Description
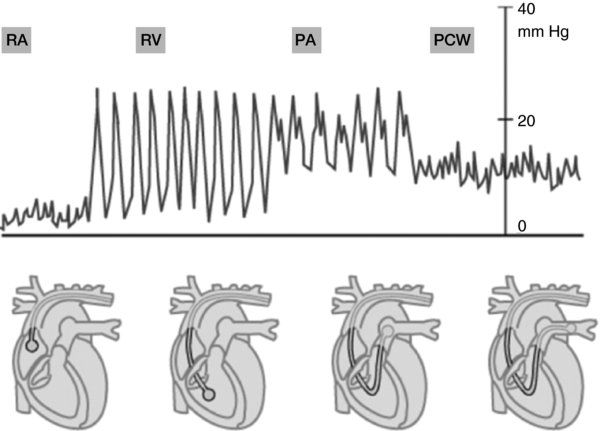
- Pulmonary artery catheters are flow-directed, balloon-tipped devices that can provide:
- Pressure measurements of the central venous/right atrium (RA), right ventricle (RV), and pulmonary artery (PA); the left atrial and left ventricular end diastolic pressure can be estimated by the pulmonary capillary wedge pressure (PCWP), also known as the PA occlusion or wedge pressure.
- An assessment of the cardiac output/cardiac index
- Values to calculate the pulmonary vascular resistance (PVR) and the systemic vascular resistance (SVR).
- Sampling of blood from the RA, RV, and PA; mixed venous oxygen saturation can be determined.
- Pressure values are a surrogate for volume, and are dependent upon the chamber compliance. To that extent, the use of echocardiography can provide a direct assessment of volume.
- Several randomized clinical trials have not been able to convincingly demonstrate the benefits of intervention on patient outcome in terms of morbidity and mortality in the ICU, management of heart failure, or the perioperative period
- RA waveform: Consists of 3 positive (a, c, v waves) and 2 negative (x, y descents) deflections.
- a wave reflects RA contraction near the end of ventricular diastole.
- c wave reflects bulging of the tricuspid valve into the RA during early ventricular systole.
- x descent corresponds to atrial relaxation and decreased RA pressure.
- v wave represents passive atrial filling during ventricular systole.
- y descent corresponds to tricuspid valve opening and filling of the RV in early ventricular diastole.
- The numeric value represents the mean pressure and is a surrogate for preload.
- RV waveform:
- Systolic pressure is dramatically increased, with a prominent upstroke and downstroke.
- Diastole is characterized by a flattened upstroke as the RV rapidly fills with blood; this is followed by a slow filling phase and then atrial systole (steeper slope).
- The numeric value is displayed as a systolic and diastolic value.
- PA waveform:
- Systolic pressure is similar to the RV pressure, but the diastolic pressure is increased (represents the diastolic vascular tone).
- A dicrotic notch represents closure of the pulmonic valve.
- PCWP waveform:
- Reflects LA pressures, with a shape similar to the RA tracing, but with higher pressure values and a more irregular tracing.
- a wave reflects LA contraction.
- c wave is often not seen, but reflects the mitral valve closure.
- x descent represents the decrease in LA pressure following the a wave.
- v wave represents the LA filling.
- y descent corresponds with decreased LA pressure following opening of the mitral valve and filling of the LV.
- Numeric values are used to estimate the LV end diastolic pressure (LVEDP; surrogate for LV preload) if no obstruction exists between the LA and the LV
- Respiratory cycle: Should be considered when interpreting pressure measurements.
- During spontaneous inspiration, the intrathoracic pressure decreases; whereas with exhalation, it increases. In the intubated patient, positive pressure ventilation has the reverse effect.
- Therefore, in order to minimize respiratory effects, measurements are made at end-expiration, when the intrathoracic pressure is close to zero.
- The standard, adult PAC is 7.0–9.0 FR and ~110 cm in length. It has several lumens and connections for transducing pressures. The lumens from proximal to distal are: Proximal lumen (25 cm from the distal tip, lies in the RA); injectate lumen (~20 cm from the distal tip, lies in the RV); thermistor lumen (~4 cm from the distal tip); distal lumen (tip of catheter, lies in either the right or left side of the PA); balloon lumen (tip of catheter, can inject 1.5 mL of air).
