Cervical plexus block (CPB)
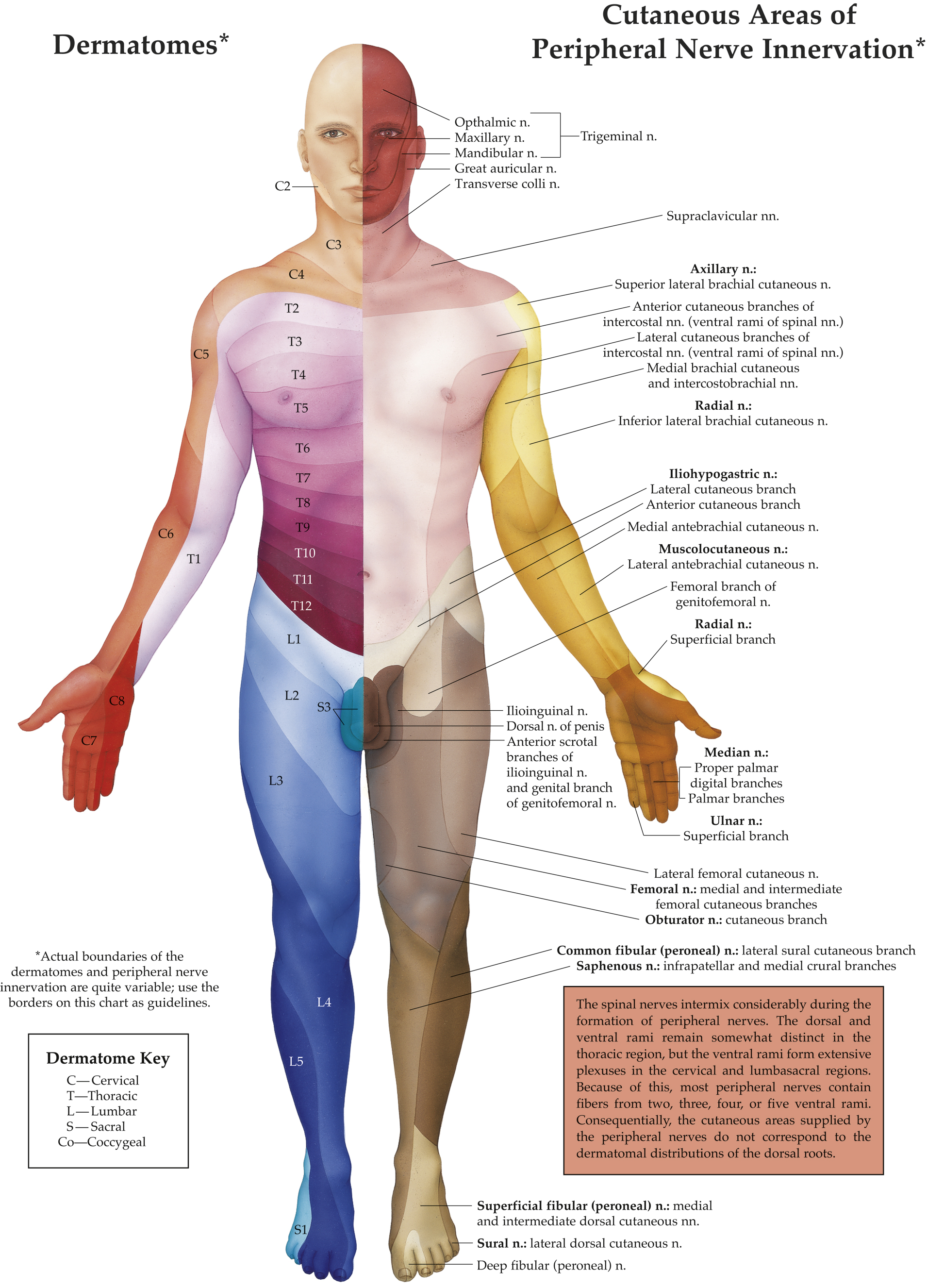
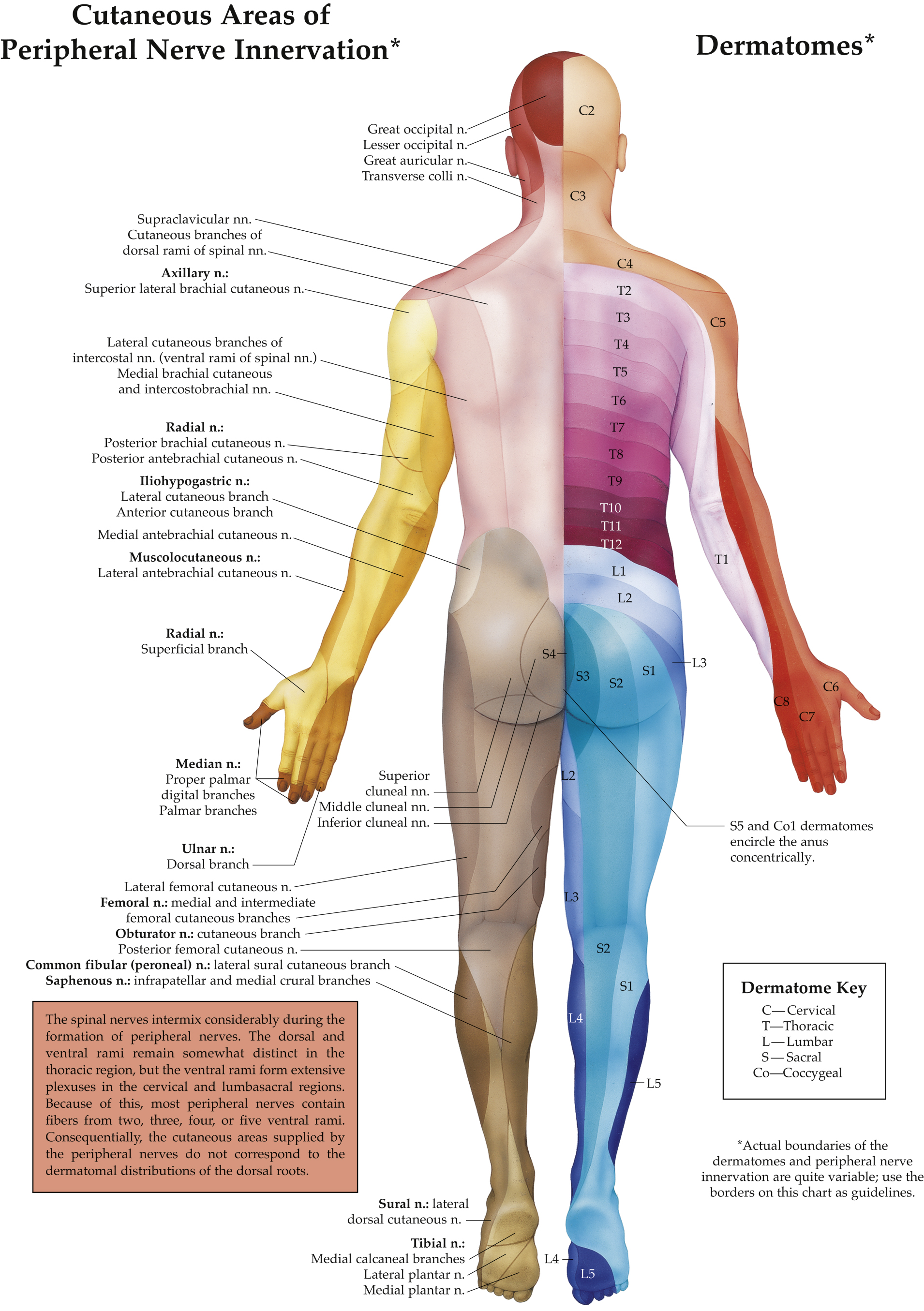
- Anatomy. The cervical plexus lies in the paravertebral region of the upper four cervical vertebrae, formed from the anterior rami of the C1-C4 spinal nerve roots. The plexus is situated between the prevertebral muscle anteromedially and the muscles attached to the posterior tubercles of the cervical transverse processes (TP) posterolaterally. The plexus has cutaneous, muscular, and communicating branches. The superficial cutaneous branches, which include the lesser occipital, greater auricular, transverse cervical, and supraclavicular nerves, pierce the prevertebral fascia anteriorly, just deep to the sternocleidomastoid muscle (SCM) at the level of the C5 TP. They innervate the skin and fascia of the back of the head, lateral neck, top of the shoulder and chest, and the clavicle (Figure 21.3). The deep muscular branches are deep to the prevertebral fascia and supply the muscles and deep structures of the neck and form the phrenic nerve.
Figure 21-3 A map of the dermatomes.
