This chapter discusses the healthcare core competency: apply quality improvement (QI) and the related nursing competency on quality identified by the Quality and Safety Education for Nurses (QSEN). The content in this chapter includes information about the key quality and associated safety reports (Quality Chasm series) and their recommendations. Accreditation of healthcare organizations (HCOs) is also related to the need to improve care. Nurses and nursing as a profession assume major roles in ensuring that care is safe and outcomes are reached, resulting in quality care. Appendix Ais an important resource for this content, providing additional content and terminology to assist in a greater understanding of quality health care. Continuous quality improvement (CQI) requires an effective use of a process as discussed in this chapter. Figure 12-1 provides an overview of the process and introduction to this content.
Figure 12-1 Continuous quality improvement: How do we do this?
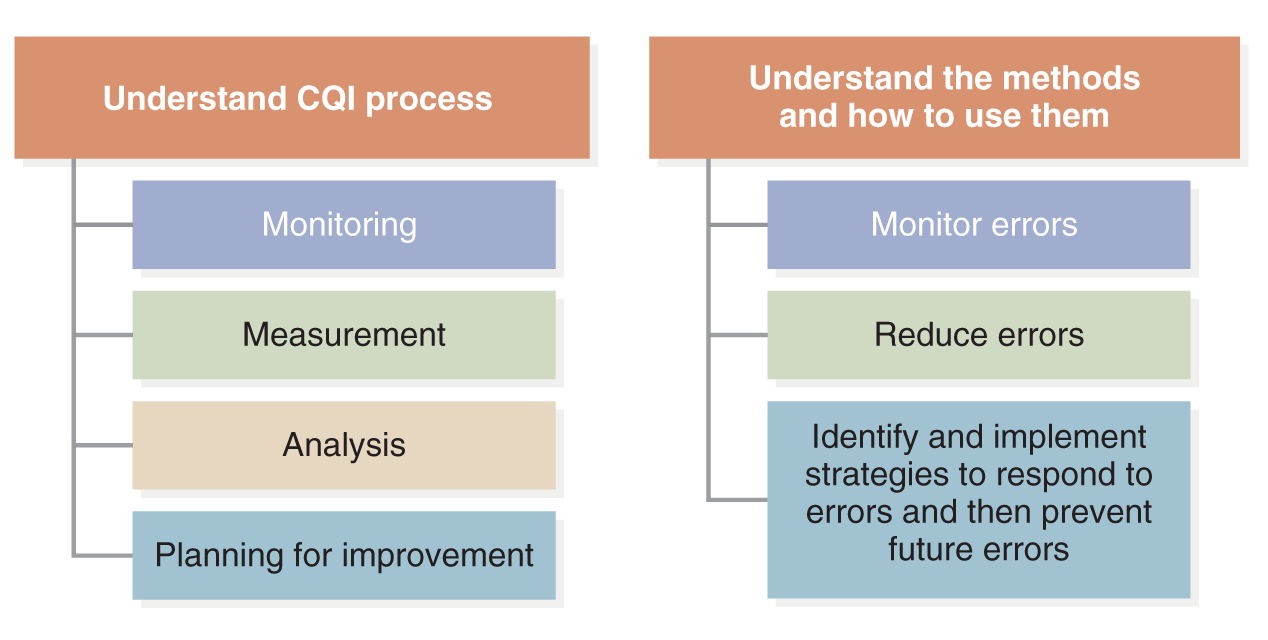
A diagram illustrates the steps for continuous quality improvement.
The left side focuses on understanding the C Q I process, which includes monitoring, measurement, analysis, and planning for improvement. The right side focuses on understanding the methods and how to use them, which includes monitoring errors, reducing errors, and identifying and implementing strategies to respond to errors and prevent future errors.
The Core Competency: Apply Quality Improvement
The competency focuses on applying QI, described as follows: “Identify errors and hazards in care; understand and implement basic safety design principles, such as standardization and simplification; continually understand and measure quality of care in terms of structure, process, and outcomes in relation to patient and community needs; and design and test interventions to change processes and systems of care, with the objective of improving quality” (IOM, 2003, p. 4) and relates to the QSEN (2022) competencies. Figure 12-2 identifies the key elements of this competency.
Figure 12-2 Apply quality improvement: Key elements.
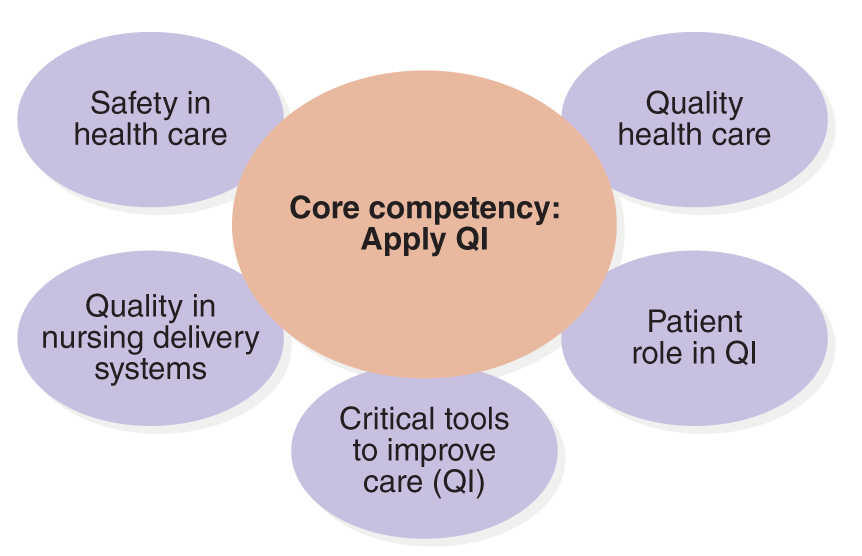
A diagram illustrates the key elements of applying quality improvement.
The Core competency, Apply Q I is in the center. Surrounding it are six key elements: safety in health care, quality health care, patient role in Q I, critical tools to improve care, Q I, quality in nursing delivery systems, and patient role in Q I.
Data indicate that there are serious problems with health care in the United States-its safety, quality, and waste and inefficiency. It is a problem that the U.S. Congress has addressed, indicating its importance to the public. In 2014, the U.S. Congressional Subcommittee on Primary Health and Aging held a meeting to examine healthcare errors: “Preventable medical errors in hospitals are the third leading cause of death in the United States, a Senate panel was told today. Only heart disease and cancer kill more Americans . . . Medical harm is a major cause of suffering, disability, and death-as well as a huge financial cost to our nation,” Senator Bernie Sanders commented. The press release went on to state, “[E]ach year as many as 440,000 people die due to a preventable medical error in hospitals. Compared with other nations, the United States is about average. In addition to deaths and injuries, medical errors also cost billions of dollars. One study conducted in 2011 put the figure at $17 billion a year. Counting indirect costs like lost productivity due to missed workdays, medical errors may cost nearly $1 trillion each year . . .” (U.S. Congress, Subcommittee on Primary Health and Aging, 2014). Experts commented on healthcare quality by noting recent studies supporting these comments-"if we identified errors as a disease then when tracking death rates per disease, errors would be the third leading cause of death in the United States” (Makary, 2016). This is a strong statement, and it had an impact on increasing efforts to improve and recognizing that the federal government is engaged in assessing, describing the problem, and collaborating to improve. The picture is not all bleak as there has been improvement since the report, To Err Is Human, but there has not been enough. The examples provided in this chapter content and in Exhibit 12-1 indicate major problems still exist more than 20 years after the publication of To Err Is Human (IOM, 1999).
| Exhibit 12-1 Examples of Quality Care Issues |
|---|
| The following represent several examples of problems that have occurred in the last few years in HCOs that have had a serious impact on patients and their health outcomes. Some have been resolved, and some are ongoing. |
| National Institutes of Health Clinical Center |
| The National Institutes of Health (NIH) Clinical Center has long been thought of as an exemplary healthcare setting that offers care for unique medical problems and clinical trials for research studies; however, in 2016, there was significant criticism of the clinical center and its care. Leadership at the center disputed the claims of poor quality (NIH, 2022; Kaiser, 2016). The report identified several recommendations for improvement: (1) Fortify a culture and practice of safety and quality; (2) strengthen leadership for clinical quality, oversight, and compliance; and (3) address sterile processing of all injectables and the specifics of the sentinel event that set this review in operation (NIH, ACD, 2016). Since this time, steps have been taken to improve. |
| Veterans Health Administration |
| In 2014, there was extensive reporting of abuse in the Veterans Health Administration (VHA) that focused on putting patients on appointment wait lists for long periods of time, and some were never seen for care. This is poor care, but documentation changes were added to make it look as if there was no problem. The inspector general for the VHA investigated this fraud and unethical actions. In 2016, problems continued in some VHA medical centers-for example, with the inspector general continuing to investigate care and misconduct incidents (Krause, 2016). Examples of other problems were environmental concerns in the operating rooms and fraud and cover-ups that included nurses' involvement (Rebelo & Santora, 2016). |
| A Nurse as a Whistleblower |
| A nurse in an academic health center sued the health center for covering up infections and then limiting the use of standard checking of equipment used in procedures to ensure sterility (Becker's Hospital Review, 2016). If the equipment is not checked, data collected will not identify problems, and performance then appears to be better than it might be. The nurse asked that the procedure for checking equipment routinely be maintained and requested an external audit. The requests were rejected. The nurse sued under the whistleblower law, as discussed in other text content on legal and ethical issues. Employers cannot retaliate for this type of employee action. |
| Lost Newborn Body |
| An academic medical center lost the body of a newborn after death during delivery. This is an unusual situation and is a sentinel event. There are procedures and policies that should be applied when a death occurs in an HCO, including care of the body. This did not happen in this case when a woman delivered twins; one was stillborn, and the second lived an hour (CBS News, 2015; Fieldstadt, 2015). |
| Whistleblower: Visiting Nurse Service Fraud |
| At one of the largest nonprofit home healthcare agencies in the United States, a senior manager filed a whistleblower lawsuit for fraud that resulted in hundreds of millions of dollars taken from Medicare and Medicaid. This fraud included falsified and improper billings. This resulted in many patients receiving a fifth or less of prescribed care. Patients were not told about changes in their service level nor were physicians notified. An example of fraud in this case was a nurse who claimed to have made 20 home visits for nine patients in one day, something that could not have occurred. Other nurses made similar claims of visits that they could not have been made in the timeframe identified. Exhibit 12-2 provides other examples with links to additional information. |
| Exhibit 12-2 Examples of Poor Quality and Safety |
|---|
|
When considering quality and ethics, such as the examples about better staffing, “[m]uch of the public discourse around the hospitals' purportedly unethical behaviors misses an important nuance-namely, that hospitals' staffing decisions are shaped by a complex system of economic and regulatory constraints created and overseen by governmental payment policies and largely replicated by private payers. Improving hospitals' behavior will require changing the policies that currently allow-and even inadvertently incentivize-hospitals to increase their operating margins through inadequate staffing” (Yakusheva & Rambur, 2023). Staffing, budget, and policies have a direct impact on quality and safety in health care. This can be a conflict for HCOs and healthcare providers, as funding, for example, reimbursement, is necessary, and funds must also be used for other expenses, but staffing is critical and costly. Policies and even politics are involved in this complex concern. Nurses are speaking out about their concerns, for example, engaging in a march to push for safer staffing in Washington, D.C. (Minnie, 2022).
| Stop and Consider 1 |
|---|
| Every nurse is expected to meet the QI competency. |
Quality Health Care
In 1970, the Institute for Medicine (IOM) was founded as a private, nonprofit, nongovernmental institution that works to provide objective expert advice and is now known as the National Academy of Medicine (NAM). Its mission is to “advance science, accelerate health equity, and provide independent, authoritative, and trusted advice nationally and globally” (NAM, 2023). Since the late 1990s, there has been an increase in efforts to examine healthcare quality. The NAM is a leader in this effort, consulting with experts, collecting and analyzing data, and publishing reports with recommendations on a variety of topics related to healthcare quality. This series of reports is often referred to as the Quality Chasm reports. The following describes the major initial reports in this series. These are important sources of information for healthcare policy, providers, professional organizations, and healthcare profession education.
To Err Is Human
The first report in the Quality Chasm series was To Err Is Human: Building a Safer Health System (IOM, 1999). This report explored the status of safety in the U.S. healthcare delivery system. The results were dramatic, with data indicating serious safety problems in hospitals. This examination did not include other types of healthcare settings, such as ambulatory care, home health care, long-term care, and other types of sites. More research was needed to provide data about the quality of care and safety in these settings. An example of the influence of this research is the report published by the Agency for Health Research and Quality (AHRQ): AHRQ Health Information Technology, Ambulatory Safety and Quality: Findings and Lessons from the AHRQ Ambulatory Safety and Quality Program. The report described studies about ambulatory care, but the report noted more information was needed to support strong conclusions (HHS, AHRQ, 2022). As discussed in this chapter, an effective understanding of quality requires clear data that are useful for monitoring and measuring healthcare outcomes.
