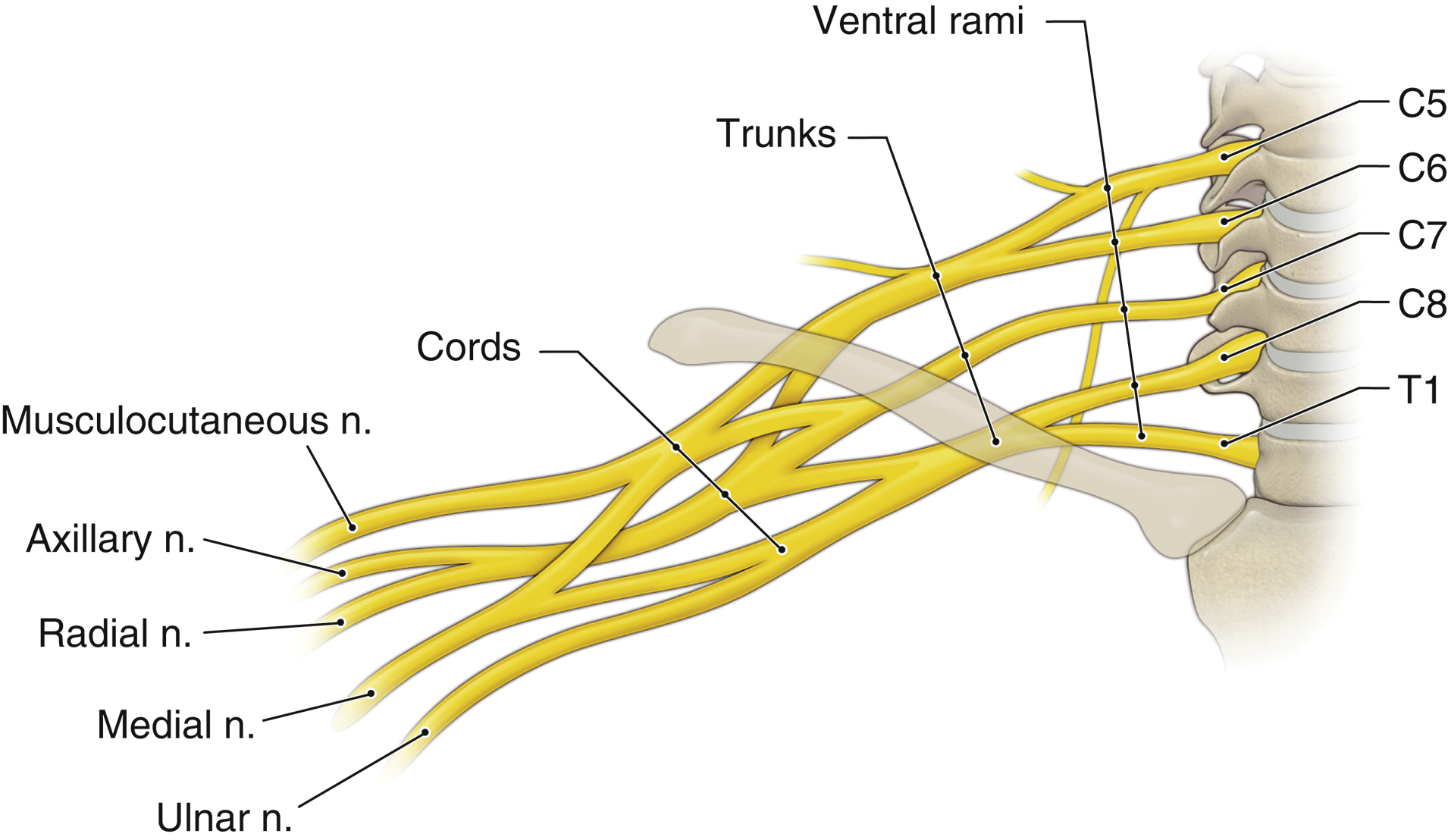
- Anatomy (Figure 21.4)
- The shoulder, axilla, and upper extremity are innervated by the brachial plexus (BP). Skin of the medial aspect of the upper arm is innervated by the intercostobrachial nerve formed by T2 and the medial cutaneous nerve of the arm. The supraclavicular nerve, which is formed by C3-C4, innervates the skin of the top of the shoulder (see Section VI.A.1).
- The BP is formed from the ventral rami of the spinal nerves from C5 to C8 and T1, with frequent contributions from C4 and T2. It is traditionally divided into five parts: roots, trunks, divisions, cords, and branches.
