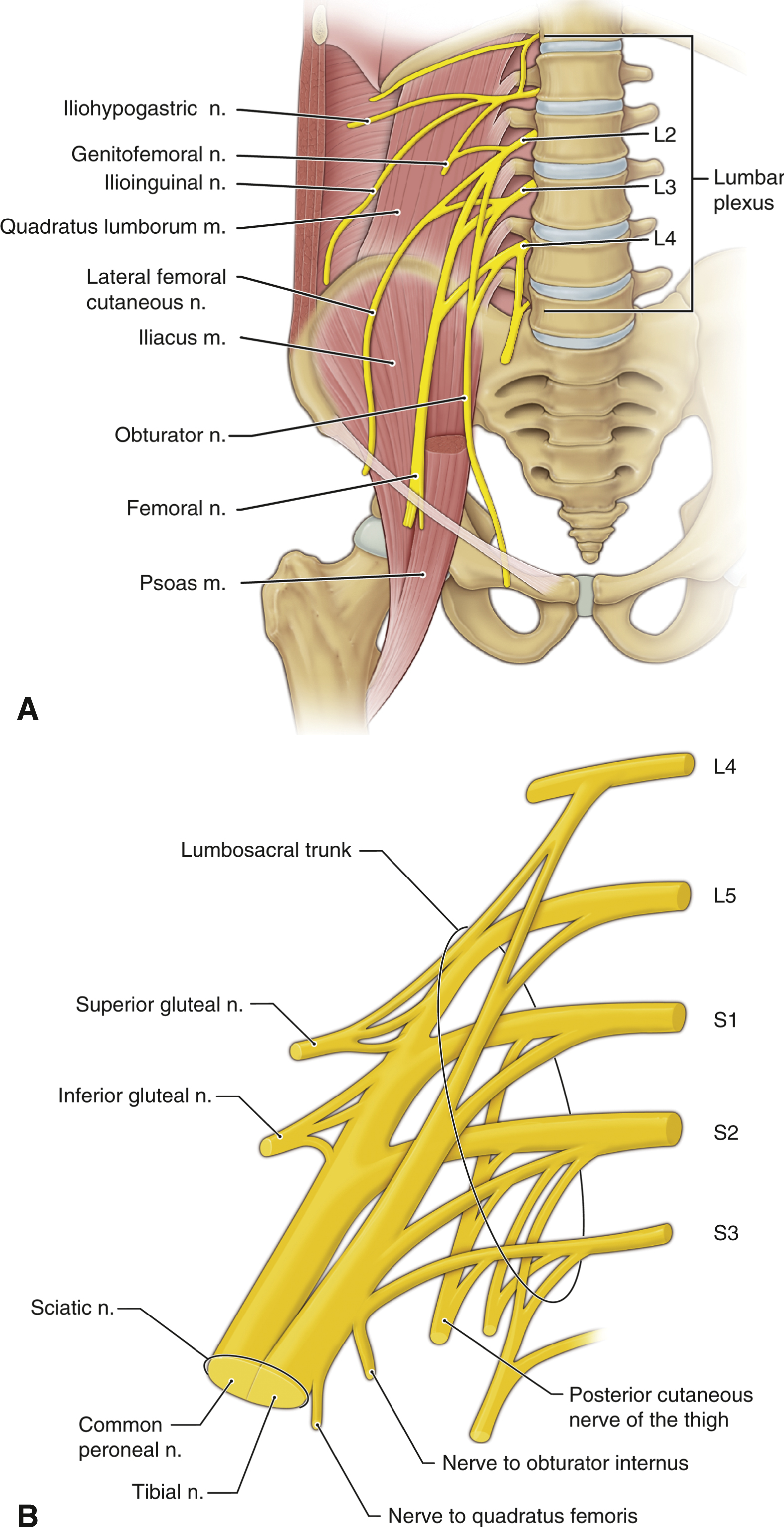
- Anatomy. There are two major plexuses that innervate the lower extremity: the lumbar plexus and the sacral plexus.
- The lumbar plexus (Figure 21.9A) is formed within the psoas muscle from the anterior rami of the L1-4 spinal nerves, with contribution from the 12th thoracic nerve (subcostal nerve). The most cephalad nerves of the plexus are the iliohypogastric, ilioinguinal, and genitofemoral. These nerves pierce the abdominal musculature anteriorly before supplying the skin of the hip, groin, and genital regions. The three caudal nerves of the lumber plexus are the lateral femoral cutaneous (LFC), femoral, and obturator.
- The LFC nerve passes under the lateral end of the inguinal ligament, supplying sensory innervation to the lateral thigh and buttock.
- The femoral nerve passes under the inguinal ligament just lateral to the femoral artery and vein, under the fascia iliaca, on the surface of the iliacus muscle. It supplies the muscles and skin of the anterior thigh as well as the knee and hip joints. From there, it courses with the femoral artery and vein through the adductor canal, an anatomic tunnel bounded by the fascial planes of the sartorius, the vastus medialis, and the adductor longus and magnus muscles. The nerve and vessels exit the canal at the adductor hiatus just above the medial femoral condyle. The saphenous nerve is the cutaneous termination of the nerve, supplying the skin of the medial leg and foot. It is the only nerve of the lumbar plexus that innervates below the knee (Figure 21.3).