Some of the data from the initial Quality Chasm report that disturbed the public and healthcare providers included the following and set the stage for major initiatives to improve care (IOM, 1999, pp. 1-2):
- When data from one study were extrapolated for the 1999 IOM report, the result suggested that at least 44,000 Americans die each year due to medication errors. To compare the 1999 report data, more recent studies indicate the number of deaths from this cause could be as high as 98,000 (AHA, 2023).
- More people die in a given year as a result of medical errors than from motor vehicle accidents (43,458), breast cancer (42,297), or acquired immunodeficiency syndrome (AIDS) (16,516) (HHS, CDC, NCHS, 1998). Deaths from medical errors continue to be a problem, but research on this issue is complex and requires careful consideration of the methods used.
- Healthcare delivery costs represent more than half of total national healthcare costs, which include lost income, lost household production, disability, and actual healthcare delivery costs (Thomas et al., 1999). Healthcare costs continue to increase.
These examples are no longer current, but they are important in understanding the significance of this report when it was published. Later in this chapter, HCO accreditation is discussed in detail; however, it is important to note that accreditation, focusing on evaluating the quality of care in HCOs, has long been the major method for supporting quality health care. It is clear from To Err Is Human that accreditation was not enough to improve care at the level needed, and as noted in this chapter and text, more needs to be done.
The media took note of To Err Is Human and its recommendations, and soon worrisome stories appeared on the evening news and in newspapers; special in-depth news reports asked, “How safe are you when you receive health care?” Consumers began to ask questions. Healthcare errors experienced by patients and errors reported in the media reduce the public's trust in the healthcare system. The result is that patients and families question their care more. Some patients now want a family member or friend with them when they are in the hospital, not just for support but also to act as a protector from errors. When a patient experiences an error, the patient's trust level drops, and this has an impact on how the patient approaches future care. There is a positive side to this situation. More patients are now demanding that they be informed about their care, and therefore, they are becoming more involved in the care process. Patient/person-centered care (PCC) has developed with this increase in patient concern about quality care. (See Saad reference in Exhibit 12-2for additional information about current consumer views of healthcare.)
When strategies are used to prevent errors and improve care, it is important to recognize there is not a specific single answer to this problem. Changing the status of quality care requires multiple planned strategies in practice and management and an increase in QI education in professional healthcare programs, such as nursing education and staff training.
Crossing the Quality Chasm
Crossing the Quality Chasm (IOM, 2001a) is the report that followed To Err Is Human (IOM, 1999) in the Quality Chasm series. This report's major message was influenced by the 1999 report and indicated that the U.S. healthcare system needed fundamental improvement. Although the healthcare delivery system has undergone many changes-such as the development of new drugs, medical technology and innovation, and healthcare informatics that have improved care and care options-more needed to be done. The 2001 report provided valuable information to help nurses better understand quality issues in the healthcare system; however, if this information is not applied to improve care, it serves little purpose. The report identified six aims or goals for improvement that continue to be relevant. Care should have the following characteristics: safe, timely, effective, efficient, equitable, and patient/person-centered care (STEEEP®) (IOM, 2001a, pp. 5-6). This type of care ensures that patients receive the services they need (effective care), when they need care (timely care), in the most cost-effective manner (effective and efficient care), and that efforts need to be made to prevent problems (safe care) that might occur due to the errors or poor-quality care (quality improvement). As noted in other Quality Chasm reports, healthcare professionals must also recognize diversity and ensure that disparities are limited when care is delivered, and today there is even greater emphasis on supporting health equity or equitable care. The critical element that connects all of this is health care, which is focused on the patient/person with the patient participating in the care process, PCC. Healthcare competencies relate to STEEEP®, and these aims continue to be viewed as critical healthcare delivery elements (IOM, 2003).
The Quality Chasm series is unique in that the reports do not stand alone but rather expand on previous reports in the series. This interconnectedness makes it important for readers to understand the general information in each report, the ways in which the reports relate to one another, and the recommendations and joint implications for nursing and health care. For example, STEEEP® is related to all the reports and is now a central feature in HCO QI programs. It is also included in national QI initiatives to better ensure continuous quality improvement.
To ensure improved healthcare, the system needs to meet the six aims identified in the Crossing the Quality Chasm report. New rules for the 21st century were developed to guide healthcare delivery, describing a vision of health care. The rules focused on various aspects of care as noted here with some comments about their relationship to nursing practice (IOM, 2001a).
- Health needs are not static, and care must change to meet them, providing a continuous experience. Consider these factors and examples: the nurse-patient relationship, continuum of care, collaboration and coordination, HCO services and systems, diversity, interprofessional teams, communication, and nursing standards.
- Patients are individuals requiring care to match their needs: patient/person-centered care. Patient needs and values also constitute one of the sources of evidence for evidence-based practice. Consider these factors and examples: nursing care and planning, interprofessional teams, PCC, collaboration and coordination, diversity and health equity, patient rights, and patient education, all of which relate to nursing standards and the nursing code of ethics.
- Patients need information to make decisions about their own care-this is essential to patient/person-centered care. The healthcare system and professionals need to share information with patients and bring patients into the decision-making process. Consider these factors and examples: plan of care, interprofessional care, and informed consent provide information for the decision maker, privacy and confidentiality, patient education, patient rights and professional ethics, and informatics.
- Patients need access to their medical information, and clinicians also need access-sharing information when needed. This rule relates to all healthcare competencies, particularly to applying informatics. Consider these factors and examples: informatics, interprofessional teams, sharing information in the nursing care process, patient/person-centered care, privacy and confidentiality, patient education, computerized documentation, professional ethics, and standards. As discussed in this text, digital health (telehealth/telemedicine) is an expanding area of health care. The COVID-19 pandemic increased the use of digital health and the need to share information electronically when patients and healthcare providers had limited physical interaction.
- Patients need care that is based on the best possible available evidence. Care should not vary illogically from clinician to clinician or from place to place. Consider these factors and examples: PCC, nursing research and other areas of research, research-informed consent, EBP, and plan of care.
- Patients need to be safe from harm that may occur within the healthcare system. More attention needs to be placed on system errors rather than just individual errors. Consider these factors and examples: PCC, CQI, nursing care provided in a safe manner, inclusion of safety in the plan of care, patient safety and errors, types of errors, staff safety, culture of safety, and reimbursement (for example, Medicare limits reimbursement if a patient experiences a fall in the hospital).
- The healthcare system should make clear and timely information available to patients and their families that allows them to make informed decisions when selecting a health plan, hospital, or clinical provider or when choosing from recommended treatment options. This should include information that describes the system's performance on quality, EBP, and patient satisfaction. Consider these factors and examples: interprofessional teams, informatics, privacy and confidentiality, patient values and preferences, informed consent, research, patient education, report cards, ethics and standards, and national reports on quality and disparity.
- Healthcare providers and the health system should not just react to events that may occur with patients but should anticipate patient needs and provide needed care. Consider these factors and examples: assessment, interprofessional teams, nursing care process, plan of care, collaboration and coordination, HCO services, patient satisfaction, diversity, and outcomes.
- Resources should not be wasted-including patient and staff time. Consider these factors and examples: use of resources for care delivery, costs of care, access to care and services, staff communication, and issues of misuse , overuse , and underuse .
- Collaboration, coordination, and communication are critical factors that determine effective healthcare professionals and systems (interprofessional teamwork). Consider these factors and examples: interprofessional team plan of care requires team collaboration and coordination.
These rules provide a vision of what healthcare delivery should be if we are to ensure quality care for all. They provide nurses with a guide in developing improvement initiatives and strategies. We continuously work to meet these requirements when care is provided to individuals, families, populations, and communities.
Envisioning the National Healthcare Quality Report
Envisioning the National Healthcare Quality Report (IOM, 2001b) is the follow-up report to Crossing the Quality Chasm (IOM, 2001a). The United States did not have a structured method to monitor and measure healthcare quality, but this report recommended changes to resolve this problem. It described a framework for collecting annual national data about healthcare quality and focused on the U.S. healthcare delivery system's performance in providing personal health care. The Agency for Healthcare Research and Quality (AHRQ) is now mandated to collect data using this framework and then publish an annual report describing the status of U.S. healthcare quality, which is made available on the internet. This has provided the United States with a structured monitoring and measurement method and regular reporting of data and analysis. Elsewhere in this chapter, healthcare report cards are discussed. An annual national report card, such as the AHRQ report, does not replace the need for individual HCOs to monitor their own quality, such as by using an HCO-specific healthcare report card. The information from the national annual report card can be used by HCOs in comparing their QI data with national data and then use this information to further develop effective services. Healthcare professionals (providers), insurers, and health policymakers should review this information routinely to better understand current healthcare quality and consider strategies to improve it. Nurse educators should use this information in planning curriculum and teaching-learning strategies to ensure that students are prepared to practice effectively based on current needs.
Because the quality report and the national disparities report, which was also the responsibility of the AHRQ, were interrelated, in 2010 they were merged into one report, the National Healthcare Quality and Disparities Report (NHQDR) (HHS, AHRQ, 2011). This report is designed to meet the following needs: use measurement based on best methods; identify issues that improve or act as barriers to quality care; collect data about care quality and disparities; educate the public, healthcare professionals, organizations, and so on about quality care and disparities; assist policymakers in improving care and reducing disparities; identify key benchmarks; compare U.S. health care with other countries; continue to improve measurement so that data are available and useful; examine healthcare issues that might affect quality of care and disparities; and report data and results. The annual report tracks outcomes for the priority areas of care and health equity and adjusts priorities based on annual results.
We now have more than 10 years of data from these monitoring reports, and the reports influence decisions made about health policy and QI. Because it takes time to collect and analyze data, the published reports are typically one to two years behind the current year. The monitoring methods used to collect and analyze the data are reviewed periodically to ensure their usefulness and the quality of the data, resulting in changes in this report process. The current NHQDR can be accessed at the AHRQ's website (HHS, AHRQ, 2023a).
Defining Quality Health Care
There is no universal definition of healthcare quality, which makes it difficult to assess quality. For this discussion, the following definition and other information provided here will be used in this chapter and applied in other chapters: the “degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (IOM, 1990, p. 4). Quality is a complex concept, and who is defining it can make a difference; for example, a nurse, a physician, and a patient may have different definitions of quality. The following and Figure 12-3 identify the three elements described as having long been included in discussions about quality care and monitoring care (Donabedian, 1980).
Figure 12-3 Three elements of quality.
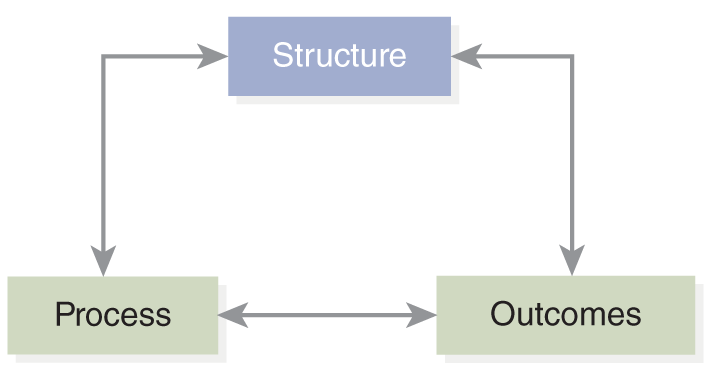
A diagram depicts the three elements of quality: structure, process, and outcomes, with arrows indicating their interconnections.
- Structure: The environment in which services are provided; inputs into the system, such as patients, staff, and environments.
- Process: The manner in which services are provided; the interactions between clinicians and patients.
- Outcomes: The results of services; evidence about changes in patient's health status in relation to patient and community needs.
A recent study examined the current relevance of the Donabedian model and indicated the model continues to be relevant in QI activities (Pogorzelska-Maziarcz et al., 2023). The study included 3,027 participants with 68% reporting that the number of patients assigned to each staff impacted how the staff were able to apply protocols. This is part of the structure element. Other factors were included in the assessment of the impact of structure, such as inadequate staffing, weakness in staff expertise, and inadequate resources. The process element included processes related to following safety protocols, assessment, and surveillance, PPE equipment and isolation policies, limitations in maintaining isolation, the need to prioritize and cluster care, and identifying and limiting staff who should be in certain areas of care. In examining the third element, outcomes, participants (staff) indicated that they felt inadequate staffing and high patient acuity led to adverse patient and staff outcomes. The study concludes: “These findings highlight the need for health care organizations to support frontline nursing staff in adhering to patient safety and infection prevention and control protocols during times of crises. Infection preventionists have substantial contact with bedside nurses and should leverage their collegial relationships to promote patient safety” (Pogorzelska-Maziarz et al., 2023, p. 1399). The application of this model in HCO QI is very common, and this approach has proven to be helpful.
| Stop and Consider 2 |
|---|
| It is not easy to define quality health care. |
Safety in Health Care
Safety is a critical component of quality care. It is important to recognize the relationship between safety and quality because it is easy to assume that safety is something different from quality care rather than to view it as an integral component of QI. An effective HCO QI program monitors all aspects of quality so that safety for patients and staff is included. There is no question that healthcare providers, including nurses, have long been concerned about providing safe care for their patients. If one interviewed healthcare providers, they would say that they want to keep their patients safe. This belief was somewhat shattered when the U.S. Congress and President Clinton's Advisory Commission on Consumer and Quality in the Healthcare Industry requested that the IOM initiate an examination of healthcare safety and make recommendations based on its findings, resulting in the report To Err Is Human (IOM, 1999). In the following content, we explore the topic of safety in healthcare quality: what it is and what can be done to better ensure safe care for all.
