Key Clinical Updates in Benign Prostatic Hypertrophy A 5-year multi-center clinical trial of aquablation shows significant and sustained improvements in urinary flow rate, postvoid residual volume, and quality of life. Zorn KC et al. BJUI Compass. [PMID: 35474721] A double-blind, randomized, sham-controlled study of the Optilume BPH catheter system showed improvement in flow rate, post-void residual, and patient satisfaction scores that were sustained at 1 year. Treatment was limited to prostates ranging in size from 20 mL to 80 mL and long-term benefit has yet to be proven. Kaplan SA et al. J Urol. [PMID: 37555604] |
| ESSENTIALS OF DIAGNOSIS | ||
|
General Considerations
Benign prostatic hyperplasia (BPH) is extremely common, and its incidence rises with increasing age. Autopsy studies have shown histologically proven BPH in 60% of men aged 60 and 80% of men aged 80. Bothersome urinary symptoms related to BPH also increase with age, although it is important to note that these symptoms can occur without significant enlargement on exam. Obstructive voiding symptoms are reported by approximately 25% of men aged 55 and 50% of men aged 75. It is critical for the clinician to discriminate between "obstructive" and "irritative" symptoms to target the root cause of that patient's bother. This may be related to prostatic enlargement, high smooth muscle tone at the bladder neck or prostatic urethra, or underlying detrusor overactivity, which all require specific treatments.
Risk factors for the development of BPH are poorly understood. Some studies have suggested a genetic predisposition and some have noted racial differences. Approximately 50% of men under age 60 years who undergo surgery for BPH may have a heritable form of the disease. This form is most likely an autosomal dominant trait, and first-degree male relatives of such patients carry an increased relative risk of approximately fourfold.
Etiology
Lower urinary tract symptoms result from the complex interplay of a dynamic system and are often multifactorial. Benign prostatic enlargement is a common component of this symptom complex. The prostate is composed of both stromal and epithelial elements, and each, either alone or in combination, can give rise to hyperplastic nodules and the symptoms associated with BPH. Each element may be targeted in medical management schemes.
Laboratory and clinical studies have identified two necessary factors for development of BPH: the effect of endocrine compounds (eg, dihydrotestosterone [DHT]) on prostate growth, and the impact of aging. The main mechanism of action seems to be stromal-epithelial interactions (stromal cells regulating growth of epithelial cells or other stromal cells by paracrine or autocrine signaling or by secreting growth factors such as basic fibroblast growth factor or transforming growth factor beta). Studies have also demonstrated that BPH is under endocrine control and that castration results in the regression of established disease and improvement in urinary symptoms. Administration of a luteinizing hormone-releasing hormone (LHRH) analog in men reversibly shrinks established BPH, resulting in objective improvement in urinary flow rate and subjective improvement in symptoms.
Pathology
BPH is truly a hyperplastic process, resulting from an increase in cell numbers. Microscopic evaluation reveals a nodular growth pattern consisting of stroma or epithelium. Stroma is composed of varying amounts of collagen and smooth muscle. The differential representation of various histologic components of BPH in part explains the potential variable responsiveness to medical therapy. Thus, alpha-blocker therapy may result in excellent responses in patients with BPH when there is a significant component of smooth muscle, while hyperplasia composed predominantly of epithelium might respond better to 5-alpha-reductase inhibitors. Patients with significant components of collagen in the stroma may not respond to either form of medical therapy. Responsiveness to specific therapy cannot be predicted reliably.
As BPH nodules in the transition zone enlarge, they compress the prostatic urethral lumen, leading to bladder outlet obstruction and its characteristic urinary symptoms of weak stream, frequency, urgency, and nocturia. Transition zone enlargement also compresses the outer zones of the prostate, resulting in the formation of a "surgical capsule." This boundary separates the transition zone from the peripheral zone of the gland and serves as a cleavage plane for enucleation of the prostate during simple prostatectomy (robotic or open surgery that removes the zone of the prostate around the urethra leaving the peripheral portion of the prostate and prostate capsule) or during Holmium Laser Enucleation of the Prostate (HoLEP).
Pathophysiology
The symptoms of BPH can be related either to the obstructive component of the prostate or to the secondary response of the bladder to the outlet resistance. The obstructive component can be subdivided into mechanical obstruction and dynamic obstruction.