- The obturator nerve exits from the pelvis through the obturator canal of the ischium, innervating the adductor muscles of the thigh, the hip and knee joints, and a portion of the skin of the medial thigh.
- The sacral plexus (Figure 21.9B) is formed from the anterior rami of the L4-5 nerves and the S1-3 nerves (lumbosacral trunk). The two major nerves of the sacral plexus are the sciatic nerve (SCN) and the posterior cutaneous nerve of the thigh (PCNT). Other branches of the sacral plexus are the pudendal, superior, and inferior gluteal nerves.
- The PCNT travels with the SCN in its proximal extent and supplies the skin of the posterior thigh, extending sometimes to the posterior calf.
- The SCN passes out of the pelvis through the greater sciatic foramen, becomes superficial at the lower border of the gluteus maximus, descends along the medial aspect of the femur supplying branches to the hamstrings, and becomes superficial again at the popliteal fossa, where it lies between the semimembranosus and semitendinosus muscles medially and biceps femoris muscle laterally. There, it divides into the tibial nerve and the common peroneal nerve.
- The tibial nerve travels down the posterior calf and passes under the medial malleolus before dividing into its terminal branches. It supplies the skin of the medial and plantar foot and causes plantar flexion (Figure 21.3).
- The common peroneal nerve winds around the head of the fibula before dividing into the superficial and deep peroneal nerves.
- The superficial peroneal nerve is a sensory nerve that passes down the lateral calf, dividing into its terminal branches just medial to the lateral malleolus, supplying the dorsal aspect of the foot (Figure 21.3).
- The deep peroneal nerve enters the foot just lateral to the anterior tibial artery, lying at the superior border of the malleolus, in between the anterior tibialis tendon and the extensor hallucis longus tendon. Although primarily a motor nerve causing dorsiflexion of the foot, it also sends a sensory branch to the web space between the first and second toes (Figure 21.3).
- The sural nerve is a sensory nerve formed from branches of the common peroneal and tibial nerves. It passes under the lateral malleolus, supplying the lateral foot (Figure 21.3).
- The lumbar plexus (Figure 21.9A) is formed within the psoas muscle from the anterior rami of the L1-4 spinal nerves, with contribution from the 12th thoracic nerve (subcostal nerve). The most cephalad nerves of the plexus are the iliohypogastric, ilioinguinal, and genitofemoral. These nerves pierce the abdominal musculature anteriorly before supplying the skin of the hip, groin, and genital regions. The three caudal nerves of the lumber plexus are the lateral femoral cutaneous (LFC), femoral, and obturator.
- Indications. Anesthetizing the entire lower extremity requires blocking components of both the lumbar and sacral plexuses.
- Innervation of the hip joint includes many nerves from both lumbar and sacral plexuses including genitofemoral, LFC, femoral, obturator, sciatic, superior cluneal, and superior gluteal nerves and the nerve to the quadratus femoris muscle. This complex innervation makes it difficult to find one single RA technique for hip surgery operation. However, the lumbar plexus block, femoral nerve block (including fascia iliaca block), SCN block, and periarticular injection techniques have been used for post–hip surgery pain control.
- An LFC nerve block provides excellent analgesia for skin graft donor sites on the anterior thigh. An isolated femoral nerve block is useful for providing postoperative analgesia for femoral shaft fractures as well as quadricepsplasty or repair of a patellar fracture.
- Knee joint innervation is also complex. Branches of the LFC, tibial, common peroneal, and obturator nerves as well as the nerves to the vastus lateralis and intermedius and femoral branches like the saphenous and medial femoral cutaneous nerves contribute to knee joint innervation. This complex innervation makes it difficult to find one single RA technique for open knee surgery. Blocks of the lumbar plexus, femoral nerve, SCN, and adductor canal and periarticular injection between the popliteal artery and posterior capsule of the knee (IPACK) have been used for postoperative analgesia for open knee surgeries.
- Operations distal to the knee can be performed under sciatic and saphenous nerve blocks.
- Complications specific to lower extremity blocks are common to all nerve blocks (see Section III).
- Techniques
- Lumbar plexus (psoas) block using UGRA (Figure 21.10): Place the patient in the lateral position, hips flexed, with the surgical side up. Place a curved array transducer in the transverse plane along the posterior axillary line above the iliac crest at the level of L2-4. Scan from medial to lateral and identify the TP, erector spinae muscle (ESM) superficial to the TP, psoas muscle (deep to the TP), and peritoneum, noting the depth of all structures. Identify the posterior one-third of the psoas muscle, where the lumbar plexus is located. The plexus itself may not be visualized inside the psoas muscle. Insert a 22-gauge 150-mm needle medial to the transducer and advance IP from medial to lateral until the needle tip lies in the posterior one-third of the psoas muscle. PNS is helpful for localization and will cause quadriceps contraction. After negative aspiration, inject 25 to 30 mL of LA. Complications specific to this block include epidural blockade with potential sympathectomy, vascular injury, perforated viscus, and renal injury.
Figure 21-10 Lumbar plexus (psoas)/quadratus lumborum block using ultrasound guidance.