It is also important to recognize that healthcare quality, including safety, is a global concern. “Every year, large numbers of patients are harmed or die because of unsafe health care, creating a high burden of death and disability worldwide, especially in low- and middle-income countries. On average, an estimated one in 10 patients is subject to an adverse event while receiving hospital care in high-income countries. Available evidence suggests that 134 million adverse events due to unsafe care occur in hospitals in low- and middle-income countries, contributing to around 2.6 million deaths every year. According to recent estimates, the social cost of patient harm can be valued at US $1 trillion to 2 trillion a year” (WHO, 2021). WHO's action plan on global health safety focuses on the maximum possible reduction in avoidable harm due to unsafe health care globally and supports a safety culture within healthcare organizations using a systems approach with effective leadership.
Critical Safety Terms
The IOM's work on healthcare quality expanded knowledge about safety and errors, in part by undertaking the identification and definition of key terms. This development of common terminology is an important step in addressing the issue. To effectively collect and analyze data nationally requires a shared terminology. Appendix Aprovides definitions for additional critical terms. The following terms are part of this effort. They have relevance for nurses who should be directly involved in care improvement initiatives in HCOs, at the individual healthcare professional level, and in health policy (IOM, 1999; Chassin & Galvin, 1998).
- Safety: Freedom from accidental injury. Example: The patient leaves the hospital after surgery and a three-day stay with no complications, meeting expected outcomes.
- Error: The failure of a planned action to be completed as intended or the use of the wrong plan to achieve an aim. Errors are directly related to outcomes. There are two general types of errors: error of planning and error of execution. Errors may harm the patient, and some, but not all, errors are preventable. Example: The patient is given the wrong medication.
- Adverse event: An injury resulting from a medical intervention; in other words, an injury that is not a result of the patient's underlying condition. Not all adverse events are caused by errors, and not all are preventable. These events require greater examination and analysis to determine the possible relationship between the error and an adverse event. When an adverse event is the result of an error, it is considered a preventable adverse event. Example: A patient is given the wrong medication and experiences a seizure. If the patient does not have a seizure disorder, this is more likely an adverse event, but much more needs to be known about the cause(s). How did the error that led to the adverse event happen? The following factors increase the risk of medication adverse events in the future: the development of new medications, the discovery of new uses for older medications, inadequate patient education and health literacy, health equity, aging of the U.S. population, more over-the-counter medications, and greater use of medications for disease prevention.
- Misuse: Avoidable complications that prevent patients from receiving the full potential benefit of a service. Example: The patient receives a medication that is not prescribed and conflicts with the patient's allergies; the patient experiences anaphylaxis.
- Overuse: The potential for harm from the provision of a service exceeds the possible benefit. Example: An elderly patient takes several medications prescribed by different healthcare providers who do not know all the patient's medications.
- Underuse: Failure to provide a service that might produce a favorable outcome for the patient. Example: The patient is not able to get specialty service needed for cancer because of distance from the healthcare provider, or the patient's insurer will not cover a medication for arthritis that could make the patient more mobile.
- Near miss: The recognition of an event that might have led to an adverse event. This does not mean an error occurred, but rather, it almost occurred. It is important to understand these errors because they provide valuable information for preventing future actual errors. Example: The surgical team is preparing for surgery to repair a patient's knee. The right knee is prepped, but soon after, the team checks the records and goes through a safety checklist prior to beginning surgery, the call-out and check-back, to ensure that the correct knee is exposed-only to find out that it is the left knee that requires surgery. The team stops and considers changes in the plan for the surgery. If there is no consideration of why this error almost happened, then the team cannot learn from it and, hopefully, prevent future errors. One model for understanding near misses and prevention of future errors is the Eindhoven model (van der Schaaf, 1992), which was adapted by nursing and continues to be used to identify three sources of errors (Henneman & Gawlinski, 2004, p. 196):
Technical failure (system error): Physical items, such as software, equipment, or other materials, are not designed correctly, work incorrectly, or are not available when needed.
Organizational failure (system error): This type of error relates to complex factors that affect how work is carried out in the healthcare setting, such as staff orientation, staff expertise, protocols, policies and procedures, clinical pathways, management priorities, budget, and organizational culture.
Human failure: This failure results from behaviors related to skills, rules, and knowledge. Safety mechanisms should include reliable system defenses and the availability of adequate human recovery. Human intervention, such as interventions provided by nurses, can prevent adverse outcomes even when high-risk incidents develop into error incidents.
- Sentinel event: This type of event causes a serious negative patient outcome (unexpected death, serious physical or psychological injury, or serious risk). Example: A patient commits suicide while in the hospital for treatment of diabetes.
If the examination of healthcare quality had concluded with the To Err Is Human report, the major impact of the report and its recommendations would most likely have been diluted (IOM, 1999). This, however, did not happen. In 2004, due to the recognition that much more needed to be known about healthcare quality, follow-up reports were published. The IOM used the following approach to develop the Quality Chasm report series and continues to use it for other reports. A team of experts is identified, and with IOM/NAM staff support, the team (1) describes the problem using data; (2) after analysis, identifies recommendations to respond to the problem(s); and (3), if needed, identifies monitoring methods and possible interventions or solutions. For example, this approach was used to develop the report Patient Safety: Achieving a New Standard for Care (IOM, 2004a) focusing on the need to establish a national information infrastructure and the need for data standards. These elements help healthcare providers and payers improve monitoring outcomes. Having a common language/terminology to use in discussions about safety and errors is critical in meeting the goal to develop a national information infrastructure to support monitoring of care. It also addresses quality improvement competency, which focuses on informatics. This is another example that illustrates how the reports, data, recommendations, and methods used to monitor change are all interconnected. As discussed later and in other chapters, there are now major initiatives that respond to the concerns noted in the Quality Chasm reports and other reports that followed the initial series.
A Culture of Safety and a Blame-Free Work Environment
The typical HCO approach to errors in health care has been to identify the staff member who is thought to have made the error, supported by requiring staff to complete incident reports that describe errors. This type of approach is often punitive in nature and has not been effective in reducing errors, as noted in the IOM's 1999 report. It has not been effective because most errors are not made by an individual but rather are complex and most likely system errors. When an error occurs, the question should not be, who is at fault? but rather, why did our defenses fail? (Reason, 2000). Communication, collaboration, and coordination; interprofessional teamwork; staffing levels and expertise; staff knowledge; patient acuity level; equipment and training to use equipment; delivery processes; the patient's role; and many other factors affect actions taken or not taken in health care. The healthcare system has focused on the “blame game” and not on designing and using structured methods to find out more about all the factors related to an error. Staff members need to feel comfortable-not fearful-reporting errors. This may require providing staff with structured assertive communication training (Chen et al., 2023). The goal now should be developing a blame-free environment or a culture of safety in which staff can practice and openly discuss potential errors or near misses and actual errors. If staff members worry about implications, such as possible impact on their position or performance evaluation, they may not report an error. This can have serious consequences for patients and prevent the system from improving. This type of fear may also prevent staff from communicating near misses, from which much can be learned about potential errors. In the past, if a nurse made a medication error, the nurse might have been routinely required to take a medication review course and a quiz on medication administration with no consideration of analyzing the causes of the error. The following are examples of questions that are important to consider when a medication error occurs in an HCO that supports a culture of safety, demonstrating the complexity of an error situation:
- What are the key questions we should consider in this situation?
- Was the order or prescription transcribed correctly?
- Was the order the best choice for the patient and the patient's problem?
- Was an error made in what the prescriber (physician, advanced practice nurse) intended to order or what the team agreed would be the best approach?
- Was the correct medication sent by the pharmacy? Correct dose? The correct method of administration? Correct time identified and frequency?
- Did the error involve placing a patient medication in the wrong patient's medication box?
- Was the wrong medication and/or dose prepared for administration? Was the administration method incorrect? Was the time or frequency incorrect?
- Was there an equipment malfunction (for example, intravenous equipment, monitoring equipment)? Was the equipment used incorrectly? Was there a computer error? Did the computer send out an alert if set to do so, and if done, why was it not followed?
- What were the distractions and interruptions when the medication was prepared and administered?
- Was the staff member who prepared the medication for administration the same staff member who gave the medication to the patient? If not, why not?
- Were monitoring guidelines followed (for example, vital signs checked)? If data indicated certain actions should be taken, were they taken? If not, why not?
- Was the patient's identification reviewed correctly?
- Was the mediation administration documented as described in the expected procedure?
To accomplish the goal of moving to a culture of safety, there must be (1) a greater understanding of its essential elements, (2) a decrease in barriers to creating the culture, (3) the development and implementation of strategies to create the safety culture, and (4) evaluation of outcomes (IOM, 2004b). Hospitals and other HCOs are moving toward cultures of safety, but it takes time and effort to change staff and administration attitudes and behaviors. It is particularly important to have effective HCO leadership that guides and supports the development of a culture of safety (Anderson, 2006). Trust is important in this type of culture-staff must trust management and vice versa. A topic that comes up often from all types of healthcare professionals is concern about revealing errors and near misses. This is based on past experiences. Moving away from blame means that staff members must trust that they will not be automatically blamed or punished for errors that are out of their individual control. Another aspect of this issue is related to individual staff expectations; nurses may feel that they should not make mistakes and that the care they provide should be perfect. Errors, however, will inevitably occur and are caused by many factors. Improvement is, of course, critical, but to think that errors will never occur is unrealistic. There is no doubt that the number of errors needs to decrease, and what has been done to address errors has not yet been fully effective. Disclosure of errors with maximum transparency must also be used. Ensuring transparency and involving patients are the most difficult aspects of ensuring a culture of safety (Anderson, 2006). “A fundamental principle of the systems approach to error reduction is the recognition that all humans make mistakes and that errors are to be expected, even in the best organizations” (Reason, 2000, p. 768).
It is important to note that a no-blame culture of patient safety does not mean a lack of individual accountability (Wachter & Pronovost, 2009). Though there is now greater emphasis on the recognition of the impact of the system on errors, nurses and other healthcare providers are still accountable for their own practice. When an individual staff member fails to adhere to a safety standard that one is expected to know and apply, and there are no system issues for this failure, then an individual staff member may be accountable for the error. Reporting is an important component of professional accountability. This means healthcare professionals recognize the importance of QI and are committed to active participation in the QI process. Despite these reports, data, and initiatives to improve care and respond to errors-for example, with checklists to ensure that the correct side or body part is operated on in surgery-major problems persist. The Joint Commission reports that wrong site, wrong procedure, and wrong patient (WSPEs) continue to be major problems, representing the most frequently reported sentinel event, and these problems are now the focus of its Universal Protocol to prevent these problems (The Joint Commission, 2023a). QI requires active engagement from all stakeholders to ensure that this type of intervention is used effectively (HHS, AHRQ, PSNet, 2019f).
The HHS, through the AHRQ, is also very involved in supporting safety; for example, it “established the National Action Alliance to Advance Patient Safety as a public-private collaboration to improve both patient and workforce safety. The National Action Alliance is a partnership between HHS and its Federal agencies and private stakeholders, including healthcare systems, clinicians, allied health professionals, patients, families, caregivers, professional societies, patient and workforce safety advocates, the digital healthcare sector, health services researchers, employers, and payors interested in recommitting our Nation to advancing patient and workforce safety to move toward zero harm in healthcare. The HHS recognizes that now is the right time to recommit to advancing patient safety. Progress in safety has been challenged in recent years, by a variety of factors, most notably the COVID-19 pandemic that revealed weaknesses and inequities in the healthcare delivery system. As health systems emerge from the pandemic, their efforts to recover and improve patient care will face competing priorities, including improving equity, addressing staffing shortages, caring for people with Long COVID, harnessing the potential of telehealth and data sciences, responding to climate change, expanding access to behavioral healthcare, and supporting workers' well-being. Addressing these challenges rests on a foundation of patient and workforce safety that requires system solutions” (HHS, AHRQ, 2023b). This action alliance is based on four foundational areas of (1) culture, leadership, and governance; (2) patient and family engagement; (3) workforce safety; and (4) creation of learning health systems, which is described later in this chapter.
The AHRQ as an active part of HHS also provides resources for healthcare providers and organizations to support patient safety. The Network of Patient Safety Databases (NPSD), as described in Figure 12-4 . This was established by the Patient Safety and Quality Improvement Act of 2005, and the focus is on evidence-based management resources. The NPSD is also associated with the National Healthcare Quality and Disparities Report.
Figure 12-4 Network of Patient Safety Databases.