As prostatic enlargement occurs, mechanical obstruction may result from intrusion into the urethral lumen or bladder neck, resulting in a higher bladder outlet resistance. However, prostatic size on DRE correlates poorly with symptoms.
The dynamic component of prostatic obstruction explains the variable nature of the symptoms. The prostatic stroma is composed of smooth muscle and collagen and is rich in adrenergic nerve supply. The level of autonomic stimulation thus sets a "tone" to the prostatic urethra. Alpha-blocker therapy decreases this tone, resulting in a decrease in outlet resistance.
The irritative voiding complaints of BPH result from the secondary response of the bladder to the increased outlet resistance. Bladder outlet obstruction results in detrusor muscle hypertrophy and hyperplasia as well as collagen deposition. The latter is most likely responsible for a decrease in bladder compliance, but detrusor instability also occurs. On gross inspection, thickened detrusor muscle bundles are seen as trabeculations on cystoscopic examination. If left unchecked, mucosal herniation between detrusor muscle bundles ensues, resulting in diverticulum formation ("false" diverticula composed of mucosa and serosa only).
Clinical Findings
A. Symptoms
The symptoms of BPH can be divided into obstructive and irritative complaints. Obstructive symptoms include hesitancy, decreased force and caliber of the stream, sensation of incomplete bladder emptying, double voiding (urinating a second time within minutes), straining to urinate, and postvoid dribbling. Irritative symptoms include urgency, dysuria, frequency, and nocturia.
The American Urological Association (AUA) symptom index (Table 25-4. American Urological Association Symptom Index for Benign Prostatic Hyperplasia) is an important tool used in the evaluation of patients with this disorder and should be calculated for all patients before starting therapy. The answers to seven questions quantitate the severity of obstructive or irritative complaints on a scale of 0-5. Thus, the score can range from 0 to 35 with increasing severity of symptoms. An estimation of postvoid residual can provide important information on bladder emptying and the need for more urgent intervention.
Table 25-4. American Urological Association symptom index for benign prostatic hyperplasia.1Questions to Be Answered | Not at All | Less Than One Time in Five | Less Than Half the Time | About Half the Time | More Than Half the Time | Almost Always |
|---|---|---|---|---|---|---|
1. Over the past month, how often have you had a sensation of not emptying your bladder completely after you finish urinating? | 0 | 1 | 2 | 3 | 4 | 5 |
2. Over the past month, how often have you had to urinate again less than 2 hours after you finished urinating? | 0 | 1 | 2 | 3 | 4 | 5 |
3. Over the past month, how often have you found you stopped and started again several times when you urinated? | 0 | 1 | 2 | 3 | 4 | 5 |
4. Over the past month, how often have you found it difficult to postpone urination? | 0 | 1 | 2 | 3 | 4 | 5 |
5. Over the past month, how often have you had a weak urinary stream? | 0 | 1 | 2 | 3 | 4 | 5 |
6. Over the past month, how often have you had to push or strain to begin urination? | 0 | 1 | 2 | 3 | 4 | 5 |
7. Over the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning? | 0 | 1 | 2 | 3 | 4 | 5 |
1 Sum of seven circled numbers equals the symptom score. See text for explanation.
Reproduced, with permission, from Barry MJ et al; Measurement Committee of the American Urological Association. The American Urological Association symptom index for benign prostatic hyperplasia. J Urol. 2017;197(2S):S189-97.
A detailed history focusing on the urinary tract should be obtained to exclude other possible causes of symptoms such as prostate cancer, urinary tract infection, neurogenic bladder, or urethral stricture. A focused medical history may also reveal other comorbidities that can directly affect urinary symptoms such as metabolic syndrome, heart failure, Parkinson disease, and obstructive sleep apnea.
B. Signs
A physical examination, digital rectal examination (DRE), and a focused neurologic examination should be performed on all patients. The size and consistency of the prostate should be noted. While prostate size does not correlate perfectly with the severity of symptoms or the degree of obstruction, it can inform treatment decisions. BPH usually results in a smooth, firm, elastic enlargement of the prostate. Induration, if detected, must alert the clinician to the possibility of cancer, and further evaluation is needed (ie, prostate-specific antigen [PSA] testing, transrectal ultrasound, and biopsy). Examination of the lower abdomen may reveal a distended bladder.
