Description
- Chronotropy refers to the ability of the heart to change its rate of electrical depolarization, with corresponding mechanical contraction.
- Positive chronotropy indicates an increase in heart rate
- Generally occurs in response to physiologic stress and is mediated by the autonomic nervous system.
- Increases cardiac output directly.
- Normal positive chronotropic response decreases in elderly patients.
- Negative chronotropy indicates a decrease in heart rate and can be beneficial in clinical situations such as myocardial ischemia, Tetralogy of Fallot, hypertrophic cardiomyopathy and stenotic valves.
- Pacemaker cells exist in different regions of the heart: The sinoatrial (SA) node, the atrioventricular (AV) node, and the His–Purkinje bundle. Each region has its own intrinsic rate of action potential firing. Pacemaker cells in the SA node have the highest intrinsic rate of all regions and thus drive the rest of the conduction system; they are considered to be the “pacemaker” of the heart (1).
- Spontaneous depolarization. The SA nodal cells have no true resting potential, but instead generate regular, spontaneous action potentials.
- Intracellular Ca2+ modulation leads to diastolic depolarization in the node. The depolarization propagates through the rest of the conduction system and leads to systolic contraction of myocytes (1).
- Rate of spontaneous depolarization. Under the control of sympathetic and parasympathetic nerve activity as well as circulating catecholamines.
- Muscarinic acetylcholine receptors are densely located in the SA node. When agonized, they hyperpolarize the SA node cell membranes and decrease the spontaneous phase 4 slope, resulting in negative chronotropy. They also function to prolong refractoriness and AV nodal action potential propagation.
- Agonism can result from parasympathetic nervous system activity, such as an increase in vagal tone.
Antagonism can result from sympathetic nervous system activity (1).
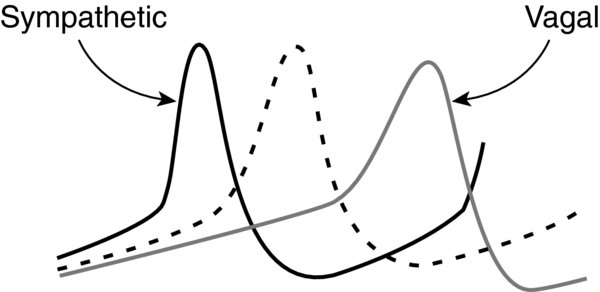
FIGURE 1. Sympathetic activity results in a hypopolarized (more positive) membrane resting potential and an increased spontaneous phase 4 slope.
Conversely, vagal activity results in a hyperpolarized (more negative) membrane resting potential and a decreased spontaneous phase 4 slope.
- Beta-receptors are located in the SA node; when agonized, they lead to altered intracellular Ca2+ release, via a cAMP pathway, resulting in positive chronotropy (1).
- The SA node is located at the junction of the superior vena cava and the right atrial appendage
- It is innervated by fibers from both the sympathetic and parasympathetic (vagal) nervous systems (1).
Physiology/Pathophysiology
- Positive chronotropy can be used to
- Increase cardiac output (stroke volume times heart rate). Used to treat severe bradycardia (e.g., oculocardiac reflex or vasovagal reflex).
- Decrease regurgitant volume in aortic or mitral regurgitation. By decreasing the systolic time, the regurgitant volume also decreases.
- Negative chronotropy is a therapeutic modality used in several disease states:
- Coronary artery disease/myocardial ischemia. Decreases myocardial oxygen demand (3) as well as supply (increases diastolic time and duration that the left ventricle is perfused).
- Acute aortic dissection. Decreased heart rate reduces shear stress on the aorta (4) [A].
- Hypertrophic/obstructive cardiomyopathy. Dynamic outflow obstruction will decrease as the heart has more time to fill and does not empty as much (3).
- Stenotic valve lesions (e.g., aortic stenosis and mitral stenosis). Allows for increased ventricular filling (increased diastolic time during each cardiac cycle) along with improved ejection of blood (increased systolic time during each cardiac cycle).
- Chronically elevated resting heart rate has multiple negative myocardial and vascular consequences:
- Impaired left ventricular (LV) function
- Impaired LV relaxation
- LV hypertrophy
- Endothelial injury/atherosclerosis (3)
Pediatric Considerations
| Neonatal left ventricles are stiffer than in adults and are less able to tolerate volume loads. Because stroke volumes are relatively fixed, they become dependent on the heart rate to maintain cardiac output (5) [A]. |
Pediatric Considerations
| Elderly patients are more prone to chronotropic incompetence—the inability to adequately increase heart rate in response to normal stimuli (85% maximal predicted heart rate). This may be secondary to remodeling that is associated with an augmentation of collagen content. It has also been hypothesized that it can be a sign of occult coronary artery disease and may correlate with increased mortality (6). |
Negative chronotropy is accomplished using
- Beta-receptor antagonists: Metoprolol, propranolol, esmolol, and atenolol. They function to decrease spontaneous depolarization of SA node cells and thus slow the heart rate (7).
Ca2+ channel antagonists (class IV antiarrhythmics): Diltiazem and verapamil (8). They function to block L-type Ca2+ channels found in the SA and AV nodes, thus slowing automaticity as well as AV conduction (9).
Positive chronotropy can result from
- Sympathomimetics
- Endogenous molecules (available for exogenous administration)
- Norepinephrine stimulates both alpha-1 and beta-1 receptors. Unopposed vasoconstriction from alpha-1 stimulation may cause a reflex bradycardia that is capable of off-setting chronotropic responses from beta-1 stimulation (2).
- Epinephrine stimulates beta-1, beta-2, and alpha-1 receptors and is a powerful chronotrope, especially at low doses (0.01–0.05 µg/kg/min) (2).
- Dopamine stimulates D1, beta-1, and alpha-1 receptors; it has a predominant chronotropic beta-1 response at mid-range doses (2–10 µg/kg/min) (2).
- Synthetic molecules
- Isoproterenol is a nonselective beta-1 and beta-2 agonist (2).
- Dobutamine is a selective beta-1 agonist (2).
- Ephedrine acts indirectly to increase the release of stored norepinephrine from synaptic junctions as well as directly binds to beta-1 receptors. Ephedrine is less effective when stores of norepinephrine have been depleted from the synaptic junction as in congestive heart failure (2).
- Endogenous molecules (available for exogenous administration)
- Muscarinic acetylcholine antagonists also increase chronotropy by blocking vagal transmission to the SA and AV node. They include atropine and glycopyrrolate.