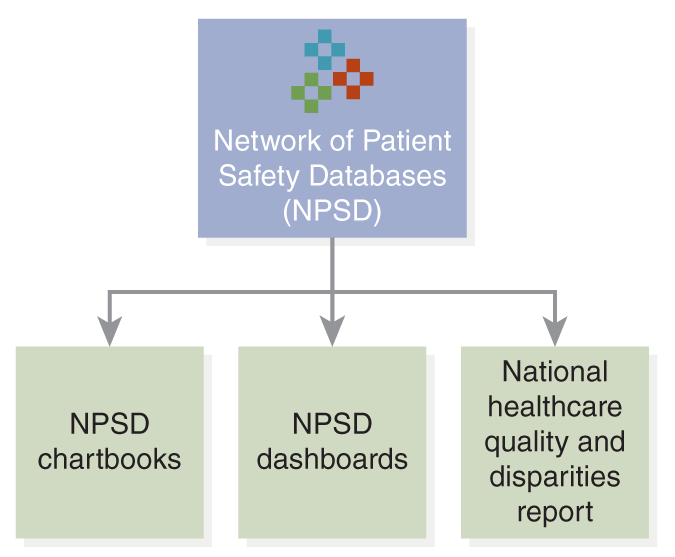
A block diagram of the Network of Patient Safety Databases.
The main block labeled Network of Patient Safety Databases, N P S D, branches out into three blocks: N P S D chartbooks, N P S D dashboards, and National healthcare quality and disparities report.
U.S. Department of Health and Human Services. Agency for Healthcare Research and Quality. (2023). https://www.ahrq.gov/npsd/what-is-npsd/index.html
Root cause analyses of WSPEs consistently reveal communication issues as a prominent underlying factor. The concept of the surgical timeout-a planned pause before beginning the procedure to review important aspects of the procedure with all involved personnel-was developed to improve communication in the operating room and prevent WSPEs. The Universal Protocol also specifies the use of a timeout prior to all procedures. Although initially designed for operating room procedures, time-outs are now required before any invasive procedure. Comprehensive efforts to improve surgical safety have incorporated timeout principles into surgical safety checklists; while these checklists have been proven to improve surgical and postoperative safety, the low baseline incidence of WSPEs makes it difficult to establish that a single intervention can reduce or eliminate WSPEs (HHS, AHRQ, Patient Safety Network [PSNet], 2019a).
Some of these errors in surgery are difficult to prevent, and some may occur before the patient reaches surgery. For example, consider what happened before surgery to a patient who was scheduled to have cardiac bypass surgery. When the nurse asked the patient to sign the consent form, it listed a different procedure. The patient, who was a physician, pointed out the error and refused to sign. Half an hour later, another nurse brought the patient another consent form to sign, but it was also incorrect. The third consent form was correct and then signed by the patient. This should never happen. What if the patient had not noticed or did not have the background to understand that the surgical procedure described was not what was agreed on between the physician and the patient? This experience also took staff time and increased stress for the patient and family just prior to surgery. Patient trust in staff was significantly reduced at a critical time of stress. This same patient experienced several critical near misses post-surgery with intravenous medications that could have led to cardiac arrest if the patient had not noticed the errors and told the nurse to stop giving the medication immediately, an error that was repeated the next day. When the patient left the hospital, he said, “What has happened to nurses? I have worked with them for years, but their practice has gone downhill. I could have been killed in there.” This highlights the need to improve care, and changing the culture is much more complicated than thought.
It is important to recognize that some HCOs continue to have blame cultures, and more attention should be given to the personal reaction of staff involved in errors, particularly errors that lead to the risk of patient death. How much debriefing occurs after an error, are staff blamed, and in what way? For example, in 2011, a neonatal nurse with 24 years' experience was involved in a medication error that led to the death of an eight-month-old baby; although at the time, it was not clear the error was the actual cause of the death. Immediately after the incident, the nurse was escorted from the hospital, put on administrative leave, and then fired several weeks later. Seven months later, the nurse committed suicide. For more than 3 years, the hospital in which this event occurred described itself as using the “just culture” approach, but this example does not demonstrate this type of culture (Aleccia, 2011). The HHS provides information on support staff who are second victims when errors occur (HHS, AHRQ, PSnet, 2019b). Does this incident send a message to staff not to mention errors? How effective was the organization's just culture-was it just something described in documents but not really practiced? How can employers help staff so that the staff does not become secondary victims if they cannot cope well after an error? Staff emotional distress after an event is not uncommon. In a survey of 3,000 physicians in the United States and Canada, 92% reported experiencing an adverse event, and of those physicians, 81% reported some job-related stress associated with the adverse event that can lead to burnout and low professionalism (Panagiote et al., 2018). Recovery requires time, but it is critical that HCOs maintain an environment of support and offer the provider assistance. Getting support from peers is also important, such as other staff offering to help so that the staff member can have a break from work responsibilities immediately after an adverse event and time to talk about the event in an environment that is not threatening.
The establishment and maintenance of an effective culture of safety requires leadership. This is so critical that The Joint Commission published a sentinel event alert entitled: The Essential Role of Leadership in Developing a Safety Culture (2021). This alert recognizes that when leaders in HCOs do not create an effective culture of safety, this may result in adverse events. The sentinel alert notes that leadership is needed for effective support of event reporting and provide feedback to staff and others who are reporting safety concerns, promote an environment in which staff who report events are not intimidated, use the reporting data to improve, and alert management to staff burnout. This type of leader supports a just culture with appropriate actions to ensure a reporting and learning culture at all levels of the organization. Reducing adverse events can be more effective by using a structured approach, such as the Global Trigger Tool (developed by the Institute for Health Improvement), which is used to assess the overall harm in an HCO. It focuses on monitoring three measures (Griffin & Resar, 2009; AHA, 2023):
- Adverse events per 1,000 patient days
- Adverse events per 100 admissions
- Percent of admissions with an adverse event
Students also have a need for support if an error occurs. It is important that students who are involved in a near miss or an error discuss the experience openly with faculty and ask for support. However, faculty should proactively provide support to students when these situations occur or get qualified persons to assist the student. If this is not done, it reinforces a blame culture-schools of nursing need to also establish cultures of safety or just cultures (Penn, 2014). As we move toward a system view of errors, factors described in Figure 12-5 support a culture of safety.
Figure 12-5 System-level factors that affect safety.
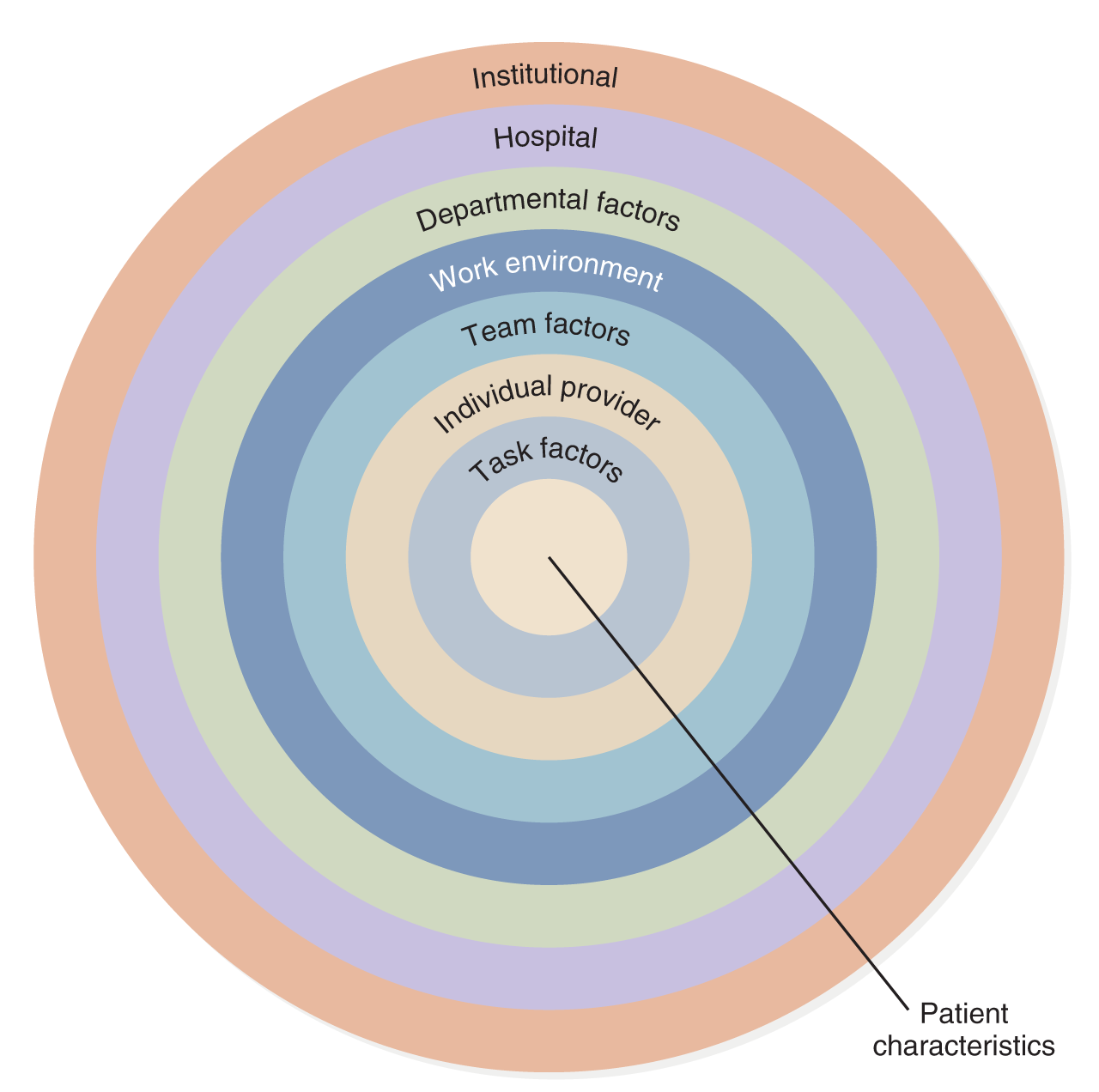
A concentric circle diagram illustrates patient safety factors.
The outermost circle is labeled Institutional, followed by hospital, departmental factors, work environment, team factors, individual provider, and task factors. At the center of the diagram is a line pointing to patient characteristics.
Understand the Science of Safety. Content last reviewed July 2018. Agency for Healthcare Research and Quality (AHRQ). https://www.ahrq.gov/hai/cusp/modules/understand/science-safety-notes.html
Staff Safety
To Err Is Human focused on patient safety, not staff safety, but the report also states: “Creating a safe environment for patients will go a long way in addressing issues of worker safety as well” (IOM, 1999, p. 20). The lack of information about staff safety in this report does not mean staff safety is not important-it is very important. Another report, Keeping Patients Safe: Transforming the Work Environment of Nurses (IOM, 2004b), included content related to staff safety, particularly related to nurses. Nursing staff members are not immune to workplace injuries. The Occupational Safety and Health Administration (OSHA) is the federal agency that is responsible for monitoring safe workplaces and provides guidance and resources to ensure workplace safety, including healthcare work settings. The American Nurses Association (ANA) is a strong advocate of safety for nurses in all types of healthcare settings. Its position statements on staff safety provide guidelines for healthy work environments. Examples of some of the position statements are available on the ANA website, such as Personnel Policies and HIV in the Workplace, HIV Infection and Nursing Students, HIV Testing, workplace violence and incivility, bullying, and others. Some of the key safety issues for nursing staff other than those mentioned are highlighted here. These statements can be accessed at the ANA website (2023a).
- Needlesticks: Since the 1990s, there has been a reduction in these events due to the application of strategies to reduce them, but they are still a problem. The greatest decreases have been in injuries associated with disposable syringes and winged-steel needles (butterflies) due to advances in safer technologies. However, injuries from sutures and scalpel blades, especially among physicians, continue to be high. Injuries from disposable syringes continue to affect nurses more than any other single professional group (53%). In addition, year after year, approximately 25% of all injuries occur downstream to the nonuser (e.g., waste management staff, laundry worker, etc.). It is important to remember that the use and activation of safety mechanisms and proper disposal protect not just the user of the device but those who encounter the device throughout its lifespan or the procedure (HHS, CDC, NORA, 2019).
- These exposures can lead to hepatitis B, hepatitis C, and human immunodeficiency virus (HIV), the virus that causes AIDS. At least 1,000 healthcare workers are estimated to contract serious infections annually from needlestick and sharps injuries. More than 80% of needlestick injuries can be prevented with the use of safer needle devices, but HCOs must provide them-and nurses need to demand that they are available and use them.
- Infections: As noted, healthcare workers are often exposed to communicable diseases via needlesticks. Other examples of infections staff may be exposed to include tuberculosis, Staphylococcus, cytomegalovirus, influenza, and bacteria. Influenza spread has been linked to suboptimal vaccination levels of healthcare workers; for example, in “2019-2020 flu vaccination coverage among healthcare personnel (HCP) was 80.6%, similar to coverage during the past five seasons (77.3% -81.1%)” (HHS, CDC, 2020). The CDC recommends that healthcare workers in hospitals and long-term care receive the vaccine annually. Some states require this immunization for state employees in healthcare and/or require reports to the state on levels of staff immunization. In states with requirements, employees may submit exemptions, and if they do not get the vaccine, they may be required to wear masks while at work. COVID-19 has clearly reminded the healthcare delivery system and healthcare professionals of the risk of infectious diseases, and this, too, has led to immunization concerns and further issues related to staff requirements. It is hoped that all healthcare providers receive new vaccines and subsequent updates for infectious diseases to protect themselves, their families, other staff, and patients. Another recent infectious disease is the Ebola virus that spread from Africa and the Zika virus, transmitted by mosquitos but not contagious in the work environment unless the nurse is working in an area where the infected mosquitos exist. These situations are examples of the global impact of infectious diseases today; people travel globally, and healthcare providers travel to assist other countries in providing health care for emergencies and on a routine basis. As seen with COVID-19, infectious diseases can directly impact travel, how it is done, when, changes in procedures, and who may travel and have a global economic travel impact.