C. Laboratory Findings
UA should be performed to exclude infection or hematuria. Clinicians should consider obtaining a serum PSA test in patients within the screening age range.
D. Imaging
Urologists are advised to consider prostate volume assessment prior to surgical intervention to determine the most appropriate approach (eg, water vapor therapy for smaller glands vs simple prostatectomy for a very large gland). This assessment can be done with cystoscopy; transrectal or abdominal ultrasound; or cross-sectional imaging of the pelvis, if it is available.
E. Cystoscopy
Cystoscopy is not required to determine the need for treatment but may assist in determining the best approach in patients opting for surgical therapy.
F. Additional Tests
Uroflowmetry and postvoid residual should be assessed prior to surgical treatment of the prostate and can be useful in tracking response to treatments. Cystometrograms and urodynamic profiles should be reserved for patients with unclear etiology of symptoms, suspected neurologic disease, or those who have not responded to previous prostate surgery.
Differential Diagnosis
A history of prior urethral instrumentation, urethritis, sexually transmitted infections, or trauma should be elucidated to exclude urethral stricture or bladder neck contracture. Hematuria and pain are commonly associated with bladder stones. Carcinoma of the prostate may be detected by abnormalities on DRE or an elevated PSA (see Part 41). A urinary tract infection can mimic the irritative symptoms of BPH and can be readily identified by UA and culture; however, a urinary tract infection can also be a complication of BPH. Carcinoma of the bladder, especially carcinoma in situ, may also present with irritative voiding complaints; however, UA usually shows evidence of hematuria (see Part 41). Patients with a neurogenic bladder may also have many of the same symptoms and signs as those with BPH; however, a history of neurologic disease, stroke, diabetes mellitus, or back injury may be obtained, and diminished perineal or lower extremity sensation or alterations in rectal sphincter tone or in the bulbocavernosus reflex might be observed on examination. Simultaneous alterations in bowel function (constipation) might also suggest the possibility of a neurologic disorder. Urodynamics studies can distinguish between neurogenic etiologies and obstructive etiologies for poor bladder emptying.
Treatment
Clinical practice guidelines exist for the evaluation and treatment of patients with BPH. Following the evaluation as outlined above, patients may be offered various forms of therapy for BPH. Patients are advised to consult with their primary care clinicians or urologists to make an educated decision on the basis of the relative efficacy and side effects of the treatment options (Table 25-5. Summary of Benign Prostatic Hyperplasia Treatment Outcomes (Listed in Alphabetical Order). ).
Table 25-5. Summary of benign prostatic hyperplasia treatment outcomes1 (listed in alphabetical order).Outcome | Rezum | TUIP | Open Surgery | TURP | Watchful Waiting | Alpha-Blockers | Finasteride2 |
|---|---|---|---|---|---|---|---|
Chance for improvement1 | - | 78-83% | 94-99.8% | 75-96% | 31-55% | 59-86% | 54-78% |
Death within 30-90 days1 | 0% | 0.2-1.5% | 1-4.6% | 0.5-3.3% | 0.8% | 0.8% | 0.8% |
Degree of symptom improvement (% reduction in symptom score) | 47% | 73% | 79% | 85% | Unknown | 51% | 31% |
Erectile dysfunction1 | 0% | 3.9-24.5% | 4.7-39.2% | 3.3-34.8% | 3% | 3% | 2.5-5.3% |
Hospital stay in days | 0% | 1-3 | 5-10 | 3-5 | 0 | 0 | 0 |
Loss of work in days | - | 7-21 | 21-28 | 7-21 | 1 | 3.5 | 1.5 |
Morbidity and complications1 | 3.7-16.9% | 2.2-33.3% | 7-42.7% | 5.2-30.7% | 1-5% | 2.9-43.3% | 8.8-13.6% |
Need for operative treatment for surgical complications1 | <2% | 1.3-2.7% | 0.6-14.1% | 0.7-10.1% | 0 | 0 | 0 |
Retrograde ejaculation | 3-6% | 6-55% | 36-95% | 25-99% | 0 | 4-11% | 0 |
Total incontinence1 | 0% | 0.1-1.1% | 0.3-0.7% | 0.7-1.4% | 2% | 2% | 2% |
2 Most of the data reviewed for finasteride are derived from three trials that have required an enlarged prostate for entry. The chance of improvement in men with symptoms yet minimally enlarged prostates may be much less, as noted from the VA Cooperative Trial.
