Description
- Method of ventilation that is characterized as an open system, with high frequency, and low tidal volumes.
- Inspiration is characterized as positive pressure, jet pulsed breaths delivered via a jet nozzle. Exhalation occurs passively and around the jet nozzle; there is no dedicated expiratory limb.
- Jet ventilation may be performed supraglottically, infraglottically, or transtracheally. Furthermore, it can be delivered manually or by automatic devices.
- Anesthesia providers utilize jet ventilation when the operative field needs to be shared or still; or in the formidable "cannot ventilate, cannot intubate" difficult airway.
- Distinguishing and desirable features of jet ventilation include an open system, high frequency, and low tidal volumes.
- Open system for inspiration and exhalation. The internal diameter (ID) of the jet nozzle is small and does not "seal" the airway (unlike the endotracheal tube (ETT) cuff). Furthermore, there is no dedicated expiratory limb (unlike controlled mechanical ventilation (CMV)); instead air egresses out and around the nozzle. Additionally, the jet pulsed inspiratory breaths entrain air via the Venturi effect (high speed pulses generate negative pressures on the gas flow edge that drags air or oxygen from the opening environment into the airway).
- High frequency (>60 breaths/minute). Results in "auto-PEEP" (positive end-expiratory pressure) from air trapping and subsequent alveolar opening; without this effect, the low tidal volumes generated would not be able to insufflate alveoli and optimize V/Q matching. Thus, this is a desired effect that increases airway pressures (Paw) and PaO2, but at the risk of hypercapnia and barotrauma.
- Low tidal volumes. Correspond to low peak airway pressures (PIP) and intrathoracic pressures, with resultant increases in venous return.
- Components of jet ventilation include a gas source, jet valve, and jet nozzle.
- Gas source: Oxygen or oxygen mixed with air from either a wall source or cylinder.
- Jet valve: Electronically or manually controlled valve to generate jet pulses when it opens and closes. Gas passes intermittently through the valve to produce jet pulses at different frequency.
- Jet nozzle: Any tubing with an ID around 2 mm to deliver jet pulses from the jet valve. These are usually disposable compliant tubes at various lengths (e.g., 14G or 16G angiocatheter, transtracheal jet catheter, Cook tube exchanger, and soft suction catheter).
- Working parameters and settings include respiratory frequency, driving pressure, inspiration time, FiO2, and humidification.
- Respiratory frequency: 15–150 breaths/minute. As frequency is increased, exhalation time is reduced and can result in physiologically beneficial auto-PEEPing. Air build-up, due to insufficient time for exhalation, results in alveolar opening with consequent improvements in V/Q matching and oxygenation. High frequencies result in reduced chest wall excursions, thereby providing a more "still" surgical field. However, the shorter exhalation times combined with the smaller tidal volumes compared to CMV results in less CO2 elimination (hypercarbia) and greater dead space ventilation (inefficient ventilation).
- Driving pressure refers to the pressure applied to the jet valve. In adults, settings usually start at ~20–25 Psi, with a maximum of 50 Psi. Driving pressure is a major determinant of tidal volume; increases result in higher tidal volumes and minute ventilation.
- Inspiration time is typically set at 30–40%. It dictates the time spent in insufflation versus exhalation. By increasing this value, tidal volumes and oxygenation (due to reduced exhalation time and auto-PEEPing) are increased
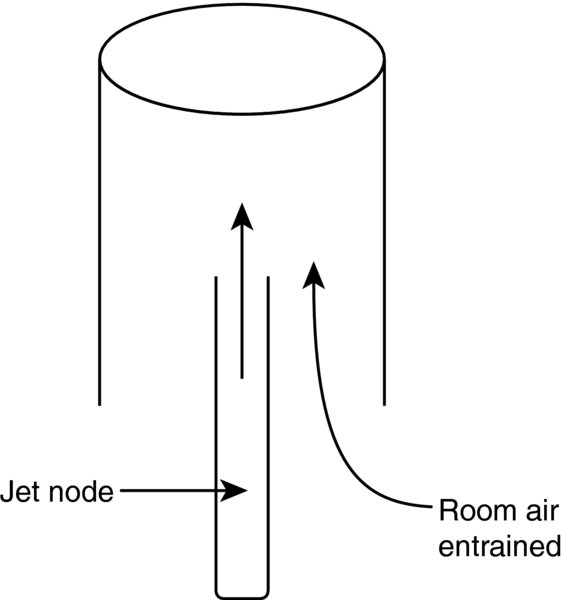
FiO2: Is set at 100% and is the oxygen concentration at the jet nozzle. The actual FiO2 is significantly less in the alveoli due to Venturi effects and the open system (Figure 1)
FIGURE 1. Venturi effect entrains room air at the level of the jet nozzle.
- Humidification: for prolonged use of jet ventilation, gas from jet pulses should be humidified to avoid airway mucus membrane damage or formation of airway mucus clot and airway obstruction.
- Monitoring during jet ventilation is limited because it is an open system. The following cannot be accurately monitored or measured.
- FiO2. Decreases along the axis of the airway towards alveoli due to air entrance from Venturi effects. The entrained air from the surrounding opening system mixes with and dilutes the injected oxygen from the jet valve. This decreases the actual oxygen at the alveolar gas exchange site.