- Ergonomic safety: Nurses experience a significant number of work-related back injuries and other musculoskeletal disorders. Because of these injuries, some nurses may request transfers to other units or other healthcare settings with less risk, and sometimes they may leave nursing. Typical injuries are to the neck, shoulder, and back. Nursing practice requires a lot of patient handling, and factors, such as the patient's weight, height, body shape, age, dependency, and medical status are important ergonomic issues. There has been an increase in weight in the U.S. adult population in general, and this has increased the risk of injury. The physical workspace is also a factor in increasing risk. There should be enough space to provide care and allow staff to safely move the patient. Nurses should consider the types of available equipment to assist in moving patients, request assistance when needed, and discuss their work needs with management, noting the importance of these factors in ensuring quality care and staff and patient safety. The ANA's “Handle with Care” campaign addresses work-related musculoskeletal disorders (ANA, 2023b). Its goal is to develop and implement a proactive, multifaceted plan to promote the issue of safe patient handling and the prevention of musculoskeletal disorders among nurses in the United States. Through a variety of activities, the campaign seeks to advocate, educate, and facilitate change from traditional practices of manual patient handling to emerging technology-oriented methods. Staff education needs to include content and experiences to facilitate the safe use of the most effective handling methods. In addition, education should put more emphasis on assistive patient handling equipment and devices ensuring that students know how to safely use this equipment. The National Institute for Occupational Safety and Health (NIOSH, 2023a) also supports guidelines for safe patient handling and mobility.
- Violence: Violence may not be a typical staff safety concern that a student would first think of when asked about safety in the healthcare workplace, but it may be a problem. There is a greater risk of violence in emergency departments, psychiatric/mental health/substance use disorder treatment services, and long-term care facilities; however, such incidents may occur anywhere. Patients and families may not be able to control their emotions appropriately and then respond with anger and violence. The nurse may also be in a situation in which there is violence that is not directly related to the nurse or health care, such as providing home health care in a neighborhood that has a high level of crime and violence. Staff members need training so that they can be alert and prevent violence when possible-particularly training in identifying signs of escalation and use of methods to deescalate a situation when possible. They need to know how to protect themselves when violence cannot be prevented. In areas such as psychiatry/mental health, this training is more common. Signs of escalation include a sudden change in behavior, clenched jaws or fists, threats, pacing, increased movement, shouting, use of profanity, increased respirations, and staring or pointing. These signs do not mean that the person will become violent but rather that the nurse should be more aware of the person's behavior and communication to determine if the person is escalating. Protecting oneself is very important; for example, the nurse may decide it is safer to leave the room, stay near the door, or keep the door open but not appear to be blocking the door; ask other staff to be present; or call for security assistance. It is also important when any weapon is found in patient belongings to secure the weapon and call for professional assistance, such as the HCO's security and the police. HCOs should have a policy and procedure describing the expected staff response in this type of situation. This information should also include requirements for police entering HCOs and carrying weapons (for example, when entering a mental health unit, they must remove their guns).
- Chemical exposure: OSHA offers information on preventing workplace injuries caused by exposure to chemicals, which is something nurses may encounter during their work. Nurses are exposed frequently to sterilizing chemicals, housekeeping cleaners, drug preparation residue, radiation, and other hazardous substances reported to increase rates of asthma, miscarriage, certain cancers, and birth defects (in particular, musculoskeletal defects). There are limited workplace safety standards for the hundreds of hazardous substances to which nurses are exposed on the job (ANA, 2023c; HHS, CDC, NIOSH, 2023b). Other reviews of healthcare workplace safety note concerns about anesthetic gases; hand and skin disinfection; latex (for example, gloves); medications, such as antiretroviral medications and chemotherapeutic agents; mercury-containing devices; personal care products; and sterilization and disinfectant agents, such as ethylene oxide and glutaraldehyde. The ANA continues to monitor risks for nurses and provide information on its website. Nurses need to be aware of past and current data that indicate specific potential problems to protect themselves and their colleagues from exposure and prevent injuries and health problems. In addition, nurses need to be alert to symptoms of allergies to drugs and products that can directly affect their health and practice.
The AHRQ defines a learning health system as “a health system in which internal data and experience are systematically integrated with external evidence, and that knowledge is put into practice. As a result, patients receive higher quality, safer, more efficient care, and HCOs become better places to work. Learning Health Systems include the following, and Figure 12-6 identifies the key elements (HHS, AHRQ, 2019):
Figure 12-6 Learning Health System.
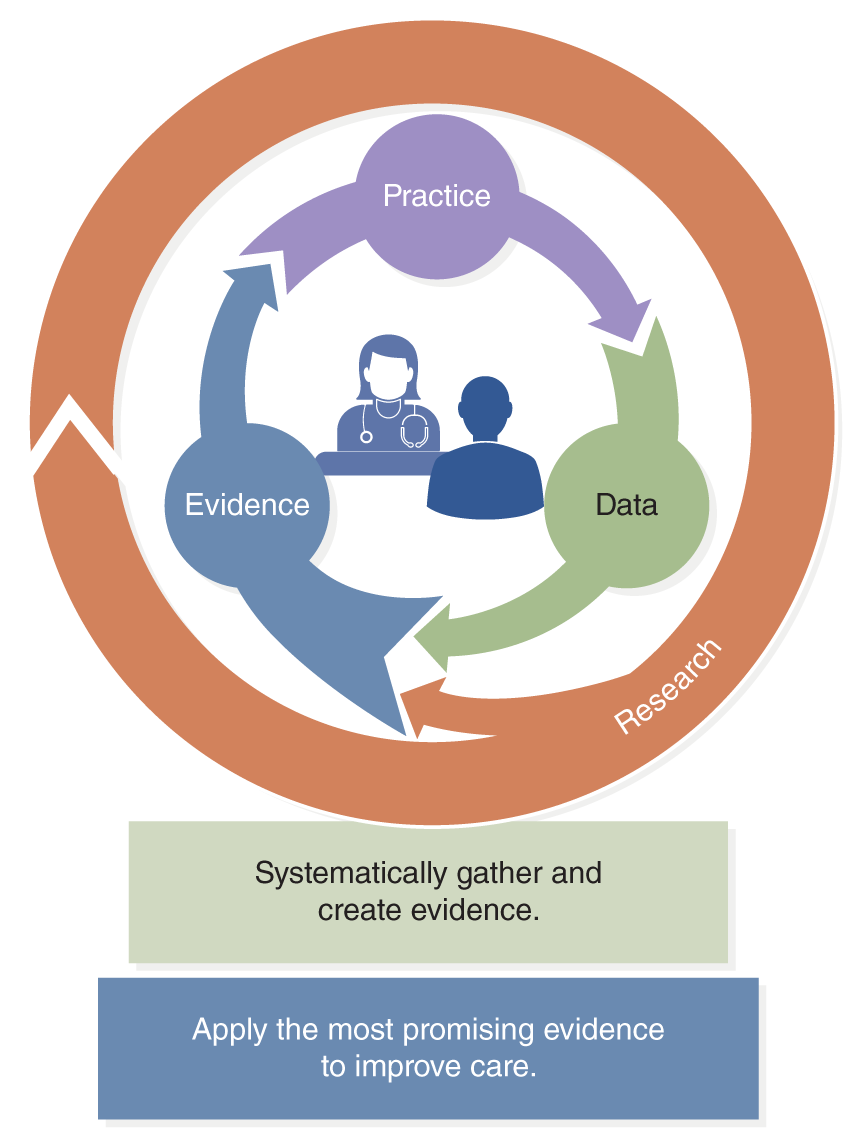
A circular diagram consists of interconnected sections labeled Practice, Data, and Evidence, forming a continuous cycle with arrows.
Inside the circle, there is an illustration of a healthcare provider and a patient. The outer ring is labeled Research. Below the diagram, there are two statements: Systematically gather and create evidence and Apply the most promising evidence to enhance care.
U.S. Department of Health and Human Services (HHS), Agency for Healthcare Research and Quality (AHRQ). (2019). Learning health systems. https://www.ahrq.gov/learning-health-systems/about.html
- Have leaders who are committed to a culture of continuous learning and improvement.
- Systematically gather and apply evidence in real time to guide care.
- Employ informatic technology methods to share new evidence with clinicians to improve decision-making.
- Promote the inclusion of patients as vital members of the learning team.
- Capture and analyze data and care experiences to improve care.
- Continually assess outcomes to refine processes and training to create a feedback cycle for learning and improvement.
| Stop and Consider 3 |
|---|
| Safety is a component of quality health care. |
Quality Improvement
Healthcare quality improvement focuses on the healthcare system, which is fragmented and in need of improvement. Plsek (2001) defined a system as “the coming together of parts, interconnections, and purpose. While systems can be broken down into parts, which are interesting in and of themselves, the real power lies in the way the parts come together and are interconnected to fulfill some purpose. The healthcare system in the United States consists of various parts (e.g., clinics, hospitals, pharmacies, laboratories) that are interconnected (via flows of patients and information) to fulfill a purpose (e.g., maintaining and improving health)” (p. 309). This does not mean that meeting individual patient needs and individual patient care improvement are not important. Each patient's care is part of the overall emphasis on healthcare improvement and is integrated into the system. Ultimately, the goal is that each patient's outcomes will be met, and this has an overall impact on population and community health.
The Institute for Health Improvement suggests that new designs can and must be developed to simultaneously accomplish three critical objectives-that is, the Triple Aim, which is now integrated into most QI efforts, both by HCOs and in health policy, to improve care on a continuous basis. The aims are (IHI, 2023a):
- Improve the health of the population.
- Enhance the patient experience of care (including quality, access, and reliability).
- Reduce, or at least control, the per capita cost of care.
More recently a fourth aim has been added: To improve the work life of healthcare providers. This addition recognizes the importance of staff safety (Feeley, 2017).
You will observe and be involved in issues of quality care as a student and then as a nurse in practice. Entering the healthcare system and the nursing profession, you may have doubts that QI is an important topic, particularly if you have found the health system to be effective for you and your family. In this case, this might demonstrate that the healthcare system or HCO in which you received care had an effective QI program that you might not know about. There are, however, serious problems that have been reported routinely in major reports, by the government, organizations, healthcare providers, and consumers. The content in this chapter is critical for you as a nurse as you engage in efforts to improve care daily for your individual patients, families, communities, and the healthcare system.
QI needs to be viewed as a continuous process as there is no end point, so it is often referred to as continuous quality improvement. When QI is discussed, there are several perspectives to consider. The first and most critical is your individual practice. What you do as a nurse has a direct impact on patient outcomes and quality. This chapter and other content in this text guide you in understanding your responsibilities and the importance of your engagement in CQI. There are two other perspectives that affect individual healthcare professionals and healthcare quality in general. One of the perspectives is the structure and processes of HCO QI programs that are designed to support the HCO efforts to maintain and improve care quality. The second view is the health policy perspective-QI initiatives from the local, state, and national levels and related requirements that influence how HCOs maintain and monitor CQI. These perspectives should be in sync to ensure effective health care for patients, families, and communities.
Implementing QI “requires that health professionals be clear about what they are trying to accomplish, what changes they can make that will result in an improvement, and how they will know that the improvement occurred” (IOM, 2003, p. 59). Healthcare complexity is mentioned many times as a barrier to understanding quality and improving healthcare delivery. Its consumers are very diverse in their needs, diagnoses, ethnic and cultural backgrounds, and overall health status, including genetic background, socioeconomic factors, patient preferences for health care, community differences, and healthcare coverage/reimbursement. Health care cannot be viewed in the same manner as other businesses (such as the automobile industry) that might manufacture or sell one product or a series of highly related products. Healthcare products/services vary based on the medical problem and the patient, the setting, the expertise of clinical staff, diagnosis, treatment options, patient decisions, patient prognosis, health policy and legislation, advances in science, medical technology, and health informatics technology (HIT). Even in specialty areas, such as obstetrics, psychiatry/mental health, emergency care, intensive care, home health care, and long-term care, there is great variation within the services-in their interventions, patient and family roles, patient education needs, prognosis and outcomes, and so on. It is expensive to develop and maintain effective QI programs, but The Joint Commission requires such programs for all its accredited organizations to guide HCOs and their staff in improving care daily and reimbursement sources, such as for Medicare and Medicaid and other insurers, also expect ongoing QI activities (Finkelman, 2022).
Because of the complex nature of quality, developing an HCO QI program that addresses monitoring and improving healthcare quality is in and of itself a complex process. HCOs typically have a department with staff that focus on CQI. This requires staff and a budget for these efforts, and the program must plan, implement its plans, monitor and measure quality, and then identify and implement interventions and solutions to maintain quality or improve quality. Effective appraisal of the scientific facts suggests that health care can be improved by closing the wide gaps between prevailing practices and the best-known approaches to care and by developing new forms of care-applying evidence-based practice (EBP). This requires planning and careful evaluation of results. One model for improvement focuses on three key questions that continue to be important today, which are (Berwick & Nolan, 1998, p. 209):
- What is the HCO trying to accomplish?