TUIP, transurethral incision of the prostate; TURP, transurethral resection of the prostate.
Patients with mild symptoms (AUA scores 0-7) and relatively low bother scores may be managed by watchful waiting only. Medical therapy is appropriate for those with significant bother attributed to their symptoms, but minimally invasive surgical treatments are also a first-line option for appropriately counseled patients. Absolute surgical indications include any of the following sequelae of BPH: recurrent urinary tract infection, problematic gross hematuria, bladder stones, refractory urinary retention (failing at least one attempt at catheter removal), or obstructive nephropathy.
A. Watchful Waiting
The risk of progression or complications is uncertain. However, men with progressive symptoms and large prostates do have a higher chance of developing urinary retention or requiring surgical intervention in the future.
Retrospective studies on the natural history of BPH are inherently subject to bias, relating in part to patient selection and to the type and extent of follow-up. Very few prospective studies addressing its natural history have been reported. One small series demonstrated that approximately 10% of symptomatic men may progress to urinary retention while 50% of patients demonstrate improvement or even resolution of symptoms. A large randomized study compared finasteride with placebo in men with moderate to severely symptomatic disease and enlarged prostates on DRE. Patients in the placebo arm demonstrated a 7% risk of developing urinary retention over 4 years.
Men with moderate or severe symptoms can also be observed if they so choose. The optimal interval for follow-up is patient-specific.
B. Medical Therapy
1. Alpha-Blockers
The human prostate and bladder base contains alpha-1-adrenoceptors, which show a contractile response to agonists. Blocking these receptors leads to smooth muscle relaxation and reduced resistance at the bladder outlet. Alpha-blockade has been shown to result in both objective and subjective degrees of improvement in the symptoms and signs of BPH. Alpha-blockers can be classified according to their receptor selectivity (Table 25-6. Alpha-Blockade Agent Treatment for Benign Prostatic Hyperplasia (Listed in Alphabetical Order). ) as well as their half-life.
Table 25-6. Alpha-blockade agent treatment for benign prostatic hyperplasia (listed in alphabetical order).Agent | Action | Oral Dose |
|---|---|---|
Alfuzosin | Alpha-1a-blockade | 10 mg daily |
Doxazosin | Alpha-1-blockade | 1-8 mg daily |
Prazosin | Alpha-1-blockade | 1-5 mg twice daily |
Silodosin (not available in the United States) | Alpha-1a-blockade | 4 or 8 mg daily |
Tadalafil | Phosphodiesterase type 5 inhibitor | 5 mg daily |
Tamsulosin | Alpha-1a-blockade | 0.4 or 0.8 mg daily |
Terazosin | Alpha-1-blockade | 1-10 mg daily |
Prazosin is a short-acting, nonselective alpha-blocker. Due to its short half-life and high side-effect profile (orthostatic hypotension, dizziness, tiredness, retrograde ejaculation, rhinitis, and headache), it is not typically used in the treatment of BPH.
Long-acting, nonselective alpha-blockers allow for once-a-day dosing, but dose titration is still necessary because side effects similar to those seen with prazosin may occur. Terazosin improves symptoms and in numerous studies it is superior to placebo or finasteride. Terazosin is started at a dosage of 1 mg orally daily for 3 days, increased to 2 mg orally daily for 11 days, then 5 mg orally daily. Additional dose escalation to 10 mg orally daily can be performed if necessary. Doxazosin is started at a dosage of 1 mg orally daily for 7 days, increased to 2 mg orally daily for 7 days, then 4 mg orally daily. Additional dose escalation to 8 mg orally daily can be performed if necessary.
Alpha-1a-receptors are localized to the prostate and bladder neck. Selective blockade of these receptors results in fewer systemic side effects than nonselective alpha-blocker therapy thus obviating the need for dose titration. The typical dose of tamsulosin is 0.4 mg orally daily taken 30 minutes after a meal. Alfuzosin is a long-acting alpha-1a-blocker; its dose is 10 mg orally once daily with food, and it does not require titration. Several randomized, double-blind, placebo-controlled trials have been performed comparing terazosin, doxazosin, tamsulosin, and alfuzosin with placebo. All agents have demonstrated safety and efficacy. Floppy iris syndrome, a complication of cataract surgery, can occur in patients taking both nonselective alpha-blockers and alpha-1a-blockers well after cessation of therapy.
