Description
- Neurogenic pulmonary edema (NPE) is an acute, potentially life-threatening complication of significant CNS injury, such as subarachnoid hemorrhage (SAH), prolonged seizures, or traumatic brain injury (TBI).
- NPE consists of a marked increase in pulmonary interstitial and alveolar fluid, with resultant dyspnea, tachypnea, tachycardia, basilar rales, copious frothy sputum, possible hemoptysis, and hypoxemia. It usually develops within minutes to hours after injury; however, immediate and late (days) onset has been described.
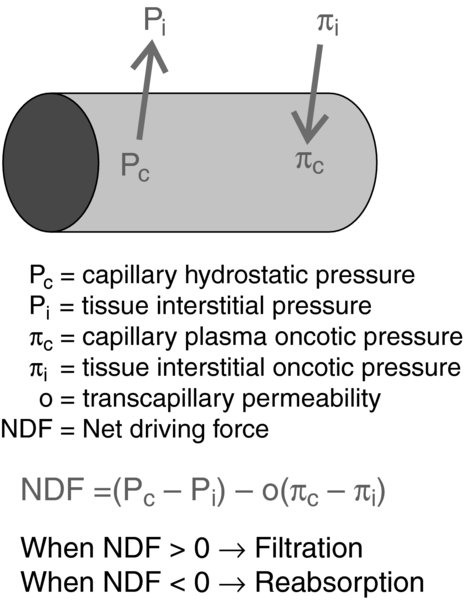
- The Starling's equation describes the effects of hydrostatic and oncotic pressures on fluid movement between the intravascular and extracellular compartments.
- Capillary hydrostatic pressure: Pressure drives fluid out of the capillary, and is highest at the arteriolar end of the capillary and lowest at the venular end.
- Capillary oncotic pressure: Plasma proteins keep/draw fluid into the capillary via osmotic effects. Proteins do not readily cross the endothelial cells and, hence, do not reach equilibrium within the two compartments. Albumin accounts for 70–80% of the oncotic pressure of the plasma.
- Transcapillary permeability: Permeability of the vessel wall to water. The capillaries’ semi-permeable membrane allows water to pass more freely than protein. If the gaps between the cells of the vessel wall widen, then permeability to proteins increases (results in edema).
- NPE "trigger zones" are located in the:
- Hypothalamus
- Cervical spinal cord
- Medulla. Contains several important centers that are believed to contribute to the pathogenesis of NPE via sympathetic stimulation: Solitary tract, area postrema, medial reticulated nucleus, and dorsal motor nucleus. Perioperative bilateral lesions in the medulla at the solitary tract and at the A1 group of neuroadrenergic neurons can cause hypertension and NPE.
Physiology/Pathophysiology
The exact mechanism is unknown. Increased intracranial pressure (ICP), brain injury, or hemorrhage is believed to cause ischemia or compression of medullary centers; this is believed to begin a cascade of events that alter Starling's forces:
- Increased pulmonary capillary hydrostatic pressure results in an outward driving force of fluids from the pulmonary capillaries.
- The inciting CNS injury sets off a massive sympathetic discharge. This results in systemic arterial hypertension, peripheral vasoconstriction, increased pulmonary artery pressure, and pulmonary vasoconstriction.
- The increased myocardial workload (oxygen consumption) can cause deterioration of cardiac function. Decreases in left ventricular function can lead to increased left atrial pressures with resultant pulmonary edema.
- Increased pulmonary artery permeability is a key step preceding NPE.
- Hemodynamic-independent: Some studies suggest that adrenergic activation increases pulmonary vessel permeability. Epinephrine and norepinephrine can have:
- Direct effects that increase vascular permeability
- Indirect effects by stimulating secondary mediators which increase the vascular permeability, such as histamine or bradykinin
- Hemodynamic-dependent: The "Blast theory" proposed by Theodore and Robin in 1975 states that a severe rise of pulmonary capillary pressure causes increased pulmonary vascular permeability, causing a shift of intravascular volume from the high-resistance systemic circulation to the low-resistance pulmonary circulation. Microvascular injury may be caused by excessive pulmonary vasoconstriction; the consequent increase in vascular permeability results in edema.
- Hemodynamic-independent: Some studies suggest that adrenergic activation increases pulmonary vessel permeability. Epinephrine and norepinephrine can have:
- Capillary oncotic pressure: The increased permeability allows for passage of proteins through the capillaries, which then exert oncotic pressure and draw fluid out of the capillaries. Studies have shown that the alveolar fluid of patients who have developed NPE has a similar protein concentration to plasma.
- Patients who develop NPE have a very poor prognosis.
- Associated with a 60–100% mortality
- Reflects the severity of the underlying etiology; thus, an ominous sign
- One retrospective study of 680 postmortem deaths from non-traumatic intracranial hemorrhage showed that pulmonary edema was seen in approximately 75% of cases.
- NPE may result from several types of cerebral lesions; the most common are:
- Fatal subarachnoid hemorrhage: seen in 70% of patients
- Status epilepticus: seen in 30% of patients
- Traumatic brain injury: seen in 50% of patients
- Presentation:
- Immediately (minutes to hours); most common
- Delayed (days) is also seen; less common
- Associated with hemodynamic and cardiac abnormalities:
- Neurogenic shock
- Left ventricular failure; usually transient and reversible
- Elevated troponin level; does not necessarily indicate permanent myocardial injury
- Chest radiography:
- Pulmonary infiltrates; maybe in a "butterfly" pattern
- Cardiac silhouette is usually normal.
- Differential diagnosis includes:
- Aspiration pneumonia
- Cardiac dysfunction: Often NPE with cardiac changes is erroneously attributed to coronary disease. ECG and enzyme levels are not useful in distinguishing between myocardial infarction and neurologic etiology of cardiopulmonary dysfunction, as they may be abnormal in both entities. The transient nature of NPE helps distinguish between neurologic and cardiac origins.
- Acute respiratory distress syndrome (ARDS)
- Treatment
- Underlying neurologic injury. Because overall outcome is dependent upon the inciting cause, efforts should focus on this. There should be an emphasis on decreasing the ICP.
- Supportive treatment consists of supplemental oxygen with or without mechanical ventilation, depending on the severity of hypoxemia.
- Medications: There are few studies that evaluate the efficacy of medications to treat NPE in humans; however, the following may be useful:
- Beta-adrenergic antagonists may decrease pulmonary capillary permeability but are usually contraindicated in the setting of cardiopulmonary and hemodynamic compromise.
- Dobutamine may increase cardiac output, counter alpha agonism, and promote diuresis (improved renal perfusion).
- Steroids have not been tested in humans and may be detrimental.
- Diuretics should be avoided in the absence of hypervolemia due to the risk of hypotension (can worsen cerebral perfusion pressure). However, mannitol is commonly administered to reduce brain edema, but it has unproven benefits for pulmonary edema.
- Chlorpromazine, via alpha-adrenergic blockade, has been used in case reports.