- Each root or ventral ramus exits posterior to the vertebral artery and travels laterally in the trough of its cervical TP, sandwiched between the fascial sheaths of the anterior and middle scalene muscles.
- The trunks (superior, middle, and inferior) pass over the first rib through the space between the anterior and middle scalene muscles in association with the subclavian artery, which shares the same fascial sheath.
- As the trunks pass over the first rib and under the clavicle, they split into the anterior (flexor) and posterior (extensor) divisions, which then reorganize to form the three cords (lateral, medial, and posterior, named for their usual positions relative to the axillary artery) of the plexus.
- Branches of the lateral and medial cords form the median nerve. The lateral cord also gives off a branch that forms the musculocutaneous nerve. The medial cord also forms the ulnar, medial antebrachial cutaneous, and medial brachial cutaneous nerves. The posterior cord becomes the axillary and radial nerves (Figure 21.4). In the axilla, the median nerve classically lies lateral to the axillary artery, the radial nerve posterior and over the conjoint tendon (of the teres major and latissimus dorsi muscles), and the ulnar nerve medial, but variation in these relative positions may occur. The musculocutaneous and axillary nerves exit the sheath high up in the axilla. The musculocutaneous nerve travels through the coracobrachialis muscle before becoming subcutaneous below the elbow, and the axillary nerve travels through the quadrilateral space (bordered by the humeral shaft, long head of the triceps, and teres major and minor muscles) before dividing into its terminal branches.
- The dermatome distribution of the nerves of the body is summarized in Figure 21.3. Cutaneous innervation does not necessarily correlate with deep structures, including the bones; therefore, knowledge of the osteotomes can be very useful in predicting the ultimate success of any regional technique.
- The major motor functions of the five nerves are as follows: axillary (circumflex nerve): shoulder abduction; musculocutaneous: elbow flexion; radial: wrist and finger extension; median: forearm pronation, wrist and finger flexion, thumb flexion and opposition; and ulnar: wrist flexion and adduction, thumb adduction.
- Indications
- The interscalene approach blocks the BP at the level of the roots to upper trunks. This approach is most useful for surgeries of the shoulder and proximal humerus. As the inferior trunk (C8-T1) and therefore ulnar nerve is usually spared, it is less useful for forearm and hand operations.
- The supraclavicular approach blocks the plexus at the level of the trunks to divisions. This approach allows for reliable anesthesia of the entire arm distal to the shoulder.
- The infraclavicular approach blocks the plexus at the level of the cords and provides coverage for surgery distal to the mid-humerus.
- The axillary approach blocks the terminal branches of the BP. The block is combined with blockade of the musculocutaneous nerve and is used for surgical procedures involving the forearm and hand.
- The intercostobrachial nerve must be blocked in addition to the BP for procedures involving the medial arm or using a proximal humeral tourniquet.
- Suprascapular and axillary nerve blocks provide shoulder analgesia similar to that of an interscalene block but avoid complications like phrenic nerve paralysis, which almost always occurs with interscalene block.
- Blockade of an individual peripheral nerve may be useful when limited anesthesia is required or a BP block is incomplete and requires a rescue block.
- Techniques and complications
- Interscalene block using UGRA (Figure 21.5;
 ): Position the patient supine and semi-reclined or lateral decubitus with the arms at the side and head turned away from the side to be blocked. Place the probe over the SCM at the level of the cricoid cartilage (C6) and identify the internal carotid artery and internal jugular vein. Move the probe laterally and identify the anterior and middle scalene muscles. At this time, the roots and trunks, usually C5 and two branches of C6, will come into view as hypoechoic nodular structures often stacked in a “stoplight” configuration between the anterior and middle scalene. After centering the nerves on the screen, infiltrate with LA and insert a 22-gauge 50-mm needle just lateral to the probe site and advance with IP approach toward the target nerves in a lateral-to-medial direction. Stimulation of the BP using PNS will result in a muscle twitch in the deltoid, biceps, triceps, or pectoralis major muscles. After negative aspiration, deposit 15 to 20 mL LA solution between the two scalene muscles.
