Description
- Respiratory compliance is defined as the change in respiratory system volume divided by the change in distending airway pressure; C =
 V/
V/ P.
P. - Respiratory system (RS) compliance is the composite of chest wall (CW) compliance, and lung (L) compliance. RS, CW, and L compliances are concepts of respiratory mechanics, the branch of physiology studying the forces causing or opposing air movement in and out of the lungs.
- Compliance is an index of the elastic properties of the respiratory system; it is also a determinant of alveolar gas flow and work of breathing.
- The inverse, or reciprocal, of compliance is elastance: E =
 P/
P/ V.
V. - Measuring lung compliance provides useful data to quantify the severity of lung pathology and to decide ventilatory strategies in the operating room and intensive care unit (ICU) (1) [A].
- Respiratory system compliance is the change in milliliters per cmH2O pressure (mL/cmH2O). It provides an objective measure and means to discuss an elastic structure's ability (or inability) to “stretch.”
- Compliance values vary with lung volume, and, thus, are not linear. CW, L, and RS compliance are maximal at the functional residual capacity (FRC).
- FRC is defined as the balance point between the natural tendency of the CW toward expansion and of the lung toward collapse. Such balance determines the lung volume at rest.
- When lung values are above or below the FRC, compliance values decrease; there is a reduced change in volume for a given pressure.
- Compliance is analogous to electrical capacitance, where chest wall and lung compliance are in series. It is also calculated in the same manner: 1/total compliance = 1/lung compliance + 1/chest wall compliance. Typical values:
- Total compliance: 100 mL/cmH2O
- C(L): 150–200 mL/cmH2O
- C(CW): 200 mL/cmH2O
- Elastance is the reciprocal of compliance and is a measure of the RS's tendency to recoil toward its original dimensions following deformation and upon removal of a distending or compressing force; it is analogous to the behavior of a stretched rubber band or spring.
- Chest wall recoil is due to anatomical structures such as the ribs and chest wall muscles, whereas, lung recoil is due to elastin fibers and the surface tension forces in alveoli.
- Inspiration is caused by the active contraction of the diaphragm and other inspiratory muscles. At rest, expiration is mainly passive and is due to relaxation of respiratory muscles and the elastic recoil of lungs.
- Elastin protein is found in the lungs, as well as arteries, skin, and bladder. Following inhalation, or stretch, it provides the force to return the lungs to their FRC. Pathologic disease states include Marfan syndrome or
 -1 antitrypsin disease.
-1 antitrypsin disease.
- The surface tension of alveoli favors collapse of the lung following LaPlace's law: P = 2T/R, where P is pressure within the alveoli measured in pascals (Pa), T is the surface tension of the alveoli measured in Newtons/meter, and R is the radius of the alveoli measured in meters (m). Surfactant is a lipoprotein complex produced by type 2 alveolar cells. It decreases alveolar surface tension (T), and hence increases compliance, decreases work of breathing, and helps to prevent alveolar collapse.
Determinants of respiratory system compliance include the lungs and chest wall (and any associated disease or pathology). Of note, the abdominal contents are a major determinant of respiratory compliance; increased intra-abdominal pressure (obesity, pneumoperitoneum, pregancy) translates to decreased compliance.
Physiology/Pathophysiology
- In a normal respiratory system, tidal volume ventilation should occur along the rectilinear portion of the compliance curve. In disease states, however, it becomes more difficult to adequately deliver tidal volume ventilation within the limits of the rectilinear portion of the compliance curve.
- Restrictive pulmonary disorders decrease compliance of the lungs, chest wall, or both.
- Lung compliance: Pulmonary edema, fibrosis, pneumonia, acute respiratory distress syndrome (ARDS), acute lung injury (ALI), pleural effusions, pneumothorax, mediastinal masses, and vascular engorgement
- Chest wall: Kyphoscoliosis and muscular disease
- Both: Increased abdominal pressure from pregnancy, ascites, obesity, and laparoscopic procedures.
- Obstructive lung disease. In emphysema or bullous lung disease, although static compliance can be increased, dynamic compliance may be decreased.
- Age affects chest wall compliance. In the elderly, the thorax is stiff due to ossification and increases outward forces. In infants, the CW has a very high compliance; as a result, during passive expiration, the outward chest wall recoil does not oppose the lungs tendency toward collapse. This may cause the FRC to decrease below the airway's closing pressure. Positive end-expiratory pressure (PEEP) may counteract this phenomenon and preserve FRC, and hence, oxygenation and ventilation.
- In the operating room, the anesthesia provider can assess dynamic and static compliance.
- The anesthesia machine is capable of measuring pressures during “peak” and “plateau,” or dynamic and static inspiratory breaths, respectively.
- These values and curves allow inferences and calculations of the compliance.
- Some machines are capable of generating pressure–volume curves; where the slope is equal to compliance at a specific volume.
- Dynamic compliance (Cdyn) is specific to the peak inspiratory or distending compliance of the lung and chest wall.
- C(dyn) = V(t)/(Ppeak – PEEP); volume change divided by peak airway pressure minus end-expiratory pressure.
- Decreased dynamic compliance is seen with atelectasis, asthma, pulmonary edema, pleural effusions, ascites, abdominal retractors or packing, pneumoperitoneum, and endobronchial intubation.
- Artifactual increases in dynamic pressure measurements result from the breathing tube and circuit apparatus: ETT diameter, secretions, kinking; ventilator settings. They do not actually change compliance.
