After completing this chapter, the reader will be able to:
1.Define terms related to the complications of vascular access devices.
2.Differentiate between local and systemic complications.
3.Describe risk factors and preventive interventions for local complications.
4.Identify noncytotoxic vesicant medications/solutions.
5.Discuss interventions shown to decrease risk for bloodstream infections.
6.Identify risk factors and preventive interventions for systemic complications.
7.Identify complications and risks associated with central vascular access devices.
8.Document relevant information related to vascular access device-related complications.
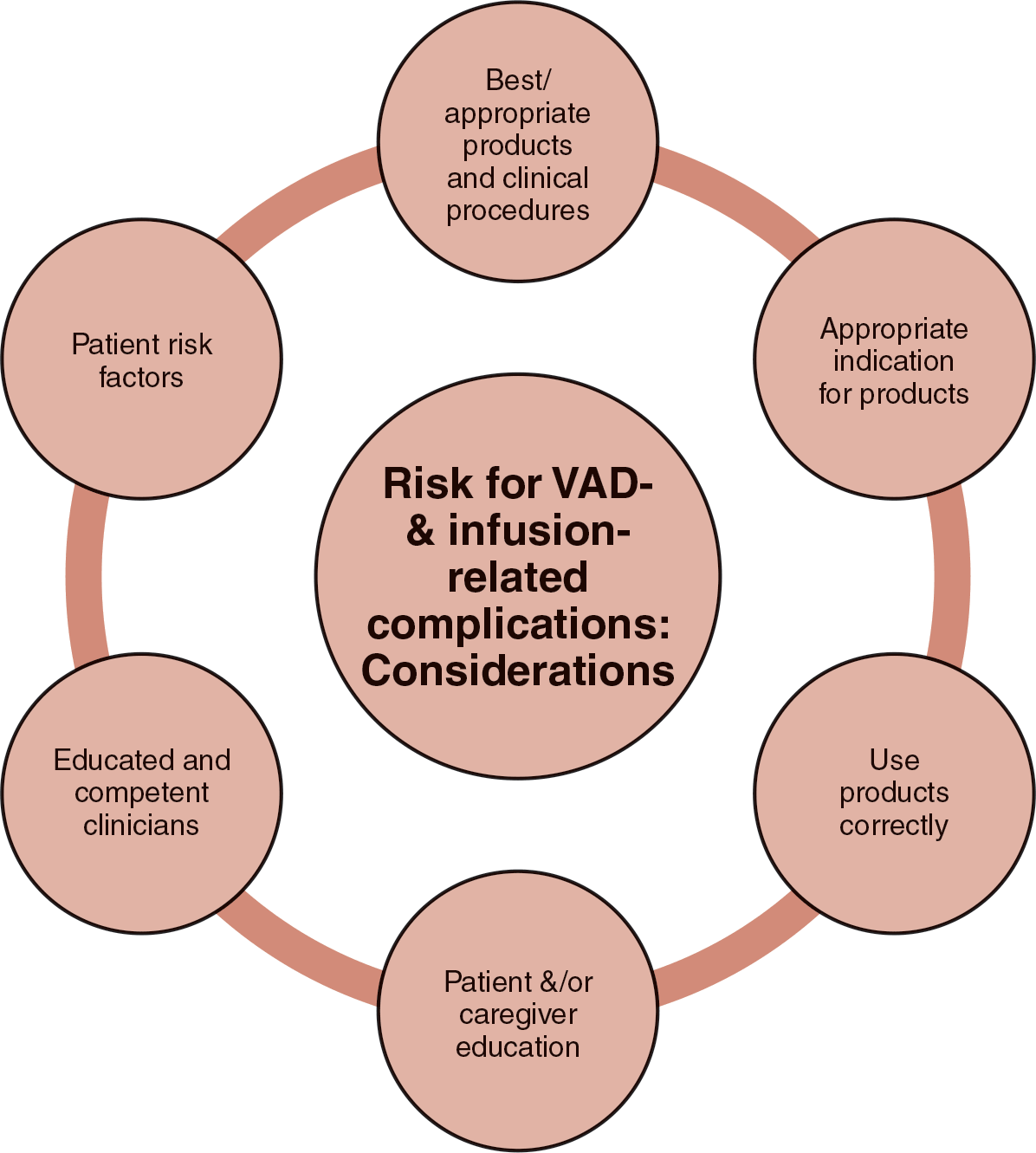
The placement and the presence of a vascular access device (VAD) put patients at risk for complications during both the insertion process and VAD dwell time. Systemic complications such as catheter-associated bloodstream infection (CABSI), air embolism, and circulatory overload are serious and can be life-threatening, yet are preventable when evidence-based prevention and care practices are employed. The impact of some local complications, such as phlebitis or infiltration, is minimized when the nurse provides thorough and frequent assessments, educates the patient and family members, and identifies early signs and symptoms that allow for prompt action. There are numerous factors that affect the risk for VAD-related complications (Fig. 9-1). These include:
- Using appropriate products and clinical procedures in VAD-related care. Considering skin antisepsis, alcohol-based chlorhexidine solution is preferred for infection prevention. However, some patients may have a sensitivity to the solution or to a transparent dressing, resources may be limited, and alternative options must be implemented. Placement of VADs in accordance with procedures that minimize risk is critical, such as adherence to Aseptic Non Touch Technique (ANTT) (see Chapter 2).