2. 5-Alpha-Reductase Inhibitors
Finasteride and dutasteride block the conversion of testosterone to dihydrotestosterone. These medications impact the epithelial component of the prostate, resulting in reduction in size of the gland and improvement in symptoms. Six months of therapy are required for maximum effects on prostate size (20-30% reduction) and symptomatic improvement.
Several randomized, double-blind, placebo-controlled trials have been performed comparing finasteride with placebo. Efficacy, safety, and durability are well established. However, symptomatic improvement is seen only in men with enlarged prostates (greater than 40 mL by ultrasonographic examination). Side effects include decreased libido, decrease in volume of ejaculate, and erectile dysfunction. Serum PSA is reduced by approximately 50% in patients receiving finasteride therapy, but the % free PSA is unchanged. Therefore, in order to compare with pre-finasteride PSA levels, the serum PSA of a patient taking finasteride should be doubled.
Studies have shown that finasteride therapy decreases the incidence of urinary retention and the need for operative treatment in men with enlarged prostates and moderate to severe symptoms. The larger the prostate over 40 mL, the greater the relative-risk reduction. Dutasteride is a nonselective 5-alpha-reductase inhibitor (5ARI) that appears to be similar to finasteride in its effectiveness; it is dosed at 0.5 mg orally daily.
Both 5ARIs have been shown to be effective chemopreventive agents for prostate cancer in large, randomized clinical trials. A 25% risk reduction was observed in men with both low and high risk for prostate cancer. However, despite the strength of the evidence for 5ARIs in reducing the risk of prostate cancer, an FDA advisory committee recommended against labeling these agents for prostate cancer chemoprevention, citing the potential increased risk of high-grade cancers in these studies (1.8% vs 1.0% for finasteride and 1% vs 0.5% for dutasteride), isolated risk reduction in low-grade cancers, and inability to apply the findings to the general population. Moreover, the FDA has included the increased risk of being diagnosed with high-grade prostate cancer in the labels of all 5ARIs.
3. Phosphodiesterase-5 Inhibitor
Tadalafil is approved by the FDA to treat the symptoms and signs of BPH (Table 25-6. Alpha-Blockade Agent Treatment for Benign Prostatic Hyperplasia (Listed in Alphabetical Order). ); it is also approved for first-line use in men with both urinary symptoms and erectile dysfunction. The data from two randomized, double-blind, placebo-controlled trials demonstrated significant improvements in standardized measurements of urinary function between 2 and 4 weeks after initiating treatment at 5 mg once daily, with minimal adverse effects.
4. Combination Therapy
The Medical Therapy of Prostatic Symptoms (MTOPS) trial was a large, randomized, placebo-controlled trial comparing finasteride, doxazosin, the combination of the two, and placebo in 3047 men observed for a mean of 4.5 years. Long-term combination therapy with doxazosin and finasteride was safe and reduced the risk of overall clinical progression of BPH significantly more than did treatment with either medication alone. Combination therapy and finasteride alone reduced the long-term risk of acute urinary retention and the need for invasive therapy. Combination therapy also entailed the risks of additional side effects and the cost of two medications.
5. Phytotherapy
Phytotherapy is the use of plants or plant extracts for medicinal purposes. Several plant extracts have been popularized, including the saw palmetto berry, the bark of Pygeum africanum, the roots of Echinacea purpurea and Hypoxis hemerocallidea, pollen extract, and the leaves of the trembling poplar. However, a prospective, randomized, double-blind, placebo-controlled trial revealed no improvement in symptoms, urinary flow rate, or quality of life for men with BPH with saw palmetto treatment compared with placebo. Importantly, no significant adverse events were reported and some patients do note a subjective improvement in symptoms.
C. Transurethral Surgical Therapy
Most cases of BPH requiring surgery can be managed with transurethral or minimally invasive techniques. This remains an area of active research and innovation with several new technologies available. An overview of all the surgical options and decision making was published by the American Urological Association (Figure 25-3). Studies have shown decreased cost with surgical compared to medical therapies in as short as 6 months and as long as 8 years.