- Static compliance (Cstat) is specific to end- inspiration, when no gas flow is present. It is mainly determined by the lung and chest wall compliance, but not by ventilator settings, the breathing circuit, or ETT.
- C(stat) = V(t)/(Pplat – PEEP); volume change divided by plateau pressure minus end-expiratory pressure
- Intrinsic PEEP (assessed by means of an end-expiratory pause) must be considered, otherwise compliance could be miscalculated.
- Specific compliance: C/FRC. It mirrors the elasticity of the aerated lung tissues.
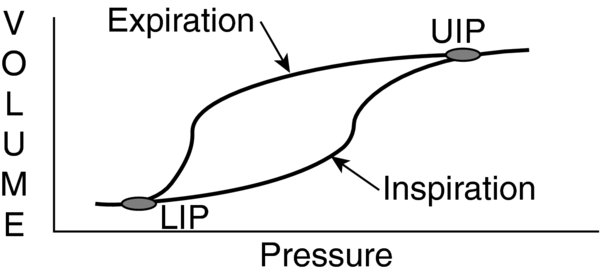
- Pressure–volume curves can be constructed to reflect changes in static and dynamic compliance. Volume (y-axis) is plotted as a function of pressure (x-axis) and the slope corresponds to compliance. Both inspiratory and expiratory compliance curves can be constructed.
- The curves are nonlinear, but sigma shaped, when compliance is tested over a sufficient range of vital capacity. In most patients, a lower and a superior inflection point can be detected. These points correspond to volumes of the respiratory system at which its elastic properties change rapidly. If present, the lower inflection point (LIP) identifies an abrupt increase in the compliance that has been traditionally interpreted as a sign of lung tissue recruitment. Alternatively, the upper inflection point (UIP) signifies an abrupt decrease in compliance as a result of overdistention of alveoli. Hysteresis between the inspiratory and expiratory compliance curves is also observed. Hysteresis reflects that, upon expiration, at a given pressure, the lungs exhibit greater volume compared to inspiration. Thus, the expiratory and inspiratory limbs of the compliance curve do not overlap.
- Compliance curves are utilized in the ICU to assess severity of lung diseases, guide ventilatory management, and evaluate progression of the lung disease or efficacy of undertaken treatments.
- General anesthesia affects chest wall compliance. Volatile IV anesthetics as well as paralysis result in diaphragm relaxation with consequent cranial displacement of the abdominal contents. This results in increased intra-abdominal pressure with decreased CW and L compliance (2)]A].
- Intraoperative clinical changes in compliance can be anticipated based on patient-related and procedure-related risk factors. Ventilator settings (PEEP, TV, RR) should be adjusted accordingly. Decreased compliance can be seen with:
- Patient-related risk factors: Age, high BMI, smoking, respiratory infections, pregnancy, abdominal distension, chest deformations.
- Procedure-related risk factors: Thoracic and abdominal procedures, Trendelenburg, surgical retractors, cardiopulmonary bypass, one lung ventilation, and pneumoperitoneum.
- Atelectasis from pulmonary edema, low tidal volumes, pulmonary disease, foreign body aspiration, and endobronchial intubation can decrease compliance.
- An abrupt increase in peak pressures, in the absence of any of the previously mentioned changes, may suggest a tube kinking or occlusion by secretions, as well as an asthma attack.
- Increases in compliance may also be seen with alveolar recruitment, resolution of lung parenchyma pathological processes, and changes in ventilator setting or in CW compliance.
- ARDS and ALI are disorders that profoundly affect pulmonary compliance.
- During lung expansion with positive pressure inhalation, new alveoli are recruited and start to open (reflected by the LIP on pressure-volume curves).
- On exhalation, some alveoli collapse or are derecruited (reflected by a steep slope change in the expiratory pressure-volume curve).
- The exact physiologic meaning of the LIP is still debated. Traditionally, its presence has been interpreted as the airway pressure value at which many alveolar units are recruited simultaneously, but studies in ICU patients have shown that it may be more influenced by the CW than the L component. Additionally, CT studies have shown that recruitment occurs along the entire compliance curve, independent of the LIP.
- Maintaining airway pressures between the LIP and UIP may prevent cyclic alveolar derecruitment and overdistention. Ventilation outside the inflection points can cause shear stress with resultant release of inflammatory mediators that can have both a local and systemic effect and contribute to multiorgan failure. Traditionally, in ICU patients, the PEEP level is set above the LIP (2,3,4) [A].
- Respiratory compliance is also a determinant of the respiratory work of breathing, and influences the patient's ability to sustain unsupported ventilation. Monitoring compliance can provide additional useful information in a ventilator weaning process.
- 1/total compliance = 1/lung compliance + 1/chest wall compliance
- Total elastance = lung elastance + chest wall elastance
- C(dyn) = V(t)/(Ppeak – PEEP)
- C(stat) = V(t)/(Pplat – PEEP)
- LaPlace's law: P = 2T/R; P is pressure within the alveoli measured in pascals (Pa), T is surface tension of the alveoli measured in newtons/meter, R is radius of the alveoli measured in meters (m).
FIGURE 1. Pressure-volume curve reflecting volume as function of pressure; the slope corresponds to compliance.
The upper inflection point (UIP) represents an abrupt decrease in compliance from overdistention of alveoli. The lower inflection point (LIP) reflects an abrupt increase in compliance from lung tissue recruitment. Hysteresis is also demonstrated.