- How will the HCO know whether a change is an improvement?
- What change can the HCO try that it believes will result in improvement?
Even in the earliest reports on quality care, it was noted that for an HCO to have an effective QI program, nurses and other health professionals need to be knowledgeable and competent in a number of areas, and this view has continued as QI developed (IOM, 2003). All aspects of the healthcare environment are important to consider, such as patients, staff, and their interactions; patient and healthcare outcomes; and changes in science, technology, and the needs of individuals and communities. HCOs need to consider and compare factors with other HCOs and similar healthcare systems to determine the best current practices and then develop and apply interventions to improve care. This all requires an understanding of quality issues-errors, risks, human factors-that affect quality care for patients and staff safety, monitoring, and measurement. Surrounding all of this is the need to integrate interprofessional teamwork in CQI and in care practice.
| Stop and Consider 4 |
|---|
| QI is a continuous process (CQI). |
Examples of Quality Initiatives
The Quality Chasm series of reports stimulated the development of several important safety initiatives. The IHI, for example, was established in 1991 and describes itself: “For more than 25 years, the Institute for Healthcare Improvement (IHI) has used improvement science to advance and sustain better outcomes in health and health care across the world” (IHI, 2023b). The IHI also focuses on STEEEP®. The 5 Million Lives Campaign is one example of an IHI safety initiative. This voluntary global initiative sought to protect patients from 5 million incidents of medical harm over 2 years (December 2006-December 2008) (IHI, 2023c). This initiative led the IHI to further develop its resources to improve healthcare quality, such as an improvement map designed to help hospitals respond to multiple requirements they face and to focus on high-leverage changes to transform health care. A newer IHI initiative was the 100 Million Healthier Lives Campaign with a projected worldwide goal by 2020 (IHI, 2023d). The COVID-19 pandemic has had an impact on this initiative, which was not expected when the campaign was developed, so time will be needed to determine its impact on global health status.
Another initiative, a collaborative effort between the IHI and the Robert Wood Johnson Foundation (RWJF), focuses mostly on nursing-Transforming Care at the Bedside (TCAB). TCAB is a “unique innovation initiative that aims to create, test, and implement changes that will dramatically improve care on medical/surgical units, and improve staff satisfaction as well” (IHI, 2023e). This program supports and guides pilot QI projects to improve care developed at the point of care by staff in practice, offering many opportunities for improvement and engaging nurses in the QI process. The framework includes (RWJF, 2020):
- Safe and reliable care
- Vitality and teamwork
- Patient/person-centered care
- Value-added care processes
The Joint Commission's (2023b) annual safety goals, which were first introduced in 2003, is a safety initiative developed by the major healthcare accreditation organization and, thus, has an impact on many HCOs. Each year, The Joint Commission identifies safety goals that should be the focus of every HCO accredited by The Joint Commission. These goals identify critical current safety concerns based on data The Joint Commission collects and analyzes from its accredited HCOs, as well as other sources of information about healthcare safety. An example of awareness of changes in health care is the addition of healthcare disparities, quality and safety, and equity in its standards (The Joint Commission, 2023c). The organization's accreditation surveyors emphasize the annual safety goals during accreditation visits. HCOs typically provide staff education related to the goals and monitor goal progress. Nursing students need to know the current safety goals and integrate them into their clinical learning experiences. The current annual goals are available on The Joint Commission website (2023d).
The Joint Commission Accreditation
Accreditation is the process used to evaluate organizations, particularly focused on quality and based on minimum standards. The major organization that accredits HCOs is The Joint Commission, a nonprofit organization accrediting more than 22,000 HCOs in the United States, including hospitals, home healthcare agencies, clinical laboratories, ambulatory care organizations, behavioral health, and nursing care centers (postacute, subacute, long-term care). It also accredits HCOs in other countries (The Joint Commission, 2023b). This accreditation organization has been in operation since 1951, and over that time, the accreditation requirements and process have changed to adjust to changes in healthcare. Participating in a Joint Commission accreditation survey is time-consuming and costly, but it is necessary for HCOs. For example, nursing education programs need to use HCOs with current Joint Commission accreditation for student practicum/clinical experiences. As The Joint Commission has changed, its emphasis on quality care has also changed. CQI is now the major focus of the accreditation process, which includes safety.
Nurses serve on The Joint Commission Nursing Advisory Council, which advises The Joint Commission about nursing concerns and care issues related to quality and accreditation. Nurses who work in HCOs eventually experience the Joint Commission survey. After initial accreditation is received, The Joint Commission surveyors visit the accredited HCO every 3 years to complete its intensive survey for accreditation renewal, and it may even make unscheduled visits. For the scheduled visits, the HCO is given a date and has 9-12 months to prepare for the visit. Preparing for the visit involves gathering information and data for The Joint Commission, preparing written reports, educating staff about the standards, conducting mock surveys to prepare staff, and so on. The HCO should always meet the expected accreditation standards, not just at the time of a survey. In the past, great emphasis was placed on getting ready for The Joint Commission visit and surviving it; afterward, the HCO was less vigilant until it was time to prepare for the next visit. This approach of just focusing on the survey every 3 years eventually changed, and now accredited HCOs must submit reports on certain data to The Joint Commission annually, with a plan of action for areas noted in the self-assessment that may require improvement (periodic performance appraisal/review); in addition, HCOs must be prepared for possible unscheduled visits or requests for additional data.
Nurses are very active in preparing for the survey and during the survey visit. It is challenging to manage this review and continue with routine work. It is helpful for HCOs to do their own internal surveys to gather information to develop structured action plans to improve (Pierson, 2023). The Joint Commission survey now involves more direct care staff in the survey visits by including them in meetings to discuss care in the HCO and asking individual staff questions during the visit. If students are present during the visit, surveyors may ask them questions. The goal is to find out if patients are achieving expected outcomes and, if not, why. Examples of outcomes that The Joint Commission assesses include staffing, communication, care planning, mortality rates, length of stay, sentinel events, adverse incidents, complications, readmission rates, patient/family satisfaction, referrals to specialists, patient adherence to discharge plans or treatment plans, achievement of safety goals, prevention adherence services (for example, mammograms, Pap smears, immunizations), and more. The Joint Commission (2023d) standards are periodically evaluated and revised to meet changes in healthcare delivery. These standards form the framework for accreditation. The Accreditation Guide provides a detailed review of what is included in the surveys, demonstrating this complex process (The Joint Commission, 2023e).
Because The Joint Commission accredits a broad range of HCOs, there are differences in the minimum standards and in how the various healthcare settings might monitor care and outcomes. An example is home healthcare agencies. These agencies may use other national evaluation approaches that are not led by The Joint Commission. The home healthcare outcome-based approach to QI, known as the Outcome and Assessment Information Set (OASIS), was developed in the 1990s by the HHS and the Centers for Medicare and Medicaid Services (CMS). It offers a database for collecting and organizing home healthcare data so that outcomes can be analyzed (HHS, CMS, 2023a). This database focuses on a group of data elements that represent core items for a comprehensive assessment of home healthcare patients. The key question is: Did the patient benefit from the home healthcare services? In this type of system, home healthcare agencies from all over the country input their QI data. The CMS manages the OASIS and, by doing this, offers a national view of home healthcare quality. The CMS is responsible for federal oversight of care quality in all U.S. hospitals that receive Medicare and Medicaid reimbursement, and since most hospitals and many other types of HCOs have patients who receive this reimbursement, this has a major impact on the healthcare delivery system (Pierson, 2023; HHS, CMS, 2023a). These hospitals include approximately 61.4 million patients who receive Medicare, Parts A and B, and 75.8 million have Medicaid reimbursement. For the HCOs to receive CMS payments, they must meet the conditions of participation mandated by CMS. These requirements include accreditation from one of 10 accrediting organizations, such as The Joint Commission, and CMS also assesses The Joint Commission's survey process to ensure it meets the CMS conditions of participation. This is an example of linking reimbursement, accreditation, performance, and quality care.
Healthcare Report Cards
Healthcare report cards provide specific HCO performance data at required intervals, with a focus on quality. The report can be used by the HCO to compare its outcomes with report cards published by other similar HCOs or with a large state or national database (benchmarking). This information can be helpful in improving care in an HCO by identifying what the HCO is doing well and what needs improvement as compared with other similar HCOs. Some of these report cards are accessible on the internet and may also be reviewed by consumers (patients, families). Nurses may use them when searching for jobs to obtain evaluation data about a specific HCO as a potential employer. In some cases, insurers use healthcare report cards to assess an HCO and compare it with similar HCOs. The goal is to examine performance based on clearly defined criteria.
Examples of other changes in QI focus on sharing information with patients and rewards for QI performance. Today, public reporting is more common, and there is greater access due to the internet, so report cards may be made public. This sharing of predetermined quality and efficiency measures of performance data informs patients and stakeholders about provider performance; for example, a patient might use this information to select a hospital or other type of provider for the patient's needs.
Value-based performance is also used today. This is a payment system that provides financial rewards for performance. This type of system, in addition to public reporting, may incentivize providers to improve outcomes. There is, however, a risk that pay-for-performance (P4P) may act as an incentive to “cut corners,” to take steps to ensure data “looks positive” when this is not the case. An example is found in Exhibit 12-1 describing how some of the facilities in the Veteran Health Administration (VHA) changed records about appointment data and wait times in order to improve their performance data.
In 1994, the ANA began an examination of the impact of workforce restructuring and redesign on the safety and quality of patient care in acute care settings. In 1998, this examination led to the development of a nursing report card, the National Database of Nursing Quality Indicators (NDNQI®) (Montalvo, 2007). This occurred around the time that the Quality Chasm series began to address healthcare quality. The ANA wanted to “explore the nature and strength of the linkages between nursing care and patient outcomes by identifying nursing quality indicators” (Pollard et al., 1996, p. 1). This initiative also provides a framework for educating nurses, consumers, and policymakers about nursing contributions within the acute care setting and the need to track the quality of nursing care provided in such settings. The NDNQI made it clear that data on nursing and outcomes were lacking-that is, the methods HCOs used to collect data at that time did not include nursing-specific data. Patients come into the acute care setting primarily because they need around-the-clock care, which is the focus of nursing care, and yet data on this care were not accessible.
Initially, the University of Kansas School of Nursing, under contract to the ANA, managed the NDNQI, but now this is done by Press Ganey, a company that offers services to evaluate HCO quality and patient satisfaction (Press Ganey, 2020; 2023). There are now more than 2,000 U.S. hospitals participating in this database. Except for Magnet hospitals, which are required to use NDNQI, participation in the NDNQI process is voluntary; therefore, only participating HCOs are reflected in the data. The initiative focuses on providing comprehensive nursing-sensitive quality measures to assist in tracking nursing care using more than 250 individual measures related to structure, process, and outcomes; help prevent adverse events and promote quality patient care; empower nurses to take actions based on unit-level comparisons with other similar units; and give nurses the opportunity to speak up and improve quality (Press Ganey, 2023). The participating HCOs submit their nursing-sensitive indicator data to the NDNQI electronic database, which collects a large amount of data for evaluation and research. To assist with more effective comparisons, reports are provided to participating hospitals with information about patient population, unit type, and hospital bed size. The result is a more detailed nursing profession quality report card, providing information about the characteristics of the nursing workforce/structure, nursing processes, and patient outcomes within an HCO.
Other public reporting now includes some nursing-sensitive indicators. The National Quality Forum (NQF) is an important national quality initiative, and it collaborates with the NDNQI. The NQF Strategic Plan goals are (2022):
- Define the national measurement architecture to drive improvement in quality and value.
- Advance health equity and address disparities.
- Become a national leader in defining measures for equitable patient and family engagement.
- Develop measurement approaches utilized in value-based payment arrangements.
- Promote the transformation to digital health.
- Close quality gaps for national healthcare priorities.
The NQF examines some of the critical care issues that need to be considered to meet these goals. Currently, the NQF endorses about 300 measures, which are used in more than 20 federal public reporting, pay-for-performance programs, state programs, and the private sector, but it does not develop measures (NQF, 2023). The NQF also identifies areas that require more measures to reduce gaps and to better ensure measures are effective.
In 2020, the NDNQI was used to assist with improving care during the COVID-19 pandemic. For example, it developed the following resource for HCOs: “COVID-19 CLABSI (central line-associated bloodstream infection) Tip Sheet and a Prone Positioning Kit for HAPI Prevention are strategies developed to address quality of care issues experienced with the COVID-19 patients” (Stifter, 2020, p. 1). These efforts reduced problems and now provide an additional standard of care, which require practice changes. This is an example of how a public health crisis can lead to more examination of current problems and develop positive changes and innovations to assist staff, improve care, and ensure better patient and community health outcomes.