Figure 25-3. Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia
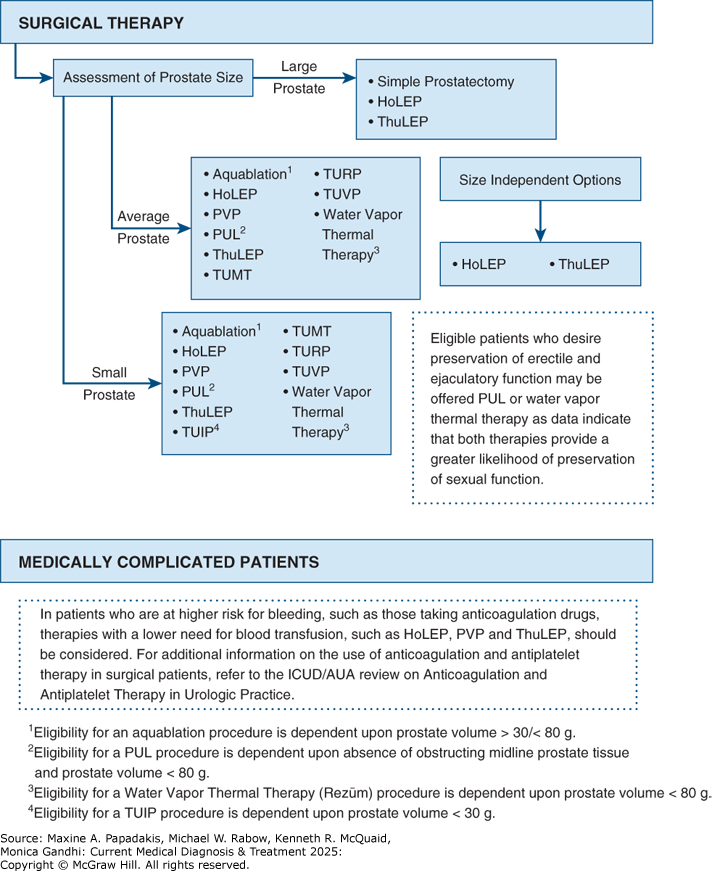
Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia. HoLEP, holmium laser enucleation of the prostate; PUL, prostatic urethral lift; PVP, photoselective vaporization of the prostate; ThuLEP, thulium laser enucleation of the prostate; TUIP, transurethral incision of the prostate; TUMT, transurethral microwave therapy; TURP, transurethral resection of the prostate; TUVP, transurethral vaporization of the prostate. (Reproduced with permission from Foster HE, Dahm P, Kohler TS, et al. Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA Guideline Amendment 2019. J Urol. 2019;202(3):592-598.)
1. Transurethral Resection of the Prostate (Turp)
Over 95% of prostate surgeries can be performed endoscopically (through the urethra). TURP is the gold standard treatment for surgical treatment of BPH, and it often requires a 1- to 2-day hospital stay. Most head-to-head surgical studies comparing TURP to minimally invasive therapies show that symptom scores and flow rate improvements are superior following TURP compared with other minimally invasive therapies. It is one of the most durable treatments available, with patients remaining symptom-free for an average of 5-10 years. The risks of TURP include retrograde ejaculation (75%), erectile dysfunction (5-10%), and urinary incontinence (less than 1%). Potential complications include (1) bleeding; (2) urethral stricture or bladder neck contracture; (3) perforation of the prostate capsule with extravasation; and (4) transurethral resection syndrome, a hypervolemic, hyponatremic state resulting from absorption of the hypotonic irrigating solution. Clinical manifestations of the syndrome include nausea, vomiting, confusion, hypertension, bradycardia, and visual disturbances. The risk of transurethral resection syndrome increases with monopolar resection times over 90 minutes. Treatment includes diuresis and, in severe cases, hypertonic saline administration (see Hyponatremia, Part 23). This syndrome was much more prevalent when TURPs were most often performed with monopolar electrocautery but, with the increased use of bi-polar TURPs (using saline irrigation), it is now very rare.
2. Transurethral Incision of the Prostate (Tuip)
Men with moderate to severe symptoms and small prostates (less than 30 g) often have posterior commissure hyperplasia or an "elevated bladder neck." These patients will often benefit from incision of the prostate. The procedure is more rapid and less morbid than TURP. Outcomes in well-selected patients are comparable, though a lower rate of retrograde ejaculation has been reported (25%).