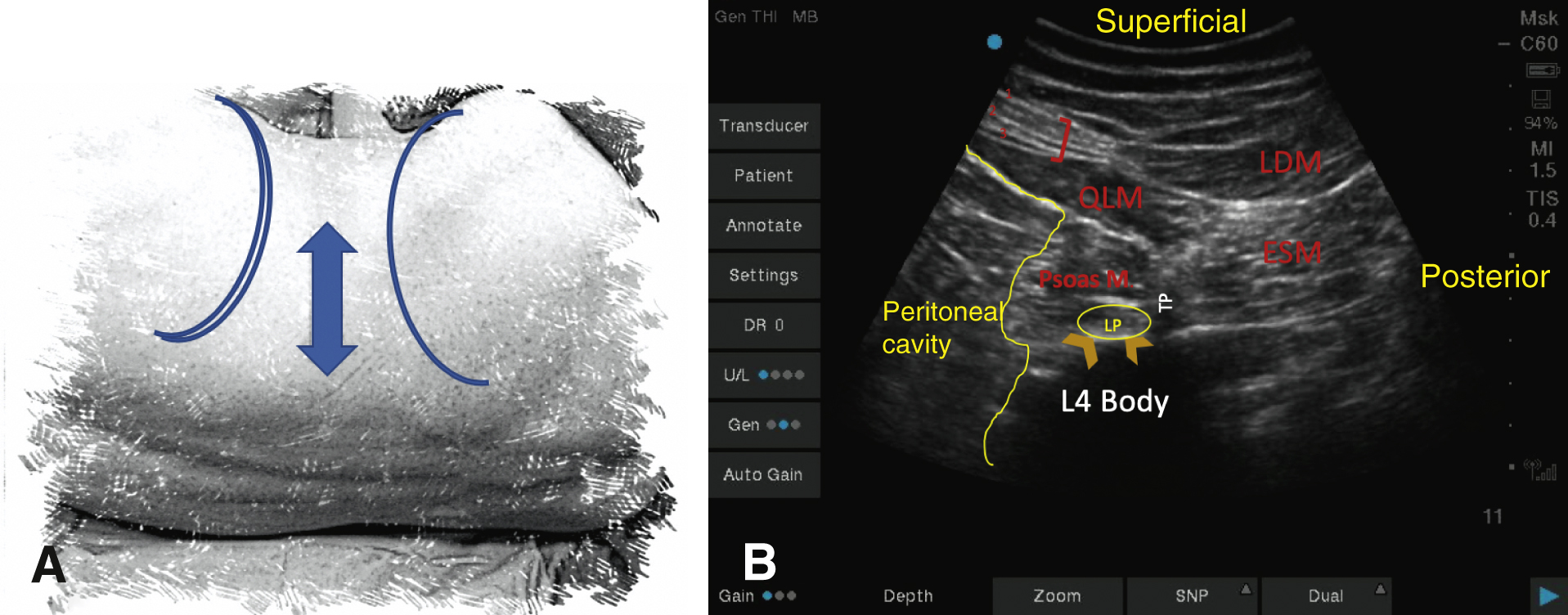
A, The two-sided arrow shows the placement of the US probe, between the iliac crest (one blue line) and costal margin (two blue lines). B, The red bracket delineates the three abdominal muscle layers (1: external oblique, 2: internal oblique, 3: transversus abdominis). The TP of the lumbar vertebra separates the psoas muscle from the ESM. The LP is embedded within the psoas muscle. ESM, erector spinae muscle; LDM, latissimus dorsi muscle; LP, lumbar plexus; QLM, quadratus lumborum muscle; TP, transverse process.
- LFC nerve
- LFC nerve block using landmark: Insert a 22-gauge 25-mm needle 1 to 2 cm caudal and medial to the anterior superior iliac spine (ASIS). Direct the needle in a slightly lateral and cephalad direction, striking the iliac bone medially just below the ASIS, and inject 5 to 10 mL of LA.
- LFC nerve block using UGRA: Place the probe inferior to the ASIS, parallel to the inguinal ligament. The LFC nerve is localized on the “fat pad” between the tensor fasciae lata and sartorius muscles. Insert a 22-gauge 25-mm needle with IP approach and inject 5 to 10 mL of LA around the nerve. Note that the nerve may pass through the sartorius muscle in up to 22% of the population.