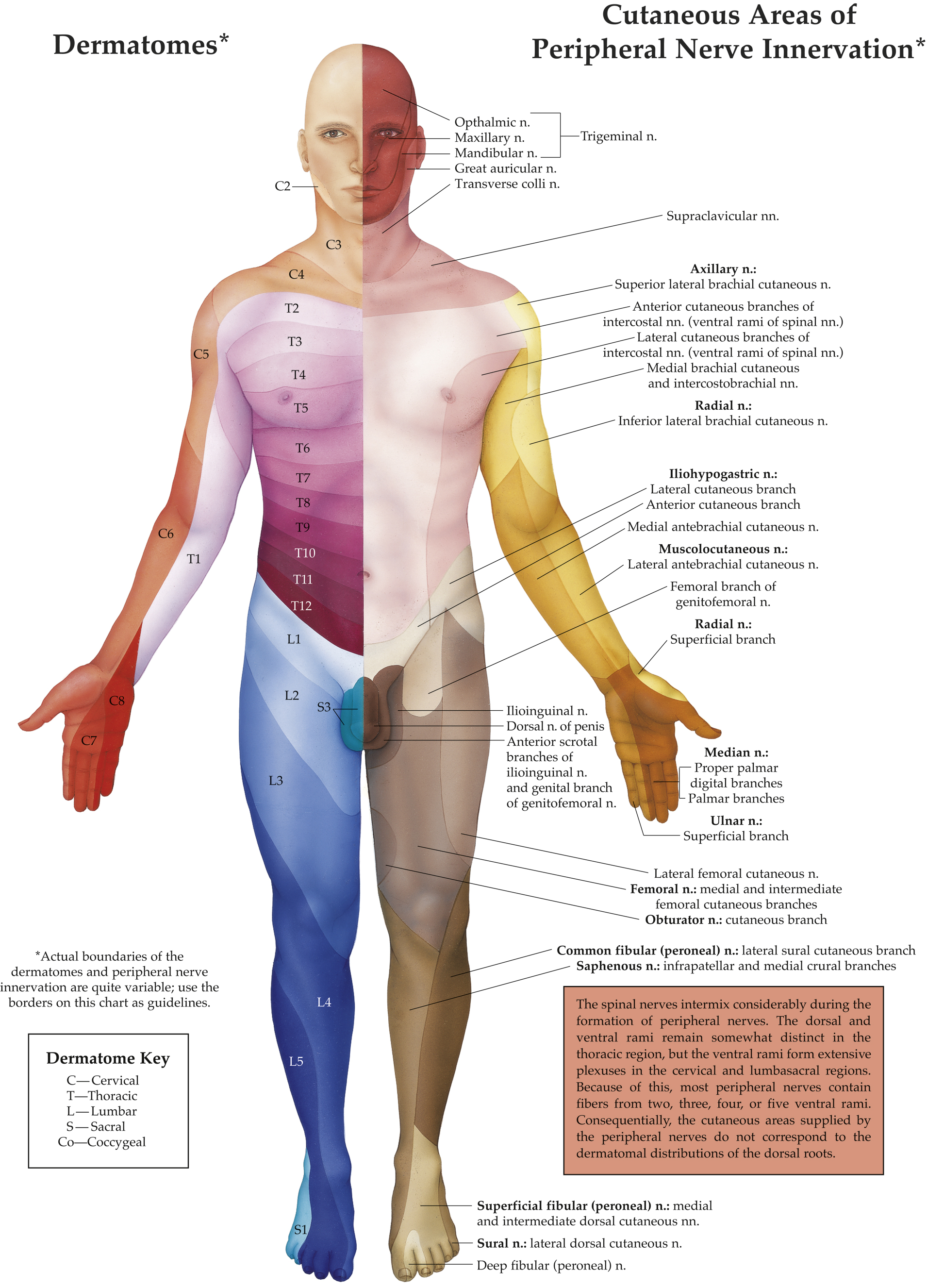
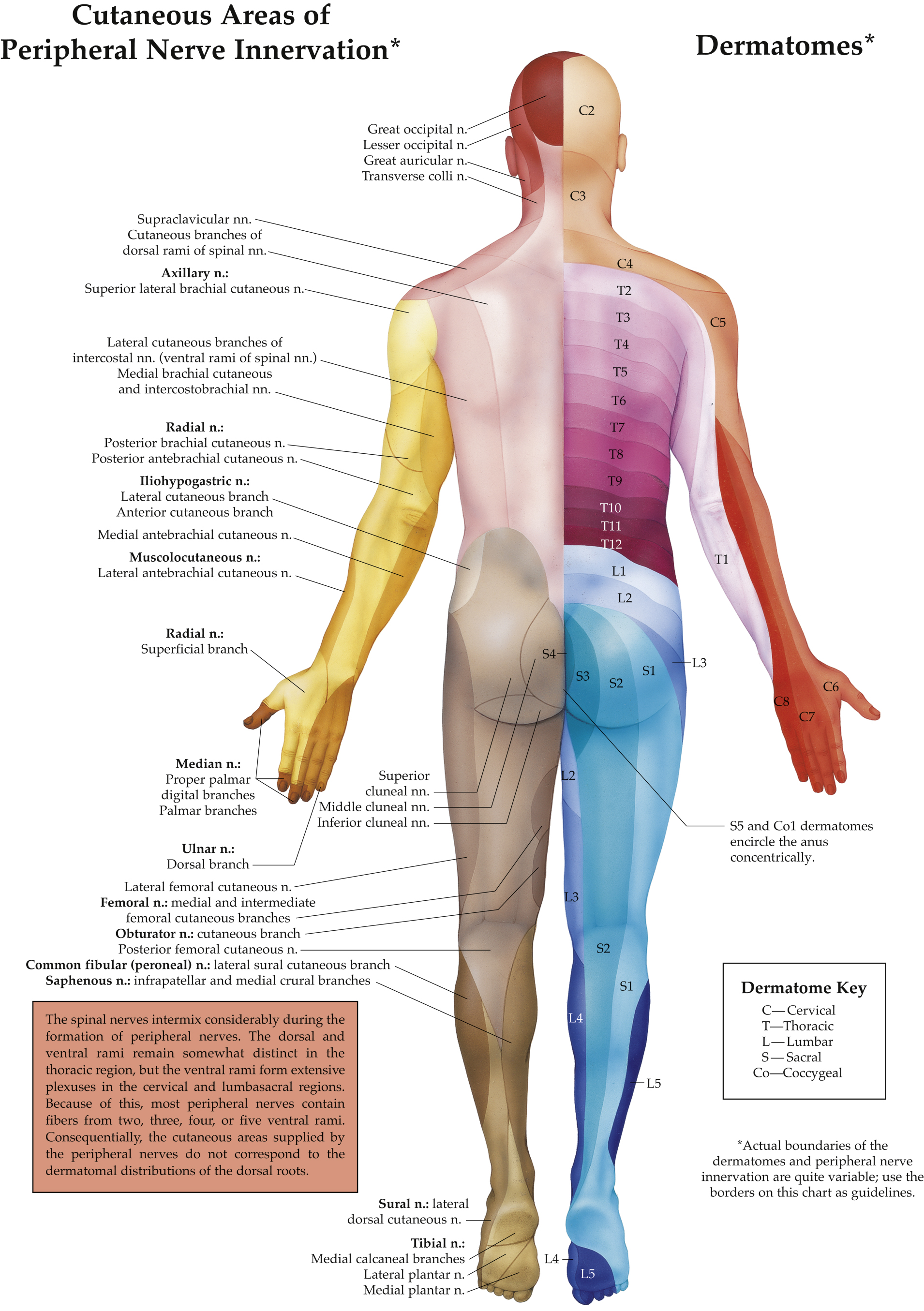
(Adapted from Anatomical Chart Company. Dermatomes Anatomical Chart. Wolters Kluwer; 2004 and Jaffe RA, SchmiesingCA, GolianuB, eds. Anesthesiologist’s Manual of Surgical Procedures. 6th ed. Wolters Kluwer; 2020.)
- Indications. Superficial CPB (C2-C4) produces cutaneous anesthesia and is useful for superficial procedures on the neck and shoulder. It has been shown that superficial CPB is as effective as paravertebral cervical root block, known previously as deep CPB, for carotid endarterectomy with fewer complications.
- Superficial CPB using UGRA (see Figure 21.5): Position the patient supine with the neck slightly extended and the head turned toward the opposite side. Place the ultrasound probe transversely over the SCM at the level of the cricoid cartilage and scan posteriorly until the posterior edge of the SCM is visualized in the center of the screen. The SCP may be visualized as two to three small hypoechoic structures between the SCM and scalene muscles. Using an IP approach, insert a 23- to 25-gauge 50-mm needle lateral to the probe and advance until the needle tip is beneath the posterior border of the SCM and adjacent to the plexus. After negative aspiration, inject 10 mL of LA in a fan-like fashion along the posterior border of the SCM, 2 to 3 cm above and below the needle insertion site. LA should spread between the SCM and the underlying prevertebral fascia.
- Complications. Vagus nerve block and recurrent laryngeal nerve block can occur if LA spreads too medially, causing hoarseness and vocal cord dysfunction.