): Position the patient supine and semi-reclined or lateral decubitus with the arms at the side and head turned away from the side to be blocked. Place the probe over the SCM at the level of the cricoid cartilage (C6) and identify the internal carotid artery and internal jugular vein. Move the probe laterally and identify the anterior and middle scalene muscles. At this time, the roots and trunks, usually C5 and two branches of C6, will come into view as hypoechoic nodular structures often stacked in a “stoplight” configuration between the anterior and middle scalene. After centering the nerves on the screen, infiltrate with LA and insert a 22-gauge 50-mm needle just lateral to the probe site and advance with IP approach toward the target nerves in a lateral-to-medial direction. Stimulation of the BP using PNS will result in a muscle twitch in the deltoid, biceps, triceps, or pectoralis major muscles. After negative aspiration, deposit 15 to 20 mL LA solution between the two scalene muscles.Complications. Phrenic nerve palsy and hemidiaphragm paralysis almost always occurs. The cervical sympathetic nerve block can produce an ipsilateral Horner syndrome.
Figure 21-5 Superficial cervical plexus/interscalene block using ultrasound (US) guidance.
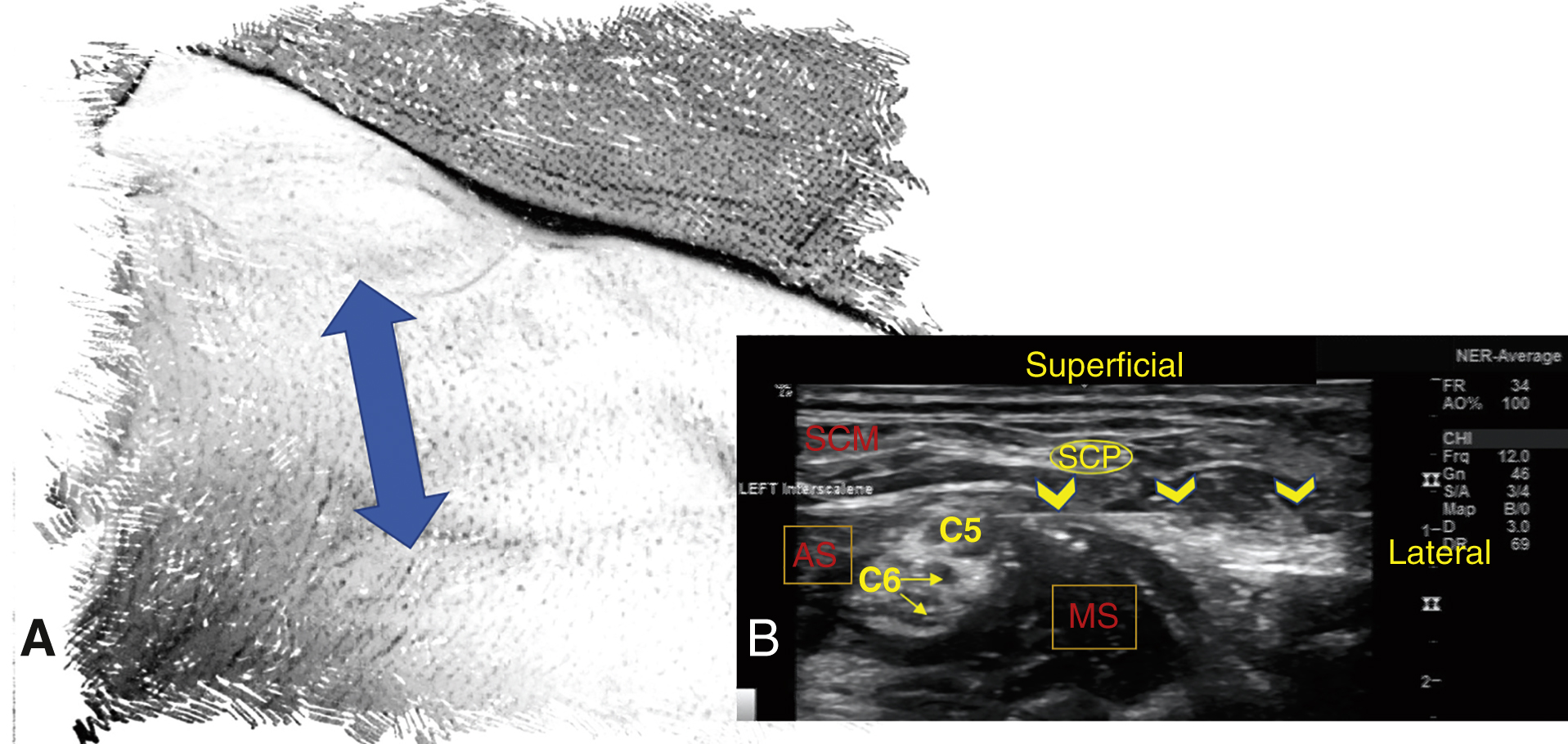
A, The two-sided arrow shows the placement of the US probe. B, US image of brachial plexus (C5 and C6) at the level of interscalene. The yellow arrows delineate the path of the needle toward the plexus. AS, anterior scalene muscle; MS, middle scalene muscle; SCM, sternocleidomastoid; SCP, superficial cervical plexus.