3. Transurethral Electrovaporization of the Prostate (Tuvp)
TUVP is a technical electrosurgical modification of the standard TURP. A variety of energy delivery surfaces including a spherical rolling electrode (rollerball), grooved roller electrode (vaportrode), or hemispherical mushroom electrode (button) are used to deliver high current densities resulting in heat vaporization of prostatic tissue. The device requires slower sweeping speeds over the prostatic urethra, and the depth of vaporization is approximately one-third that of a standard loop. For larger prostates, this procedure usually takes longer than a standard TURP, but it has comparable efficacy with lower transfusion requirements.
4. Aquablation
This ultrasound-guided, robot-executed waterjet ablation of the prostate is designed to relieve prostatic obstruction with limited bleeding, shorter operative time, and preservation of sexual function. It is one of the few size-agnostic transurethral surgical options for BPH and has been shown to effectively treat glands ranging in size from 30 to 150 mL. Urinary outcomes have been shown to be comparable to the gold standard TURP with lower risk of stricture, incontinence, and sexual dysfunction. Pretreatment transrectal ultrasound is used to map out the obstructive adenoma to be ablated, while excluding the ejaculatory ducts. Real-time transrectal ultrasound is then used to monitor tissue resection during the procedure. The resection is performed under general or spinal anesthesia using a heat-free water jet from a transurethrally placed robotic handpiece with simultaneous suction of ablation tissue through the device. Following the resection, electrocautery or traction from a three-way catheter is used to obtain hemostasis. A 5-year multicenter clinical trial shows significant and sustained improvements in urinary flow rate, postvoid residual volume, and quality of life.
D. Minimally Invasive Therapies
1. Laser Therapy
Various laser technologies now exist and vary by wavelength, energy produced, and the technique of tissue removal, but all ultimately result in vaporization of tissue with simultaneous coagulation of small blood vessels. The laser fiber is advanced through the cystoscope, and the prostate tissue is systematically vaporized to create a capacious outlet passage. An immediate defect is obtained in the prostatic urethra, similar to that seen during TURP. Advantages to such laser therapy include minimal blood loss, rare occurrence of transurethral resection syndrome, ability to treat patients on anticoagulant therapy, and ability to operate on outpatients. Disadvantages are the lack of tissue for pathologic examination, variable effectiveness, more frequent irritative voiding complaints with certain lasers, and expense of laser fibers and generators.
Holmium laser enucleation of the prostate (HoLEP) is a technique of enucleating the adenomatous lobes intact and morcellating the tissue within the bladder. Advantages of HoLEP compared with other methods include ability to treat all prostate sizes, low re-treatment rates, few complications, and shorter duration of bladder catheterization. This technique is an attractive alternative to open simple prostatectomy for very large glands (greater than 100 mL) with comparable outcomes. However, due to the steep learning curve for operators, it is not as widely available as other techniques.
Photovaporization of the prostate (PVP) is a more widely adopted technique that can be performed with a number of different lasers depending on surgeon preference. The original KTP greenlight laser used a 532-nm wavelength that is selectively absorbed by hemoglobin, leading to improved hemostasis. Advantages include combined vaporization and coagulation with significant reduction in tissue volume, making this an ideal choice for anticoagulated patients. Disadvantages include limitations on prostate volume that can be efficiently treated (less than 80 mL) and difficulty controlling bleeding from larger venous channels.
Thulium laser enucleation of the prostate (ThuLEP) uses a continuous wave of 2013-nm energy that undergoes absorption in the irrigant but without the intermittent nature of holmium. This results in cleaner incisions, more efficient tissue absorption, and similar hemostatic advantages. Thulium laser has also been used for resection-type techniques with success. Advantages and disadvantages are similar to greenlight PVP, though the cleaner incisions make it more appealing for surgeons.
2. Transurethral Microwave Therapy (Tumt)
Microwave hyperthermia is most commonly delivered with a transurethral catheter. Some devices cool the urethral mucosa to decrease the risk of injury. However, if temperatures do not go above 45°C, cooling is unnecessary. Improvements in symptom scores and flow rates are obtained, but (as with laser surgery) large randomized studies with long-term follow-up are needed to assess durability and cost-effectiveness. Re-treatment rates are reported to be 9-21% at 5 years.