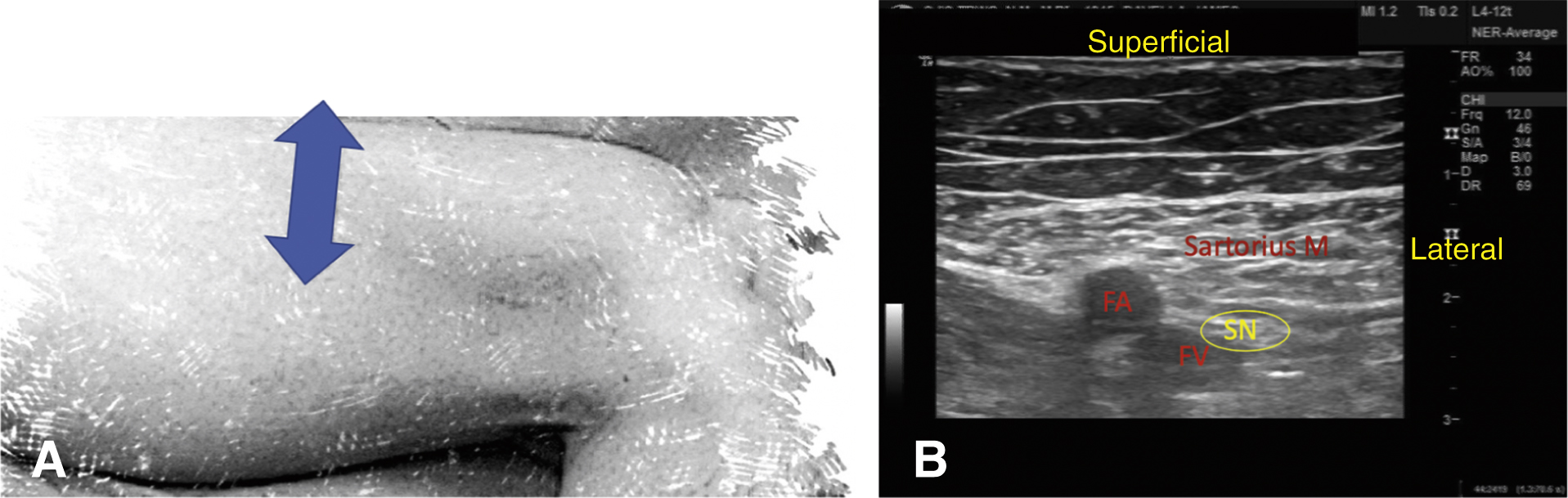
- Femoral nerve block using UGRA (Figure 21.11): With the patient supine, place the probe over the femoral artery at the level of the femoral crease and move approximately 1 cm laterally so that the artery is at the medial edge of the image. Two separate fascial layers can be visualized overlying the iliopsoas muscle: the superficial fascia lata and the deeper fascia iliaca. The nerve can be visualized just deep to the fascia iliaca and lateral to the artery. Insert a 22-gauge needle at least 50-mm in length and advance medially at a 60° angle to the skin using an IP approach. As the needle is advanced, two distinct “pops” are felt and seen as the two fascial layers are traversed. At this point, the needle tip should lie between the fascia iliaca and the iliopsoas muscle, on the lateral side of the nerve. If the needle is in the proper plane, with PNS a quadriceps twitch (patella dance) is elicited and LA spread is seen mostly in the horizontal direction, easily reaching the femoral nerve.
Figure 21-11 Femoral nerve/fascia iliaca block using ultrasound guidance.
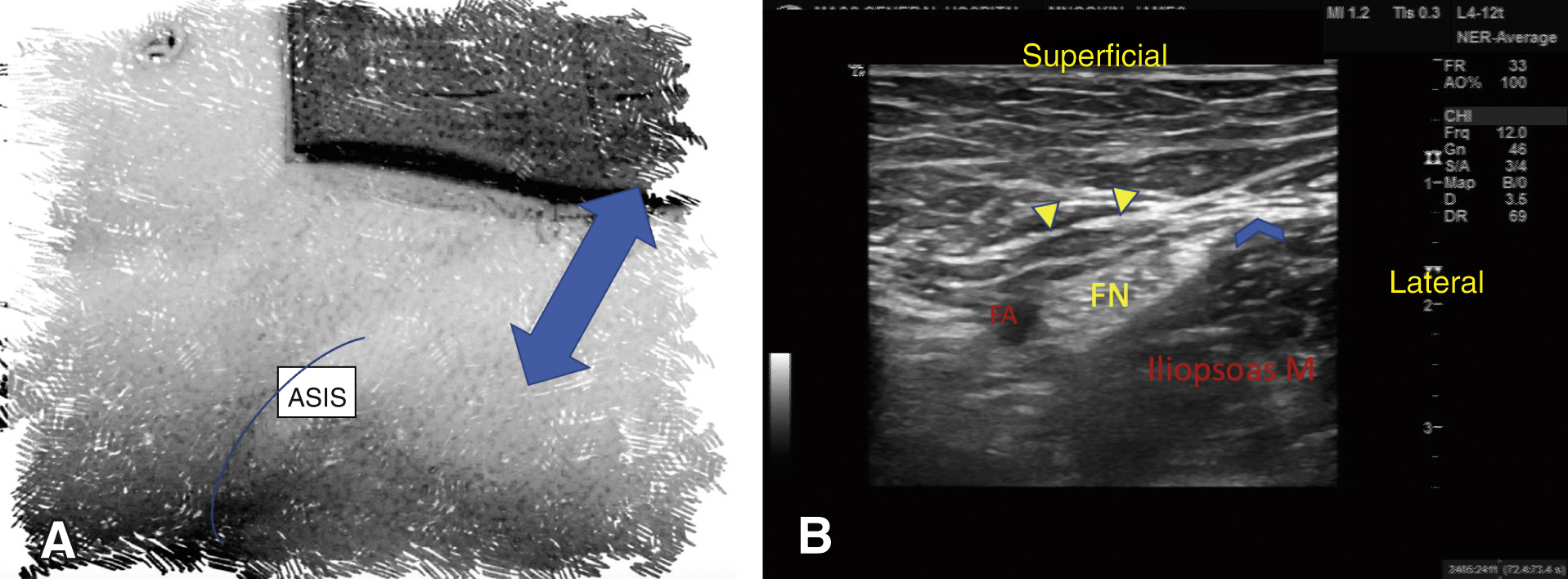
A, The two-sided arrow shows the placement of the US probe, parallel and caudad to the inguinal ligament. The blue lines show the iliac crest. B, The FN is located deep to the fascia lata (yellow arrows) and fascia iliaca (blue arrow) and lateral to the FA. ASIS, anterior superior iliac spine; FA, femoral artery; FN, femoral nerve.