- Supraclavicular block using UGRA (Figure 21.6;
 ): Position the patient similar to that for the interscalene block. A blanket roll or pillow behind the shoulder may facilitate visualization. Place the probe in the transverse plane with caudal tilt in the supraclavicular fossa. The BP will be visualized as a hypoechoic group of nerves (“cluster of grapes”) located laterally and posterior to the subclavian artery. Deep to the artery, the hyperechoic first rib and part of the pleura are typically seen, with the portions of the pleura often obscured by the rib’s acoustic shadow. Insert a 22-gauge 50-mm needle just lateral to the probe and advance IP in lateral-to-medial direction until it reaches the BP. Stimulation of the BP using PNS is manifested by a twitch of the fingers in flexion or extension. After negative aspiration, slowly administer 15 to 20 mL of LA solution. LA should spread throughout the BP, between the middle scalene and subclavian artery, just above the first rib.
): Position the patient similar to that for the interscalene block. A blanket roll or pillow behind the shoulder may facilitate visualization. Place the probe in the transverse plane with caudal tilt in the supraclavicular fossa. The BP will be visualized as a hypoechoic group of nerves (“cluster of grapes”) located laterally and posterior to the subclavian artery. Deep to the artery, the hyperechoic first rib and part of the pleura are typically seen, with the portions of the pleura often obscured by the rib’s acoustic shadow. Insert a 22-gauge 50-mm needle just lateral to the probe and advance IP in lateral-to-medial direction until it reaches the BP. Stimulation of the BP using PNS is manifested by a twitch of the fingers in flexion or extension. After negative aspiration, slowly administer 15 to 20 mL of LA solution. LA should spread throughout the BP, between the middle scalene and subclavian artery, just above the first rib.Complications include pneumothorax (0.04% with UGRA), phrenic nerve block, and Horner syndrome.
Figure 21-6 Supraclavicular block using ultrasound guidance.
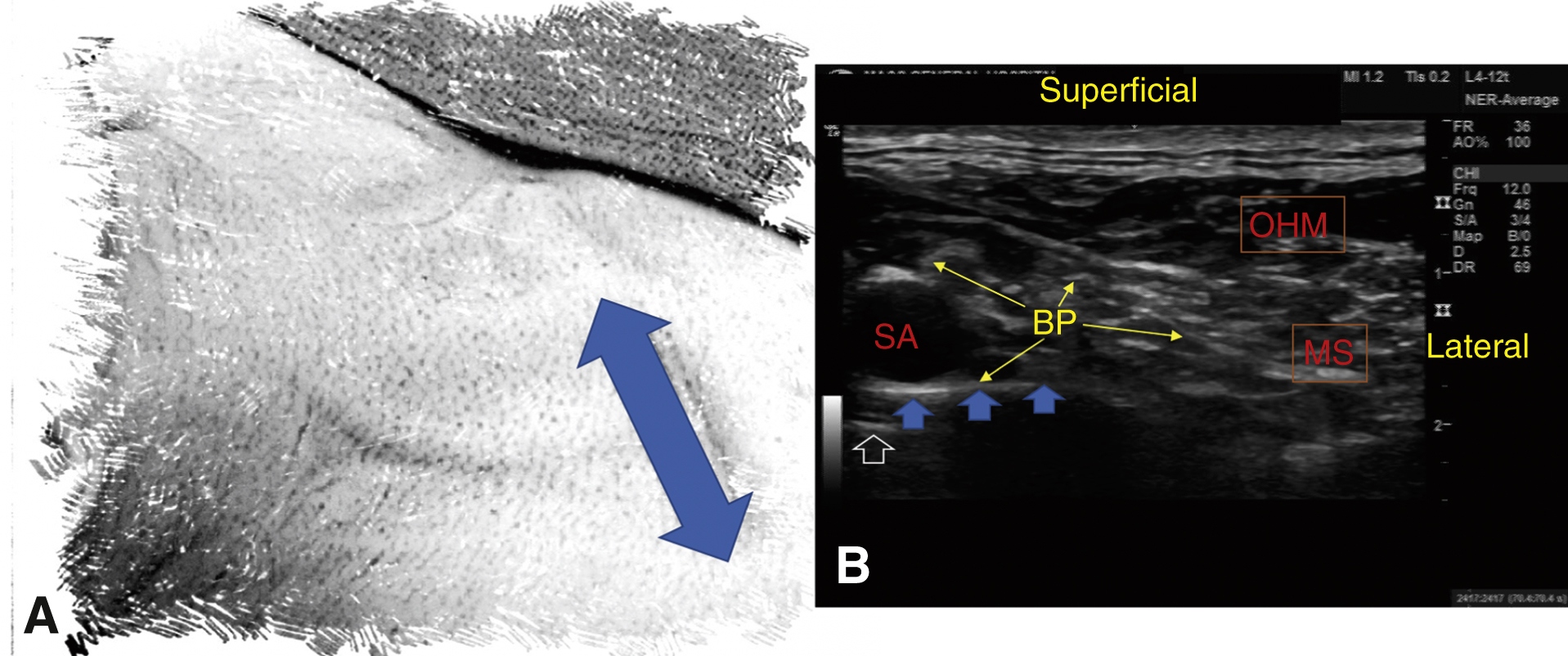
A, The two-sided arrow shows the placement of the US probe. B, The BP is at the posterolateral border of the SA and superior to the first rib (blue arrows). The pleura can be seen as a hyperechoic line deep to the first rib (white arrow). BP, brachial plexus; MS, middle scalene muscle; OHM, omohyoid muscle; SA, subclavian artery.
- Infraclavicular block using UGRA (Figure 21.7,