The federal government is also involved in the use of report cards. For example, the NHQDR, discussed earlier in the chapter, serves as another report card option. It is now the major national annual report on the status of care in the United States-quality and diversity. Current reports can be accessed online (HHS, AHRQ, 2023a). The HHS uses report cards in its own activities, for example, its 2024 Annual Performance Plan demonstrates the importance of CQI with the national government's healthcare services whose goal is to ensure the health and safety of the American public and uses the National Strategic Plan. This extensive federal plan includes the following goals and related objectives that relate to CQI (HHS, AHRQ, 2023a):
Strategic Goal 4: Restore Trust and Accelerate Advancements in Science and Research for All.
Objective 4.1: Improve the design, delivery, and outcomes of HHS programs by prioritizing science, evidence, and inclusion.
Objective 4.2: Invest in the research enterprise and the scientific workforce to maintain leadership in the development of innovations that broaden our understanding of disease, healthcare, public health, and human services resulting in more effective interventions, treatments, and programs.
Objective 4.3: Strengthen surveillance, epidemiology, and laboratory capacity to understand and equitably address diseases and conditions.
Objective 4.4: Improve data collection, use, and evaluation, to increase evidence-based knowledge that leads to better health outcomes, reduced health disparities, and improved social well-being, equity, and economic resilience.
Strategic Goal 5: Advance Strategic Management to Build Trust, Transparency, and Accountability.
Objective 5.1: Promote effective enterprise governance to ensure programmatic goals are met equitably and transparently across all management practices.
Objective 5.2: Sustain strong financial stewardship of HHS resources to foster prudent use of resources, accountability, and public trust.
Objective 5.3: Uphold effective and innovative human capital resource management resulting in an engaged, diverse workforce with the skills and competencies to accomplish the HHS mission.
Objective 5.4: Ensure the security and climate resiliency of HHS facilities, technology, data, and information, while advancing environment-friendly practices.
The plan's focus elements are equity, SDOH, critical health problems, such as mental health and substance use disorders, the use of evidence-based practice and the need for research, and leadership and management supporting planning and CQI.
| Stop and Consider 5 |
|---|
| Healthcare accreditation supports QI, but it does not ensure quality improvement. |
Patient Safety Culture™ (SOPS®)
The Agency for Healthcare Research and Quality's (AHRQ) initiative, Surveys on Patient Safety Culture™ (SOPS®) provides important information for hospitals, medical offices, nursing homes, community pharmacies, and ambulatory care centers and the survey data (HHS, AHRQ, 2023c):
- Raises staff awareness about patient safety.
- Assesses the current status of patient safety culture.
- Identifies strengths and areas for patient safety culture improvement.
- Examines trends in patient safety culture change over time.
- Evaluates the cultural impact of patient safety initiatives and interventions.
The AHRQ recommends that communities, HCOs, and healthcare providers do the following to apply SOPS® data in planning services (HHS, AHRQ, 2023c):
- Identifying Areas to Improve:
- What areas do you want to focus on for improvement?
- What are your "SMART" goals? (Specific, Measurable, Achievable, Relevant, Time bound)
- Planning Your Improvement Initiatives:
- What initiative will you implement?
- What resources will you need?
- What are possible barriers, and how can you overcome them?
- How will you measure progress and success?
- Will you pilot-test the initiatives?
- What is the timeline?
- Communicating Your Action Plan:
- How will you share your action plan?
- How will you provide progress updates on your action plan?
National Quality Strategy
A provision in the Affordable Care Act (ACA) of 2010 required the HHS to develop the National Quality Strategy (NQS). The AHRQ, an agency in the HHS, led the development of the strategy by using an evidence-based approach along with a collaborative effort, including feedback from more than 300 stakeholders representing the federal government, especially the HHS; the states; the private sector; and multi-stakeholder groups, such as healthcare professional organizations. The AHRQ now also manages the ongoing NQS. It is a groundbreaking initiative supporting national measurement and QI at multiple levels: community, practice settings, and individual physicians (HHS, AHRQ, 2017a). As the strategy was developed, a critical problem was noted. There were too many QI measures and no control or evaluation of the measures, causing measurement redundancies and overlaps that might negatively affect the value of data and results. As this work continued, the NQS now addresses the assessment of measures and the measurement process on an ongoing basis.
Patient/person-centered care is a core factor in the NQS, supporting earlier work emphasizing PCC. The major purpose of the NQS is to provide a national approach to measure quality and ensure higher quality care for all, which correlates with the Triple Aim and STEEEP®. The NQS recommends that all HCOs adopt the Triple Aim and STEEEP®, and many HCOs are meeting this recommendation. The NQS priorities establish a guide to maintain and improve health and healthcare delivery and are also monitored as part of the annual NHQDR and correlate with other initiatives, such as Healthy People 2030. The NQS establishes priorities, and information about outcomes related to the priorities is then included in the annual NQS report to Congress (HHS, AHRQ, 2017a). Thus, data for the NQS annual report originate from multiple HCOs and government agencies. The NQS provides a framework for effective development and coordination to establish core sets of measures to improve the measurement of multiple populations and healthcare services. It is clear we need to have better control and coordination of measurement-confusion does not support effective CQI. The six strategy priorities are (HHS, AHRQ, 2017b):
- Make care safer by reducing harm caused in the delivery of care.
- Ensure that each person and family is engaged as partners in their care.
- Promote effective communication and coordination of care.
- Promote the most effective prevention and treatment practices for leading causes of mortality.
- Work with communities to promote the wide use of best practices to enable healthy living.
- Make quality care more affordable for individuals, families, employers, and the government by developing and spreading new healthcare delivery models.
The priorities may change over time as the NQS is evaluated and adapted to current needs. Figure 12-7 provides an overview describing how the NQS works. It is important to consider the entire healthcare delivery system rather than just focus on the hospital setting, so the plan applies to all types of healthcare settings and addresses the entire continuum of care.
Figure 12-7 NQS: How it works.
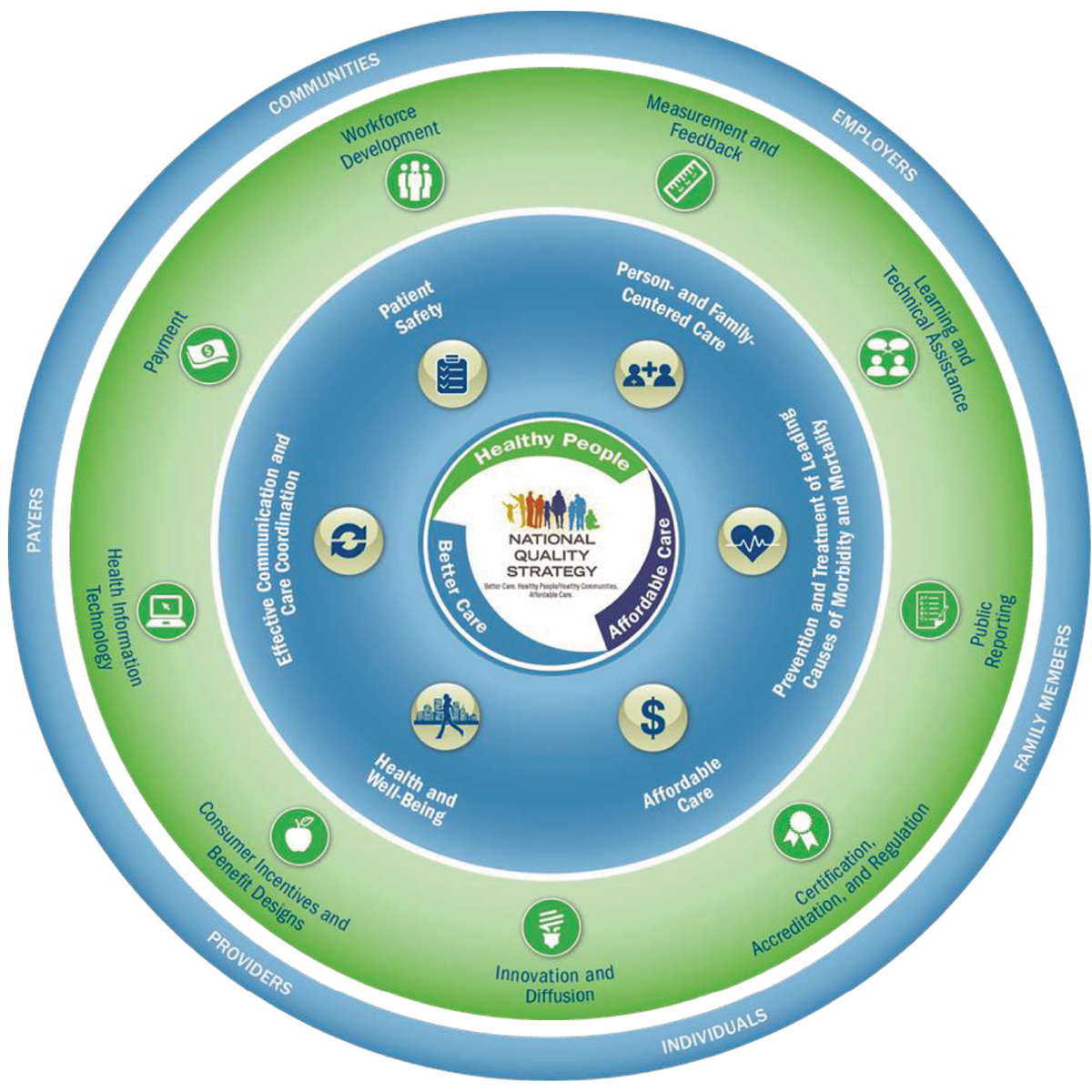
A concentric circle diagram details the National Quality Strategy.
At the center, it reads National Quality Strategy, surrounded by healthy people, better care, and affordable care. Surrounding this core are key areas: Patient safety, Person- and Family-Centered Care, Prevention and Treatment of Leading Causes of Morbidity and Mortality, Affordable Care, Health and Well-Being, and Effective Communication and Care Coordination. The outermost ring includes factors such as Workforce Development, Measurement and Feedback, Learning and Technical Assistance, Public Reporting, Certification, Accreditation, and Regulation, Innovation and Diffusion, Consumer Incentives and Benefit Designs, and Health Information Technology. The diagram segments are labeled communities, employers, family members, individuals, providers, and payers.
Reproduced from Agency for Healthcare Quality and Research (AHRQ). (2015, July). National Quality Strategy: Overview (power point slide presentation). http://www.ahrq.gov/workingforquality/toolkit.htm
It is recommended that other healthcare programs, private and public, adopt the NQS; however, it is not required-though more healthcare programs and quality initiatives do correlate with the NQS, as noted in Figure 12-8. The AHRQ provides tools and resources to support the implementation of the NQS (HHS, AHRQ, 2017c). The NQS annual reports to Congress are posted on the AHRQ website. The 2020 congressional report states, “Across the nation the National Strategy for Quality Improvement in Health Care (NQS) brings together federal agencies, healthcare payers, purchasers, providers, consumers, and other partners in pursuit of improved health and health care for all Americans. The NQS serves as a framework for aligning stakeholders across private and public sectors at the federal, state, and local levels” (HHS, AHRQ, 2021). This effort continues currently with the ongoing implementation of the NQS, and there has been progress made to develop, implement, and monitor an ongoing national quality process as many of the initiatives described here were stimulated by the key initial IOM report in 1999 To Err Is Human, which was a major stimulus for what has been accomplished today.
Figure 12-8 Do you already align to the NQS?
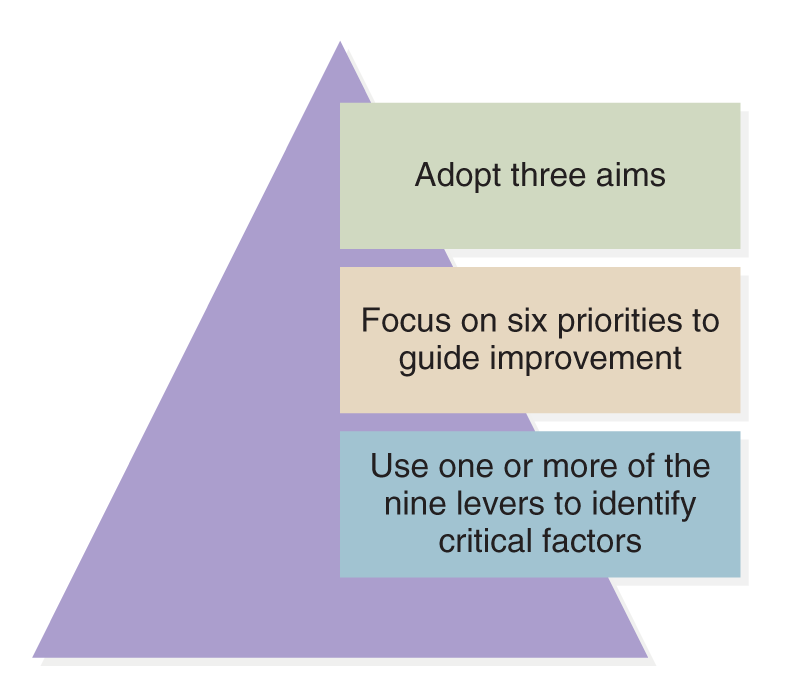
A pyramid diagram outlines alignment to the N Q S.