- Fascia iliaca block using UGRA (Figure 21.11): This technique can block the LFC and femoral nerves. The approach is essentially the same as the femoral nerve block. Approximately 35 to 40 mL of diluted LA is injected at the lateral edge under the fascia iliaca and will spread medially toward the femoral nerve.
- Adductor canal block using UGRA (Figure 21.12;
 ): This block anesthetizes the terminal branches of the femoral nerve (saphenous nerve and nerve to the vastus medialis) and the branches of the obturator nerve at the level of the mid-thigh as they course through the adductor canal. Blocking the femoral nerve terminal branches here as opposed to at the inguinal crease has been shown to result in equivalent analgesia with potentially less motor blockade of the quadriceps. Place the patient in the supine position, with the operative leg externally rotated and slightly flexed at the knee. Scan with the ultrasound probe to identify the femoral artery deep to the sartorius at the medial aspect of the mid-thigh. The nerve bundles can be visualized as echo-dense structures lateral to the femoral artery. Insert a 22-gauge 80- to 100-mm needle lateral to the probe and advance toward the target structures. After negative aspiration, deposit a total of 15 to 20 mL of LA on each side of the femoral artery.
): This block anesthetizes the terminal branches of the femoral nerve (saphenous nerve and nerve to the vastus medialis) and the branches of the obturator nerve at the level of the mid-thigh as they course through the adductor canal. Blocking the femoral nerve terminal branches here as opposed to at the inguinal crease has been shown to result in equivalent analgesia with potentially less motor blockade of the quadriceps. Place the patient in the supine position, with the operative leg externally rotated and slightly flexed at the knee. Scan with the ultrasound probe to identify the femoral artery deep to the sartorius at the medial aspect of the mid-thigh. The nerve bundles can be visualized as echo-dense structures lateral to the femoral artery. Insert a 22-gauge 80- to 100-mm needle lateral to the probe and advance toward the target structures. After negative aspiration, deposit a total of 15 to 20 mL of LA on each side of the femoral artery. - Saphenous nerve block using UGRA: The adductor canal approach is used for saphenous nerve block at the level of the mid-thigh. For saphenous nerve block below the knee, position the patient supine with the leg straight. Place the probe at the level of the tibial tuberosity. Visualize the saphenous vein and fascia lata and inject LA around the saphenous nerve close to the saphenous vein. Using a tourniquet above the knee may help to engorge the saphenous vein.
- Obturator nerve block using UGRA: Position the patient supine. Place the transducer on the medial thigh just below the inguinal crease. Identify the anterior branch of the obturator nerve in the fascial plane between the adductor longus and brevis muscles. Identify the posterior branch in the fascial plane between the adductor brevis and magnus muscles. Advance a 22-gauge 80-mm needle with the IP or OOP approach until the tip lies in the appropriate fascial plane. PNS of the obturator nerve will elicit an adductor twitch. Inject 5 to 10 mL of LA around each branch (total of 10-20 mL).
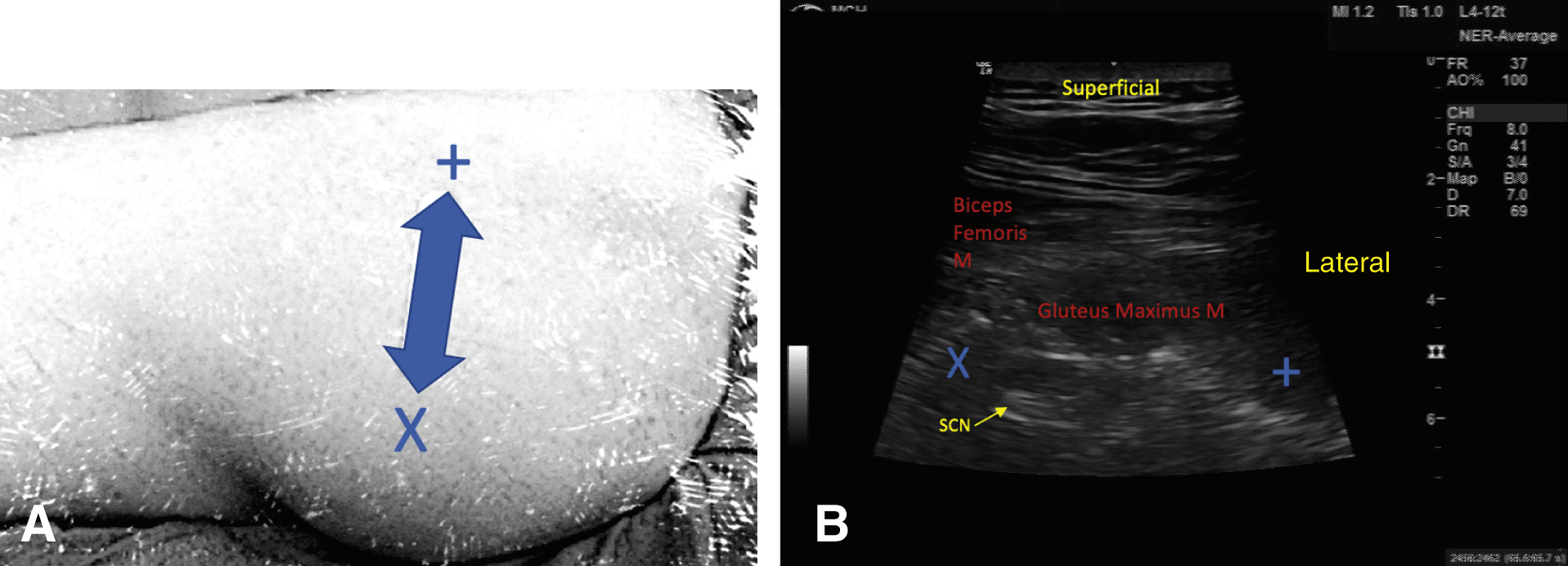
- SCN block