 ): Position the patient supine with arm supinated and abducted 90° at the shoulder, with the forearm supinated. Place the probe in the infraclavicular fossa (at the deltopectoral groove) and under the coracoid process. Identify the axillary artery and vein with hyperechoic lateral, posterior, and medial cords lying in a U-shape configuration around the artery. A needle-insertion site is identified approximately 1 cm superior to the probe, just inferior to the clavicle. A 22-gauge 100- to 150-mm needle is appropriate. Insert the needle and advance caudally at a steep angle to the skin in an IP approach until the tip is positioned posterior to the axillary artery (ie, in the 6-o’clock position). PNS stimulation of the posterior cord will produce extension at the wrist and/or finger (radial nerve) and stimulation of the medial cord produces flexor carpi ulnaris movement with some flexion of the wrist and/or fingers (median and ulnar nerves); stimulation of the posterior cord generally results in a higher success rate. After negative aspiration, deposit 20 to 30 mL of LA solution with a goal of U-shaped spread around the axillary artery. This may require repositioning the needle to achieve the desired spread and coverage of the medial and lateral cords.
): Position the patient supine with arm supinated and abducted 90° at the shoulder, with the forearm supinated. Place the probe in the infraclavicular fossa (at the deltopectoral groove) and under the coracoid process. Identify the axillary artery and vein with hyperechoic lateral, posterior, and medial cords lying in a U-shape configuration around the artery. A needle-insertion site is identified approximately 1 cm superior to the probe, just inferior to the clavicle. A 22-gauge 100- to 150-mm needle is appropriate. Insert the needle and advance caudally at a steep angle to the skin in an IP approach until the tip is positioned posterior to the axillary artery (ie, in the 6-o’clock position). PNS stimulation of the posterior cord will produce extension at the wrist and/or finger (radial nerve) and stimulation of the medial cord produces flexor carpi ulnaris movement with some flexion of the wrist and/or fingers (median and ulnar nerves); stimulation of the posterior cord generally results in a higher success rate. After negative aspiration, deposit 20 to 30 mL of LA solution with a goal of U-shaped spread around the axillary artery. This may require repositioning the needle to achieve the desired spread and coverage of the medial and lateral cords.Complications include pneumothorax in addition to those mentioned in Section III.
Figure 21-7 Infraclavicular block using ultrasound guidance.