3. Implant to Open Prostatic Urethra (Urolift)
The UroLift system uses permanent nitinol and stainless steel implants placed under cystoscopic guidance to retract the lateral lobes of the prostate and mechanically open the prostatic urethra. The procedure can be performed under local anesthesia in the outpatient setting, and holding anticoagulation medication is not necessary. The ideal candidate has primarily lateral lobe hyperplasia and a prostate volume under 80 mL. Short-term data show improved symptoms and voiding flow rates with no de novo erectile dysfunction or incontinence. Re-treatment rates within 5 years have been reported to be as high as 13.6%.
4. Water Vapor Thermal Therapy (Rezum)
This minimally invasive, FDA-approved technique uses a modified cystoscope to deliver water vapor into the prostatic tissue. As the steam condenses back into water, it releases large amounts of stored thermal energy leading to tissue necrosis and resorption of tissue within about 3 months. This procedure is done in the clinic or ambulatory surgery setting with local anesthesia; it requires 3-7 days of bladder catheterization. In contrast to the UroLift procedure, there is a significant reduction in prostate volume over time, about 30% by 6 months, which relieves lower urinary tract symptoms as a result. A 6-year randomized, controlled trial reported significant objective improvement in lower urinary tract symptoms as early as 2 weeks post-procedure, improvement that remained durable throughout the 6-year period. Recommended prostate volume for Rezum treatment is 30-80 mL. Advantages include the minimally invasive, outpatient nature of the procedure with no significant bleeding risk even for anticoagulated patients, ability to treat the median lobe, and no reports of de novo erectile dysfunction or urinary incontinence. Disadvantages include slower recovery and longer bladder catheterization times compared to TURP and laser procedures. Re-treatment rate at 4 years was reported to be 4.4%, a rate far lower than other minimally invasive options.
The Optilume BPH catheter system is the first minimally invasive device with a dual mechanical and pharmacological mechanism of action that builds on the device's original use in treating recurrent urethral strictures. The BPH balloon creates an anterior commissurotomy with simultaneous paclitaxel delivery to prevent regrowth or refusion of the anterior prostatic lateral lobes. A double-blind, randomized, sham-controlled study showed improvement in flow rate, post-void residual PVR and patient satisfaction scores that were sustained at 1 year. Treatment was limited to prostates ranging in size from 20 to 80 mL, and long-term benefit has yet to be proven.
E. Simple Prostatectomy
When the prostate is very large, a simple prostatectomy by an open or robotic enucleation approach may be considered. What size is "too large" depends on the surgeon's experience with TURP. Glands over 100 g are usually considered for enucleation. In addition to size, other relative indications for open prostatectomy include when there is a concomitant bladder diverticulum or stone, and when dorsal lithotomy positioning of the patient is not possible.
Simple prostatectomy can be performed with either a suprapubic or retropubic approach. Simple suprapubic prostatectomy is performed transvesically and is the operation of choice if there is a concomitant bladder stone that is not amenable to transurethral treatment (>3 cm). These operations can also be performed via robotic-assisted laparoscopic techniques with shorter hospital stays, less blood loss, and decreased need for a suprapubic catheter.
When to Refer
- Obstructive uropathy.
- Patient dissatisfaction with medical therapy.
- Patient interest in surgical treatments.
- Need for further evaluation (cystoscopy) or surgical intervention.
GaoBet al. Office-based procedures for BPH. Curr Urol Rep. 2021;22:63. [PMID: 34913101] KaplanSAet al. The PINNACLE Study: a double-blind, randomized, sham-controlled study evaluating the Optilume BPH Catheter System for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2023;210:500. [PMID: 37555604] McVaryKTet al. Final 5-year outcomes of the multicenter randomized sham-controlled trial of a water vapor thermal therapy for treatment of moderate to severe lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2021;206:715. [PMID: 33872051] ParsonsJKet al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA Guideline Amendment 2020. J Urol. 2020;204:799. [PMID: 32698710] RukstalisDet al. Prostatic urethral lift (PUL) for obstructive median lobes: 12-month results of the MedLift Study. Prostate Cancer Prostatic Dis. 2019;22:411. [PMID: 30542055] SterlingJet al. Comparing outcomes of medical management and minimally invasive surgical techniques for lower urinary tract symptoms due to BPH. Curr Urol Rep. 2019;20:29. [PMID: 30989392] ZornKCet al. Aquablation therapy in large prostates (80-150 cc) for lower urinary tract symptoms due to benign prostatic hyperplasia: WATER II 3-year trial results. BJUI Compass. 2021;3:130. [PMID: 35474721] |