- Gluteal/subgluteal approach using UGRA: Place the patient in the Sims position, a lateral decubitus position with the leg to be blocked uppermost and flexed at the hip and knee. Place a curved transducer between the greater trochanter and ischial tuberosity. Visualize the hyperechoic SCN in the transverse plane at the level of the ischial spine, deep to the gluteus maximus muscle and superficial to the quadratus femoris muscle. Insert a 22-gauge 80- to 100-mm needle lateral to the transducer and advance in plane until the needle tip is in proximity to the nerve. PNS elicits a motor response in the SCN distribution (contraction of hamstring or gastrocnemius, foot dorsiflexion or plantar flexion) or paresthesia in the leg or foot. After negative aspiration, inject 15 to 25 mL of LA with the goal of circumferential spread around the nerve. In the subgluteal approach (Figure 21.13;
 ), the needle is inserted a few centimeters more distally where the gluteus maximus is thinner and the SCN is more superficial.
), the needle is inserted a few centimeters more distally where the gluteus maximus is thinner and the SCN is more superficial. - Popliteal approach using UGRA (Figure 21.14;
 ): This may be performed posteriorly with the patient in the prone, lateral, or supine position with the leg elevated. The linear or curved probe is placed at the level of the popliteal crease, and the popliteal artery should be seen in cross-section. The artery is then followed cephalad 5 to 7 cm. The popliteal vein classically lies superficial and lateral to the artery, and the SCN lies even more superficial and lateral to the vein. The semimembranosus muscle is seen medially and the biceps femoris is seen lateral to the nerve. The nerve should be traced to identify the site of bifurcation into the tibial and common peroneal nerves. With the SCN centered in the image and taking an IP approach, a needle insertion site is chosen approximately 1 cm lateral to the probe. Insert a 22-gauge 80-mm needle and advance the needle tip adjacent to the nerve at the point of bifurcation and between common peroneal and tibial nerves. A distinct pop is felt with entry into the perineural sheath. PNS causes foot dorsiflexion or plantar flexion and/or paresthesia in the leg or foot. After negative aspiration, inject 20 to 30 mL of LA to achieve circumferential spread around the nerve.
): This may be performed posteriorly with the patient in the prone, lateral, or supine position with the leg elevated. The linear or curved probe is placed at the level of the popliteal crease, and the popliteal artery should be seen in cross-section. The artery is then followed cephalad 5 to 7 cm. The popliteal vein classically lies superficial and lateral to the artery, and the SCN lies even more superficial and lateral to the vein. The semimembranosus muscle is seen medially and the biceps femoris is seen lateral to the nerve. The nerve should be traced to identify the site of bifurcation into the tibial and common peroneal nerves. With the SCN centered in the image and taking an IP approach, a needle insertion site is chosen approximately 1 cm lateral to the probe. Insert a 22-gauge 80-mm needle and advance the needle tip adjacent to the nerve at the point of bifurcation and between common peroneal and tibial nerves. A distinct pop is felt with entry into the perineural sheath. PNS causes foot dorsiflexion or plantar flexion and/or paresthesia in the leg or foot. After negative aspiration, inject 20 to 30 mL of LA to achieve circumferential spread around the nerve.Figure 21-14 Sciatic nerve block with popliteal fossa approach using ultrasound guidance.