- Using products for appropriate indications, such as for the right device and the right patient population.
- Using products correctly. The best product for the appropriate indication may be implemented but must also be used correctly. Examples include proper placement of chlorhexidine dressings, following recommended manufacturer guidance in removal and replacement of securement devices, and appropriate disinfection of needleless connectors (NCs) whether using alcohol wipes, alcohol-based chlorhexidine wipes, or disinfection caps.
- The educated nurse understands potential complications, signs and symptoms, and preventive interventions and employs appropriate interventions in the event of a complication. Given that a number of complications are preventable, nursing knowledge is critical.
- Patient/caregiver education becomes especially critical for those patients living at home with a VAD and perhaps administering their infusions.
- Individual patient risk factors such as skin/vein fragility or lack of ability to respond to or report symptoms may increase risk for complications such as phlebitis or infiltration. It is always important to recognize such risk factors that may result in the need for increased frequency of monitoring.
Figure 9-1 Considerations: Risk for Vad- and Infusion-Related Complications. © Lisa A. Gorski.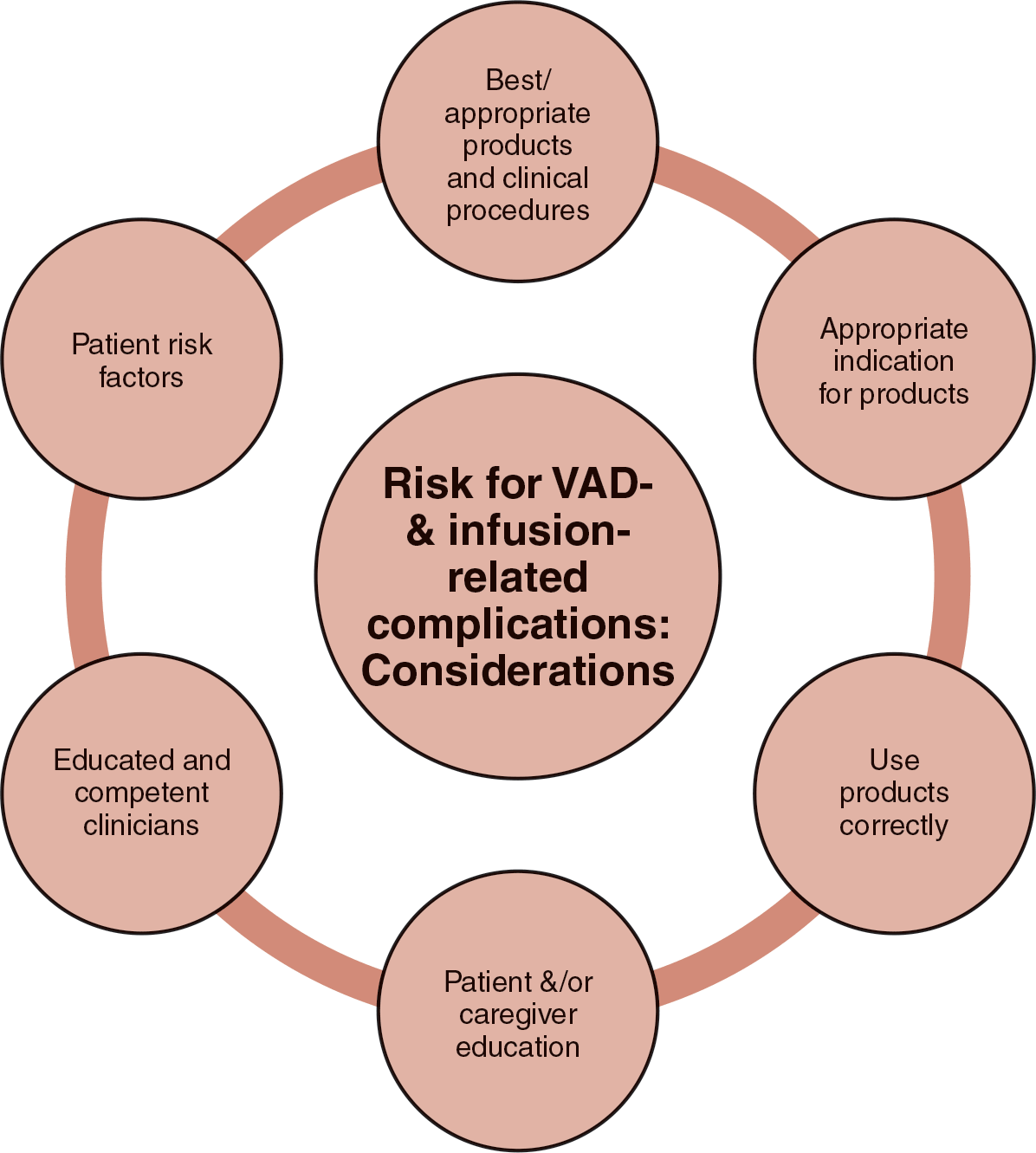
In this chapter, complications are categorized as local, systemic, and central VAD (CVAD) related. The etiology, signs and symptoms, preventive interventions, and treatment are addressed for each complication. Documentation points are also provided.