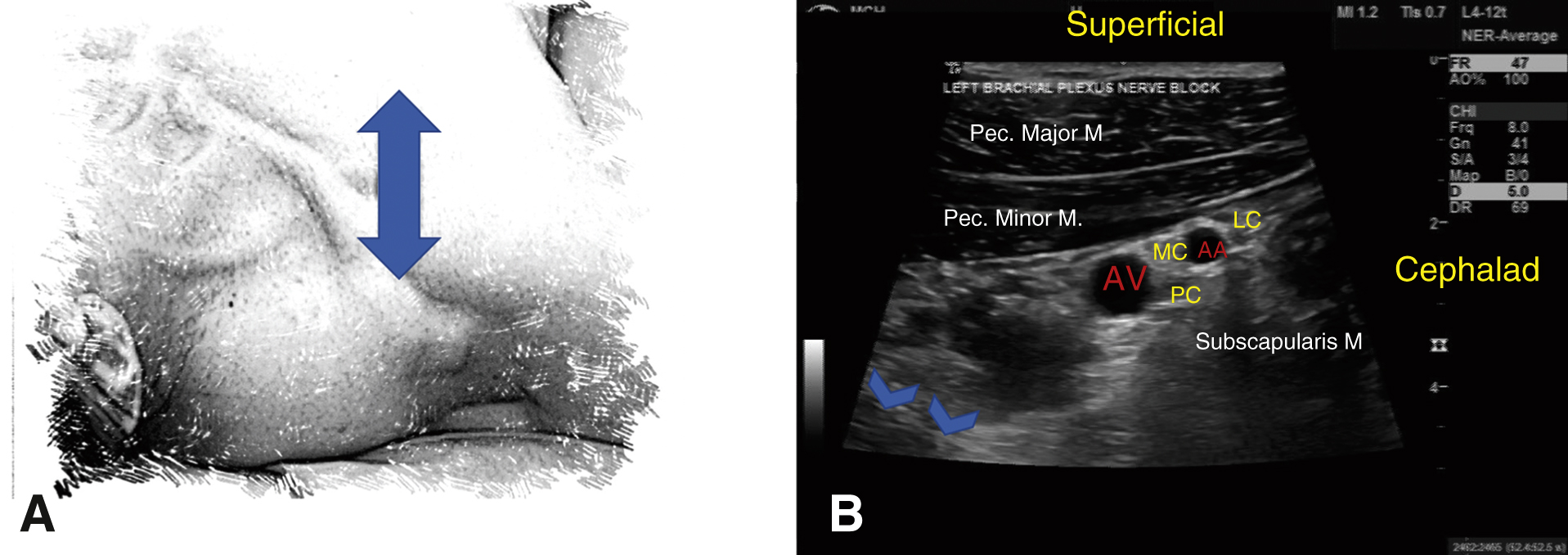
A, The two-sided arrow shows the placement of the US probe. B, The LC, MC, and PC are located around the AA. The PC can be obscured by the acoustic enhancement of the artery. The blue arrows designate the pleura. AA, axillary artery; AV, axillary vein; LC, lateral cord; MC, medial cord; PC, posterior cord.
- Axillary block using UGRA (Figure 21.8;
 ): Position the patient supine with the arm abducted 90° at the shoulder, externally rotated and flexed at the elbow. Place the transducer over the axillary artery, perpendicular to the axis of the arm, and position the artery in the center of the screen. The hyperechoic median, ulnar, and radial nerves can be appreciated in the perivascular area. Special care should be taken to identify veins as pressure from the transducer may easily compress and obscure them from view. Insert a 22-gauge 25- to 50-mm needle superior to the transducer and advance toward the nerves with IP approach. PNS stimulation of each nerve will result in different motor stimulation (see Section VII.A.8). After negative aspiration, inject a total of 20 to 30 mL of LA near each terminal nerve. The goal is to cover each of the terminal nerves, which may be achieved by a single injection of 5 to 7 mL of LA around the median, radial, and ulnar nerves. Next, identify the musculocutaneous nerve as a hyperechoic oval or triangular structure between the coracobrachialis and biceps muscles or within one of the muscles. Without changing the needle entry site, redirect the needle adjacent to the nerve and inject 5 to 7 mL of LA solution. PNS stimulation of the musculocutaneous nerve leads to flexion of the elbow.
): Position the patient supine with the arm abducted 90° at the shoulder, externally rotated and flexed at the elbow. Place the transducer over the axillary artery, perpendicular to the axis of the arm, and position the artery in the center of the screen. The hyperechoic median, ulnar, and radial nerves can be appreciated in the perivascular area. Special care should be taken to identify veins as pressure from the transducer may easily compress and obscure them from view. Insert a 22-gauge 25- to 50-mm needle superior to the transducer and advance toward the nerves with IP approach. PNS stimulation of each nerve will result in different motor stimulation (see Section VII.A.8). After negative aspiration, inject a total of 20 to 30 mL of LA near each terminal nerve. The goal is to cover each of the terminal nerves, which may be achieved by a single injection of 5 to 7 mL of LA around the median, radial, and ulnar nerves. Next, identify the musculocutaneous nerve as a hyperechoic oval or triangular structure between the coracobrachialis and biceps muscles or within one of the muscles. Without changing the needle entry site, redirect the needle adjacent to the nerve and inject 5 to 7 mL of LA solution. PNS stimulation of the musculocutaneous nerve leads to flexion of the elbow.Complications include LAST secondary to injection into the axillary artery or vein in addition to those mentioned in Section III.