- Following the placement of a sterile introducer sheath into a central vein, the PA catheter is inserted while monitoring the waveforms and pressures. After the catheter tip has entered the RV, the distal balloon is inflated to "float" the catheter as blood is pumped toward the LV; akin to a sail amongst waves. Proper positioning is determined by the pressure waveform or fluoroscopic guidance.
Physiology/Pathophysiology
- RA pressure reflects the central venous pressure (CVP), and is increased in RV failure, right-sided valvular disease, and cardiac tamponade.
- Enlarged a waves are seen with tricuspid stenosis. "Cannon" a waves are seen with atrio-ventricular dissociation (RA contracts against a closed tricuspid valve during ventricular contraction).
- a waves may be absent in atrial fibrillation.
- Enlarged v waves are present with tricuspid regurgitation.
- Tamponade impairs venous return, decreasing the end-diastolic volume and cardiac output, dramatically increasing filling pressures, and leading to the equalization of pressures in all chambers at end-diastole.
- RV systolic pressure is increased in pulmonary hypertension, pulmonic stenosis, or pulmonary embolism. RV diastolic pressure is increased in right heart failure and cardiac tamponade.
- PA pressure elevations are seen in left heart failure, mitral valve disease, and primary parenchymal lung diseases such as chronic bronchitis and emphysema. Pulmonary vascular disease from pulmonary embolism and primary pulmonary hypertension also lead to elevated pressures. Left-to-right cardiac shunts, as in atrial septal and ventricular septal defects, are other potential causes.
- PCWP can be increased in left heart failure and mitral valvular disease.
- Enlarged a waves can be seen during mitral stenosis.
- Elevated v waves can be present with mitral regurgitation or ventricular septal defects.
- Complications with placement of the PAC.
- Arrhythmias are the most common complication
- Transient PVCs: 68% of placements
- Transient right bundle branch block: 5%. In patients with pre-existing left bundle branch block, it can lead to a complete heart block
- Persistent ventricular dysrhythmias: 3.1%
- Atrial dysrhythmias: 1.3%
- Pneumothorax occurs with 0.5% of IJ cannulations, but is more common with subclavian vein catheter placement.
- Infections can occur, with increased frequency in continuous monitoring and in patients with pre-existing sepsis.
- Hemorrhage and damage to vascular structures can also occur. PA rupture is rare, occurring in 0.02–0.2%, but has a mortality rate of 50%.
- Arrhythmias are the most common complication
- Despite the widespread use of PA catheters in hemodynamically unstable patients, there are many controversies that exist regarding appropriate indications for their usage. The American Society of Anesthesiologists Task force on Pulmonary Artery Catheterization concluded that the placement of PA catheters should not be routinely used with low risk of hemodynamic complications, and should be reserved for high-risk settings that depend on the patient, surgery, and practice-setting variables. If clinical assessment or non-invasive measures are not appropriate to determine the hemodynamic status, or if the use of the catheter can change management, then its use is indicated.
- Indications for PAC in surgical patients include:
- Procedures that have a high-risk of complications from hemodynamic shifts (cardiac surgery, aortic cross-clamping, liver transplantation).
- Patients with advanced cardiopulmonary disease.
- Shock. Can aid in the diagnosis, management, and measurement of therapeutic responses.
- Pulmonary edema to differentiate between the mechanisms (cardiogenic versus non-cardiogenic).
- Normal pressure values
- RA: 1–5 mm Hg (mean)
- RV: 15–30/1–7 mm Hg
- PA: 15–30/4–12 mm Hg, mean 9–19 mm Hg
- PCWP: 4–12 mm Hg (mean)
- Cardiac output (CO) = 4.0–6.5 Liters/minute (normal)
- This is measured in a PAC by the thermodilution technique, where a known volume and temperature of sterile solution is injected and the change in PA blood temperature is measured by the thermistor.
- CO can also be calculated by Fick's equation = (oxygen consumption)/(10 × arterio-venous oxygen difference)
- SvO2 (mixed venous blood oxygenation) = SaO2 – (VO2/[CO × 1.36 × Hb])