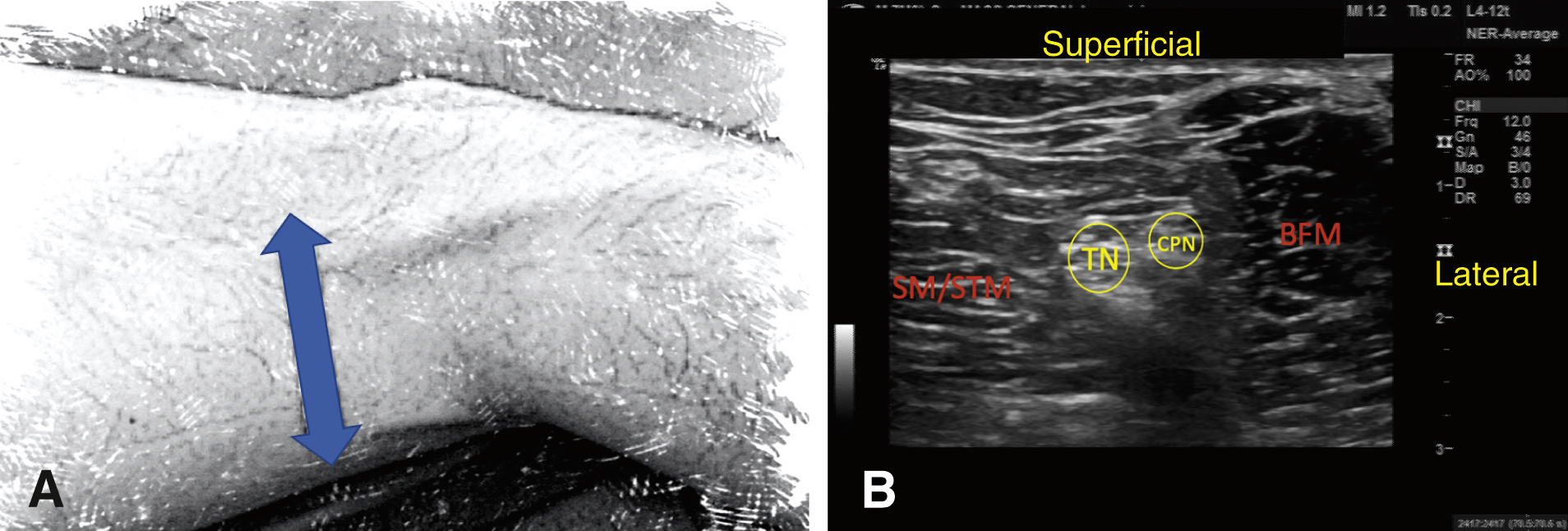
A, The two-sided arrow shows the placement of the US probe at the popliteal fossa. B, The SM/STM is seen medially, and the BFM is seen lateral to the sciatic nerve, which is composed of the TN and CPN. BFM, biceps femoris muscle; CPN, common peroneal nerve; SM, semimembranosus muscle; STM, semitendinosus muscle; TN, tibial nerve.
- Gluteal/subgluteal approach using UGRA: Place the patient in the Sims position, a lateral decubitus position with the leg to be blocked uppermost and flexed at the hip and knee. Place a curved transducer between the greater trochanter and ischial tuberosity. Visualize the hyperechoic SCN in the transverse plane at the level of the ischial spine, deep to the gluteus maximus muscle and superficial to the quadratus femoris muscle. Insert a 22-gauge 80- to 100-mm needle lateral to the transducer and advance in plane until the needle tip is in proximity to the nerve. PNS elicits a motor response in the SCN distribution (contraction of hamstring or gastrocnemius, foot dorsiflexion or plantar flexion) or paresthesia in the leg or foot. After negative aspiration, inject 15 to 25 mL of LA with the goal of circumferential spread around the nerve. In the subgluteal approach (Figure 21.13;
- Ankle block
The five nerves supplying the foot can be blocked at the ankle. These include two deep nerves (tibial and deep peroneal) and three superficial nerves (superficial peroneal, sural, saphenous) (Figure 21.15). The ankle block can be performed with the landmark technique or UGRA with a small linear high-frequency probe.
- At the superior border of the malleoli, the deep peroneal nerve is situated between the anterior tibialis tendon and the extensor hallucis longus tendon, which are easily palpable with dorsiflexion of the foot and extension of the great toe. Place the transducer transversely at the level of the extensor retinaculum on the anterior ankle and identify the nerve lateral to the anterior tibial artery. Insert a 25-mm needle just lateral to the anterior tibial artery while depositing 5 to 10 mL of LA close to the nerve.
Figure 21-15 Cross-section of anatomic structures at the level of the ankle.