INS Standard: Vascular access devices are removed when clinically indicated: unresolved complication, discontinuation of infusion therapy, or when no longer necessary for the plan of care (Gorski et al., 2021, p. S133). Clearly complications are prevented when the VAD is removed if no longer needed. Yet in many organizations, a peripheral IV catheter (PIVC) in particular, may be left in place “just in case,” even if the patient is not receiving active infusions and is able to orally hydrate. Unused or “idle” IV catheters are common and are associated with adverse outcomes, including increased risk of infection, intensive care unit admission, and phlebitis (Bercerra et al., 2016; Silk et al., 2021).
The nursing process is a six-step process for problem-solving to guide nursing action (see Chapter 1 for details on the steps of the nursing process). The following table focuses on nursing diagnoses, nursing outcomes classification (NOC), and nursing interventions classification (NIC) for patients with local and systemic complications of infusion therapy. Nursing diagnoses should be patient specific and outcomes and interventions individualized. The NOC and NIC presented here are suggested directions for development of specific outcomes and interventions.
| Nursing Diagnoses Related to Complications | Nursing Outcomes Classification (NOC) | Nursing Interventions Classification (NIC) |
|---|
| Anxiety (mild, moderate, or severe) related to: Stressors (threat to change in health status or situational crisis) | Anxiety level; anxiety level self-control | Anxiety reduction (techniques such as use of a calm, reassuring approach, explaining all procedures) |
| Excess fluid volume related to compromised regulatory mechanism; excess fluid intake; excess sodium intake | Fluid balance, hydration | Fluid monitoring, fluid management |
| Impaired gas exchange related to: Alveolar-capillary membrane changes; ventilation-perfusion imbalance (e.g., pneumothorax, air embolism) | Respiratory status, gas exchange, ventilation | Acid-base management; airway management (monitor blood gases and hemoglobin levels) |
| Pain, acute, related to: Biological injury (e.g., peripheral vascular inflammation, edema, CVAD-associated venous thrombosis); chemical injury (e.g., extravasation) | Pain control | Pain management, analgesic administration |
| Risk for infection related to: Environmental exposure to pathogens; immunosuppression, invasive procedures, altered skin integrity, insufficient knowledge to avoid exposure to pathogens | Risk control: Infectious process, immune status | Infection control; infection protection |
| Protection ineffective related to: Abnormal blood profiles, pharmaceutical agents, extremes of age, treatment regimen | Blood coagulation, immune status | Bleeding precautions, infection prevention, infection protection |
| Skin integrity, impaired, external related to external factors: Presence of a VAD; irritation from IV solution; chemical injury (extravasation, reaction to antiseptic agent, dressing); extremes of age | Tissue integrity: Skin; wound healing | Skin surveillance, wound care, risk identification |
| Decreased cardiac tissue perfusion risk for, related to: Arterial or venous blood flow exchange problems, hypovolemia, decreased systemic vascular resistance related to sepsis | Circulation status,
Tissue perfusion: Cardiac; vital signs | Cardiac care, cardiac precautions, embolus precautions, vital signs monitoring and shock management: Cardiac |
Source: Ackley et al., 2020; Herdman et al., 2021.
 Media Link: Chapter post tests and answers are provided on FADavis.com, along with case studies and critical thinking activities.
Media Link: Chapter post tests and answers are provided on FADavis.com, along with case studies and critical thinking activities.