Figure 21-8 Axillary block using ultrasound guidance.
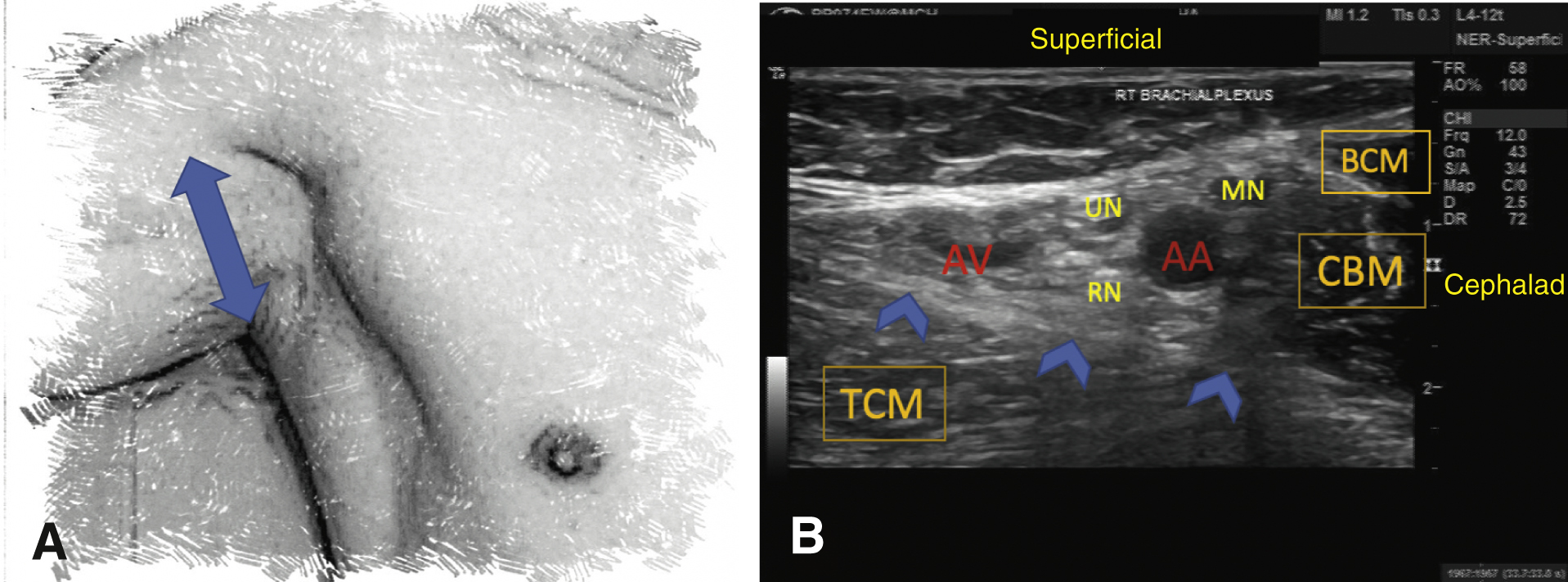
A, The two-sided arrow shows the placement of the US probe. B, The axillary approach to the terminal branches of the brachial plexus is achieved by placement of the US probe over the axillary artery. The blue arrows trace the conjoined tendon of the latissimus dorsi and teres major muscle. AA, axillary artery; AV, axillary vein; BCM, biceps muscle; CBM, coracobrachialis muscle; MN, median nerve; RN, radial nerve; TCM, triceps muscle; UN, ulnar nerve.
- Intercostobrachial nerve block: Insert a 25-gauge needle inferior to the axillary artery at the level of the axillary fossa. Subcutaneously infiltrate 5 mL of LA superiorly and inferiorly along the axillary crease. Complications are rare given the superficial nature of the block.
- Suprascapular and axillary nerve block: A suprascapular nerve block with or without axillary nerve block is considered a phrenic nerve-sparing regional anesthesia technique for shoulder surgery.