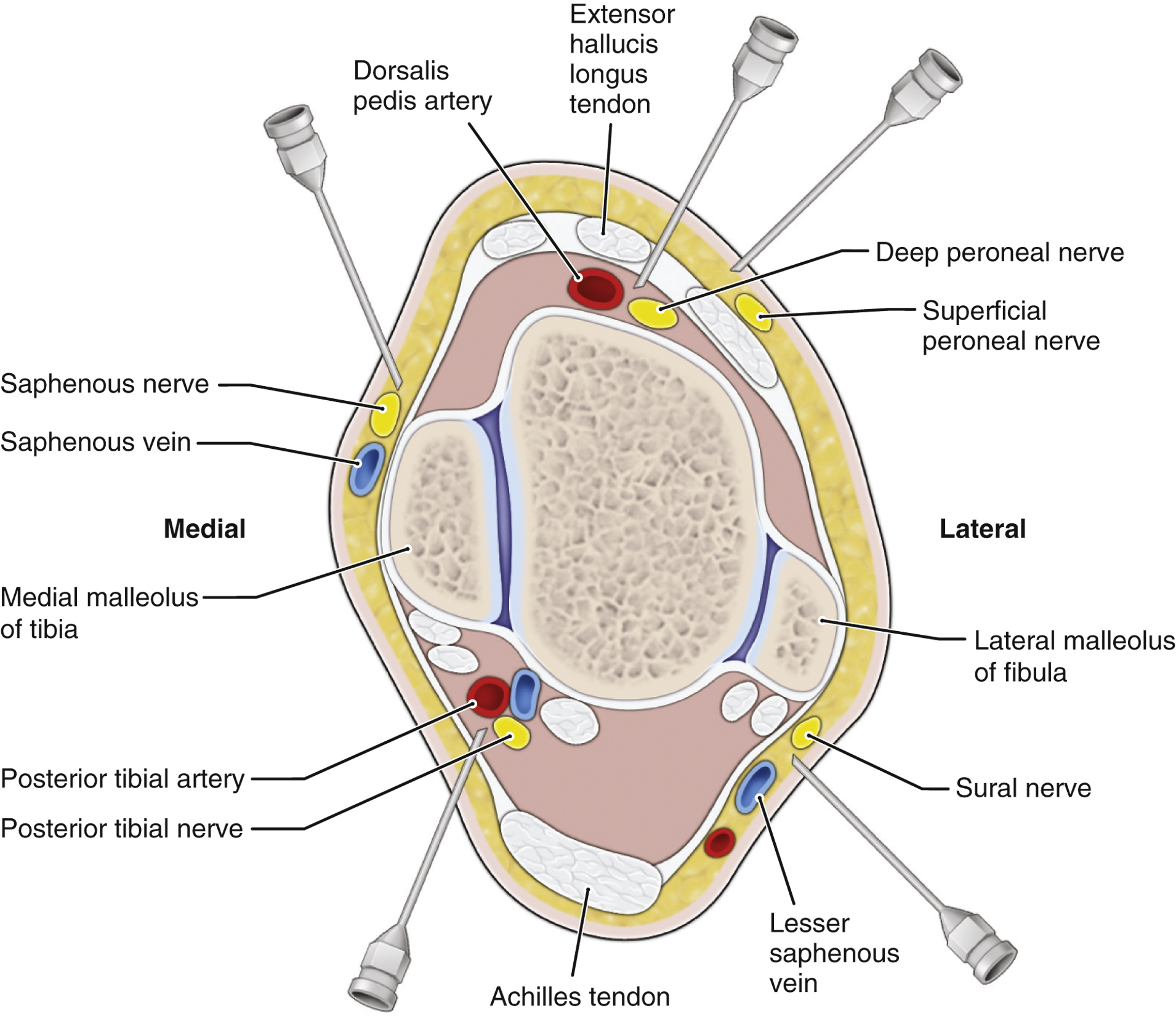
The deep peroneal nerve is located lateral to the extensor hallucis longus tendon and dorsalis pedis artery. The posterior tibial nerve is posterior to the distal medial malleolus and posterior tibial artery.
(From Horn JL, NasiriM. Regional blocks—A brief overview. In: JaffeRA, SchmiesingCA, GolianuB, eds. Anesthesiologist’s Manual of Surgical Procedures. 6th ed. 2020:1763-1799.)
- Block the superficial peroneal nerve by placing the transducer transversely 5 to 10 cm proximal and anterior to the lateral malleolus. Identify the nerve in the subcutaneous tissue superficial to the fascia. Alternatively, inject 10 mL of LA subcutaneously across the anterior surface of the tibia, from malleolus to malleolus. The latter approach will block the superficial peroneal nerve laterally and the saphenous nerve medially.
- To block the posterior tibial nerve, place the transducer transversely at the level of the medial malleolus and visualize the nerve posterior to the posterior tibial artery. Insert a needle OOP posterior to the medial malleolus, directed toward the posterior tibial nerve, and inject 5 to 10 mL of LA in a fan-shaped area.
- Block the sural nerve by placing the probe lateral and proximal to the lateral malleolus. Find the small saphenous vein, identify the nerve superficial to the deep fascia and adjacent to the saphenous vein, and inject 5 mL of LA.
- At the superior border of the malleoli, the deep peroneal nerve is situated between the anterior tibialis tendon and the extensor hallucis longus tendon, which are easily palpable with dorsiflexion of the foot and extension of the great toe. Place the transducer transversely at the level of the extensor retinaculum on the anterior ankle and identify the nerve lateral to the anterior tibial artery. Insert a 25-mm needle just lateral to the anterior tibial artery while depositing 5 to 10 mL of LA close to the nerve.
- Lumbar plexus (psoas) block using UGRA (Figure 21.10): Place the patient in the lateral position, hips flexed, with the surgical side up. Place a curved array transducer in the transverse plane along the posterior axillary line above the iliac crest at the level of L2-4. Scan from medial to lateral and identify the TP, erector spinae muscle (ESM) superficial to the TP, psoas muscle (deep to the TP), and peritoneum, noting the depth of all structures. Identify the posterior one-third of the psoas muscle, where the lumbar plexus is located. The plexus itself may not be visualized inside the psoas muscle. Insert a 22-gauge 150-mm needle medial to the transducer and advance IP from medial to lateral until the needle tip lies in the posterior one-third of the psoas muscle. PNS is helpful for localization and will cause quadriceps contraction. After negative aspiration, inject 25 to 30 mL of LA. Complications specific to this block include epidural blockade with potential sympathectomy, vascular injury, perforated viscus, and renal injury.