- Partial pressure of end-tidal of carbon dioxide (PetCO2). Varies along the axis of the airway due to the opening system.
- Airway pressure. Increases along the axis of the airway due to air trapping, especially at high frequency.
- Tidal volume. Primarily depends on the driving pressure.
Approaches of jet ventilation include supraglottic, infraglottic, and transtracheal.
- Supraglottic jet ventilation (SJV). Jet nozzle is positioned above the vocal cords with the air aimed toward the glottic opening. Non-invasive and may have less incidence of barotrauma compared to other approaches; additionally, faster to set up. Can be utilized in "cannot intubate, cannot ventilate" and difficult airway scenarios as well as in upper GI endoscopy cases. Also applicable to when the jet ventilator is attached to an LMA adaptor.
- Infraglottic jet ventilation. Jet nozzle is positioned below the vocal cords. Has less ambient air entrainment (from Venturi effect) and possibly sore throat than supraglottic access. Utilized when sharing the airway; additionally, also applicable to when the jet ventilator is attached to an ETT adaptor
- Transtracheal jet ventilation (TTJV). Jet nozzle is attached to cricothyroidotomy access. Invasive and higher risk of barotrauma (up to 10% in emergent airway access). Utilized in "cannot ventilate, cannot intubate" scenarios; however, must be avoided in complete upper airway obstruction to prevent barotrauma.
Physiology/Pathophysiology
- Barotrauma occurs when pressure builds up in a closed tissue pocket, similar to when a balloon is constantly blown up until it eventually ruptures. The high-pressure system can result in injuries including pneumothorax, pneumomediastinum, and subcutaneous emphysema. Avoid jet ventilation in known barotrauma or where there is upper airway obstruction that would preclude gas egress/exhalation. Additionally, some suggested preventative measures include
- Begin to learn and use jet ventilation in elective cases rather than during emergent TTJV
- Keep the airway system open and avoid pressure building up in a closed tissue pocket
- Consider using noninvasive jet ventilation (supraglottic)
- Implement low driving pressures (<25 Psi), low frequency (<120 breaths/minute)
- Hypercapnia. Worsened with high-frequency jet ventilation, particularly in obese patients, reduced chest wall compliance, or COPD with increased baseline CO2 levels. Consider switching to CMV periodically to check PetCO2 to avoid hypercapnia or hypocapnia. Can check ABG if arterial line is available. May be treated by increasing tidal volumes (increase driving pressure or inspiratory time, or decrease respiratory rate).
- Insufficient oxygenation can result from insufficient alveolar expansion (insufficient ventilation). Seen more commonly in patients with baseline pulmonary disease. May be prevented by increased FiO2, driving pressure, or inspiratory time. Adding ambient oxygen can increase the delivered FiO2.
- Inadequate humidification may result in necrotizing tracheobronchitis and mucus clot-mediated airway obstruction. Use humidification methods if available especially for prolonged use of jet ventilation. (Current clinical studies do not identify an agreed upon time point).
- With its three features of open system, high frequency, and small tidal volumes, jet ventilation is often utilized to support respiration and perform mechanical ventilation in certain clinical scenarios.
- Open systems
- "Cannot ventilate, cannot intubate" emergent airway. Included in the ASA difficult airway algorithm. TTJV is comparatively faster, easier to perform, and more often used than emergent tracheostomy. A cricothyroidotomy is performed with either a commercially available cricothyroidotomy needle or a 14G or 16G angio catheter.
- GI endoscopy; SJV via a nasal airway allows oxygenation and ventilation without intubating or other airway devices that are invasive or preclude endoscopy.
- Difficult airway management. Allows oxygenation while a definitive airway is attained, as during the process of tracheal intubation under direct laryngoscopy or a fiberoptic bronchoscopy.
- ENT cases with an open airway such as rigid bronchoscopy, vocal cord, or other upper airway surgeries. During surgical procedures of the upper respiratory tract, surgeons and anesthesia providers must share the airway, and the use of an ETT may obscure access to the surgical site; conversely, surgical instruments can preclude tight sealing of the airway. High-frequency jet ventilation (HFJV) is used to continuously or intermittently provide oxygenation and ventilation.
- Thoracic or pulmonary cases such as one lung ventilation, bronchofiberoptic examination or resection of airway tumors, tracheal resection, bronchopleural fistulas
- High frequency to provide oxygenation with minimal diaphragm movement
- Electrophysiology procedures such as atrial fibrillation or atrial flutter ablations. Less movement allows for more precise mapping and ablation. May reduce the operating time relatively.
- Shock wave lithotripsy. CMV or SV via an LMA can result in significant respiratory movement and is akin to hitting a "moving target." Jet ventilation may be implemented at high frequency and therefore minimize the diaphragm movement and provide optimistic environment for lithotripsy.
- Low tidal volume and low intrathoracic pressure. Serves to minimize interference with venous return and may improve hemodynamic in patients with hypovolemia or shock. HFJV (RR at 100/min) seems to be better than CMV to maintain BP and cardiac output during hypovolemia in animal studies. Synchronization of the heart rate with breathing using the R wave of the EKG to trigger jet ventilation has been shown to improve cardiac function in animal studies.
- Total IV anesthetic technique is utilized to maintain general anesthesia when utilized in this capacity. A balanced technique utilizing sedatives, opioids, or muscle relaxants may be utilized depending on the case specifics and the needs.