- Suprascapular nerve block using UGRA: With the posterior approach, position the patient in the lateral position, with shoulder fully adducted. Place the ultrasound probe transversely over the supraspinous fossa, and trace it from the medial end of the spine of the scapula to the greater suprascapular notch laterally. Insert a 22-gauge needle and advance with an IP approach to the lateral aspect of the supraspinous fossa, beneath the supraspinatus muscle. After negative aspiration, inject 10 to 12 mL of LA. With the anterior approach, position the patient and the probe as for supraclavicular block. Identify the omohyoid muscle on the top of the brachial plexus. Follow the omohyoid muscle laterally and posteriorly. Locate the suprascapular nerve as it separates from the upper truck. Insert a 22-gauge needle and advance with an IP approach under the inferior belly of the omohyoid muscle. Inject 10 to 12 mL of LA adjacent to the nerve.
- Axillary nerve block using UGRA: Position the patient in the lateral position. Locate the humeral head and neck on the posterolateral aspect of the arm. Identify the humeral circumflex artery and visualize the axillary nerve located superior to the artery. Advance a 22-gauge needle IP through the deltoid muscle, and after negative aspiration, deposit 10 mL of LA solution around the axillary nerve. LA should fill the potential space between the deltoid and posterior surface of the humerus.
- Complications include concurrent radial nerve block due to spread of the LA proximally to the posterior cord in addition to those in Section III. As the suprascapular and/or the axillary nerve block do not anesthetize the other three terminal nerves of C5 and C6, supplemental analgesic is frequently necessary.
- Blockade of an individual terminal nerve of the BP
- Ulnar nerve block using UGRA: At the forearm, the ulnar nerve is just lateral to the flexor carpi ulnaris and medial to the ulnar collateral artery, lying over the flexor digitorum profundus. Place the ultrasound probe transversally over the mid-forearm, and using an IP approach, inject 3 to 6 mL of LA around the nerve.
- Median nerve block using UGRA: At the elbow, the median nerve is just medial to the brachial artery and on the top of the brachialis muscle at the level of the epicondyles. Using the same approach as above for the ulnar nerve, inject 3 to 5 mL of LA around the median nerve, avoiding penetration of the brachial artery. At the wrist, the median nerve lies between the palmaris longus tendon and the flexor carpi radialis tendon. At this level, isolating the nerve from the tendons can be difficult with ultrasound. Sliding the probe alongside the forearm will help to visually separate tendons from the nerve, as tendons become muscles and their appearance will change while the nerve will stay the same. The approach is the same as above at the elbow.
- Radial nerve block using UGRA: At the elbow, the radial nerve lies lateral to the biceps tendon and medial to the brachioradialis muscle, at the level of the lateral epicondyle of the humerus. Place the ultrasound probe transversally about 3 to 4 cm above the lateral epicondyle to locate the radial nerve. Follow the radial nerve until it reaches the lateral margin of the humerus to confirm the nerve. Use an IP approach to reach the nerve and inject 3 to 5 mL of LA around it.
- Lateral cutaneous nerve of the forearm block using UGRA: This is the primary cutaneous branch of the musculocutaneous nerve. It may be blocked in the axilla, as described in Section VII.C.4, or at the elbow, where is it usually located on the lateral side of the forearm and can be seen between the biceps tendon and the brachioradialis muscle, usually accompanying the cephalic vein. Block technique is the same as above, but with 5 to 10 mL of LA.
- Interscalene block using UGRA (Figure 21.5;
- Intravenous (IV) RA (Bier block): IV administration of LA distal to a tourniquet is a simple way to anesthetize an extremity for short procedures (60 minutes or less).
- Place a 20- to 22-gauge IV catheter as distally as possible in the extremity to be blocked. Apply a pneumatic double tourniquet proximally and exsanguinate the extremity by elevating it and wrapping it distally to proximally with an Esmarch bandage.
- Inflate the proximal cuff to 150 mm Hg greater than systolic pressure. Absence of pulses after inflation ensures arterial occlusion. Remove the Esmarch bandage and slowly inject the anesthetic into the previously placed IV catheter. Average drug doses are 50 mL of 0.5% lidocaine for an arm. Although Bier block has been described for the leg, it is generally not utilized as it is difficult to achieve complete vascular occlusion of the leg with a tourniquet and the volume of LA required increases the risk of systemic toxicity.
- Anesthesia occurs within 5 minutes of LA injection. Tourniquet pain generally becomes unbearable after 1 hour and is the limiting factor for the success of this technique. When the patient complains of pain, the distal tourniquet that overlies the anesthetized skin should be inflated and the proximal tourniquet released.
- The major complication associated with IV RA is LA toxicity. It may occur during injection if the tourniquet fails or after tourniquet deflation, particularly with a short inflation time.