The pyramid is divided into three sections. The top section reads adopt three aims. The middle section reads focus on six priorities to guide improvement. The bottom section reads use one or more of the nine levers to identify critical factors.
| Stop and Consider 6 |
|---|
| The NQS should be integrated into our view of nursing practice to ensure QI. |
Federal Initiatives to Improve Care: Hospital-Acquired Conditions and 30-Day Unplanned Readmissions
In 2007-2008, to improve care and reduce costs, the CMS introduced a major change in its reimbursement policy. The CMS would no longer reimburse care required for complications/conditions that occurred in the hospital that could be prevented, now referred to as hospital-acquired conditions (HACs). Examples of HACs include falls, hospital-acquired decubiti, performing the wrong procedure, and administering the wrong blood type (HHS, CMS, 2023b). This policy has major implications: Who will pay for the care required for HACs, as they will occur? Ultimately, the HCO may have to cover the costs. HCOs are limited in what they can personally charge a Medicare patient. This issue is complex and serious, but the major message from the CMS is that when errors are made, there are costs involved, and performance is associated with cost. For many reasons, HCOs have problems maintaining a stable budget, and this change in reimbursement practice has a major impact on the financial status of hospitals. For example, suppose a patient who is covered by Medicare falls in the hospital and incurs an injury. Treatment for that injury may not be charged to Medicare and may not be charged to the patient personally. The hospital must provide care but will receive no payment for doing so. It is uncertain how hospitals will respond long term to this change; although they are developing methods to prevent HACs, some methods are more effective than others. However, this initiative is focused on encouraging HCOs to improve care and decrease HACs, which is a positive step for patients, families, HCOs, and payers.
In addition, in 2011-2012, Medicaid issued its initial list of HACs that might occur in hospitals, implementing the same policy as Medicare of not paying for HACs if they occurred in hospitalized patients covered by Medicaid. More current examples of some of these events, similar to Medicare's list, are blood incompatibility, falls and trauma, hypoglycemic coma, and surgery on the wrong patient or wrong body part. The Medicare and Medicaid list of HACs may change over time based on data related to common complications and errors. The CMS website maintains an updated list of HACs. In early 2008, some of the major insurers came out in support of the approach initiated by the CMS, announcing their own zero tolerance for HACs and identifying their lists of such events. Hospitals are now required to monitor and respond to all HACs regardless of insurer, and as noted here, insurers do not always include the same HACs on their lists.
Nurses can make a difference in preventing HACs. They need to be involved in determining interventions to prevent these conditions or “never” events, as they are sometimes called. Nurses need to understand HACs and why they are important. The targets for HACs are conditions that are (1) high volume and cost; (2) identified as a complication, comorbidity, or major complication as connected with CMS diagnosis-related groups; and (3) reasonably preventable using evidence-based guidelines (HHS, CMS, 2023a). HACs are quality care problems, but with this policy change, they are now associated with reimbursement, too.
In addition, attention has turned to evidence-based guidelines to improve care focused on the HACs and the need to better ensure that HCOs prevent these problems that have a negative impact on patient outcomes. For each HAC, EBP guidelines are available that should be used as care is planned and provided. This emphasizes the importance of EBP and its relationship to CQI. The CMS goal is to stimulate hospitals to improve care-to decrease preventable HACs.
A second goal is to decrease care costs. Asking HCOs to improve care did not seem to make a major difference in quality care, so the CMS turned to incentivizing by limiting payment if care performance was not at the expected level. Current data indicate there has been some improvement, but more is needed; for example, data indicate there are nine HACs per 100 discharges, and monitoring this helps to determine the extent of the problem with HACs (Lawton et al., 2020). Some HCOs have criticized the fairness of the penalties on some hospitals, which requires assessment and may lead to changes in how CMS applies the reimbursement policy. In summary, we need greater partnerships (HCOs, insurers, government) to improve care and structured initiatives to monitor and respond to problems. Motivating healthcare providers to improve performance by including a financial incentive may or may not be ideal, but it is currently used.
Along with the development of the initiative to reduce HACs, the CMS turned to examining CMS beneficiary unplanned readmissions for any cause to an acute care hospital within 30 days of discharge. ‘The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that, for example, encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. The program supports the national goal of improving health care for Americans by linking payment to the quality of hospital care” (HHS, CMS, 2023b). The goal of this initiative is the same as for HACS: to improve care, reduce costs, and require that hospitals do the following (HHS, CMS, 2023c). The following are interventions that hospitals might use to reduce readmissions.
- Analyze the root causes of readmissions: Understand patterns and trends for the HCO and the local community for comparison; understand the patient's perspective, for example, the effectiveness of communication and coordination. Data should be tracked routinely.
- Inventory and align the current readmission reduction efforts to meet the needs of the HCO's targeted patients: This should be an in-depth inventory; HHS provides several tools (Hospital Inventory, Cross-Continuum Team Inventory, and Conditions of Participation Checklist) so that the HCO can understand what it currently does to prevent and/or respond to the problem to better plan changes.
- Examine the extent to which the current readmission reduction efforts meet the needs of the HCO-targeted patients: Combine previous information about methods HCOs may use.
- Improve hospital-based processes to better target and serve targeted patients' needs: With the previously mentioned information, set aims and objectives and then identify strategies that will be part of the program. Examples of strategies that might be used are checklists, arranging for post-discharge follow-up, flagging discharges more than 30 days in the chart, developing transitional plans, engaging the patient and, when appropriate, the family with the patient's permission, and identifying high-risk patients.
- Expand and strengthen cross-setting partnerships: Implement strategies to increase collaboration with cross-setting partners.
- Provide enhanced services to patients at high risk of readmission: Implement strategies for high-risk patients.
Figure 12-9 provides data on the costs of readmissions. There has been improvement since 2016-2019 data were reviewed-the number of readmissions decreased by 10% in 2020.
Figure 12-9 Readmission Costs.
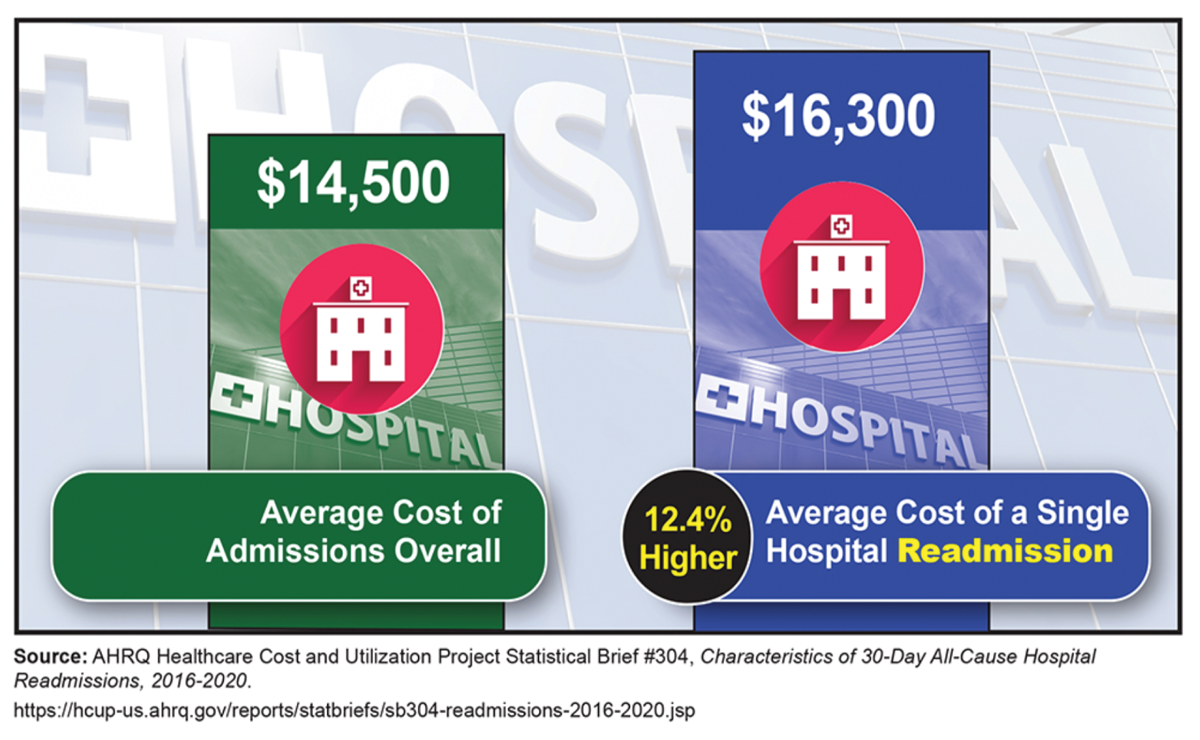
A comparative graphic illustrates readmission costs.
The left side displays Dollars 14,500 and an icon of a hospital with the text reads, Average Cost of Admissions Overall. The right side displays Dollars 16,300 and an icon of a hospital with the text reads, Average Cost of a Single Hospital Readmission. A label on the right side reads 12.4 percent Higher.
AHRQ Healthcare Cost and Utilization Project Statistical Brief #304, Characteristics of 30-Day All-Cause Hospital Readmissions, 2016-2020. https://hcup-us.ahrq.gov/reports/statbriefs/sb304-readmissions-2016-2020.jsp
Nurses are directly involved in this problem because discharge planning and patient education are critical elements in preparing patients for discharge and establishing an effective postdischarge trajectory so that patients do not need to be readmitted within 30 days of discharge. Many nurses use teach-back, asking patients to repeat information they have learned, and other such methods to better ensure that patients and families understand the information they need post-discharge (Peter et al., 2015). Patients and families should also be involved in discharge planning to ensure that the plan will work post-discharge for the patient and in the environment in which the patient will be living. Consideration needs to be given to support services that might be required, such as home healthcare, the ability to get medications and medical supplies, follow-up phone calls and other communication with healthcare providers, social services, and support for caregivers. We cannot control all aspects of the patient's life and condition, but we need to do as much as we can to ensure patient success post-discharge.
| Stop and Consider 7 |
|---|
| The CMS decided that care was not improving for its beneficiaries, so it began to incentivize performance improvement with the possible loss of payment for services. |
Examples of High-Risk Healthcare Activities
As has been stated, we cannot eliminate all errors and healthcare quality concerns; however, we can reduce them-and we need to do this much more. There are some healthcare activities, for example, nursing interventions, procedures, and treatment, that are at higher risk for errors and quality problems than others. The Joint Commission's annual safety goals identify high-risk concerns in health care. There are factors that increase risk, and these should guide us in developing plans to reduce risk for individual patients, populations, and communities. We know that poor communication is a critical factor to consider. Today, with the increasing use of and development of technology-both for communication and use in treatment methods-we have opportunities for positive outcomes, but this also increases the risk of errors (Finkelman, 2022). We also know that staff need to be competent, and this requires not only improvement in academic professional education but also lifelong learning.
Medication Administration
Medication administration via any route or for any medication is a high-risk treatment intervention (HHS, CDC, 2023). A medication error is a “preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in control of the healthcare professional, patient, or consumer” (HHS, FDA, 2022). The medication administration process includes ensuring medical order, dispensing, administering, documenting, and monitoring. Common sources of medication errors are identified in Table 12-1. Students and staff need to apply methods to reduce medication errors. Some of these methods include the following: know and respond when high-alert medications are administered (drugs that are of higher risk for patient harm); report and analyze near misses; ask for help when needed; avoid distractions and interruptions during the medication administration procedure; if in doubt, ask for help (for example, other nurses, pharmacist, physician); double-check and verify; listen to the patient and family when they question something; do not use workarounds; be alert to allergies; apply sterile technique when required; follow policies and procedures; document in a timely manner; do not document medications you have not administered; provide appropriate patient education about medications; and routinely apply the five rights of medication administration.
Table 12-1 Common Sources of Medication ErrorAmbiguous orders | Incorrect drug selected |
Drug device use | Incorrect patient |
Environmental stress | Insufficient drug information |
Miscommunication in drug order | Insufficient information about other drugs patient is on (therapeutic duplication) |
Error-prone abbreviation | Insufficient laboratory information |
Illegible handwriting | Known allergy |
Improper dose | Limited patient education |
Incomplete orders | Limited staff education |
Incomplete/Insufficient monitoring | Look-alike or sound-alike drugs |
Incomplete patient information/patient information unavailable | Poor communication |
| Youngberg, B. (2013). Patient Safety Handbook (2nd ed.). Jones & Bartlett Learning. |
Pharmacology and medication administration are important content in the nursing curriculum. This content and related learning activities focus on pharmacology, understanding of drugs, and their impact on the five rights of medication administration, which emphasize safe medication administration: right patient, right medication, right dose, right time, and right route. The goal of applying the five rights is to reduce errors; however, since they are also the common areas for errors, nurses need to be alert during these times. Other rights have been identified that are not included in the long-recognized five rights but are important, including right documentation, right to refuse medication, and right to evaluation and monitoring (Anderson & Townsend, 2010). An example of how these rights impact care and QI and relate to health information technology (HIT) is administering the medication at the right time or time ordered. This has been a potential problem for some time, particularly as most HCOs use electronic medical records and bar codes. A commonly accepted policy that was supported by the CMS was that medications should be administered within 30 minutes of the ordered time. The Institute for Safe Medication Practice (ISMP, 2011) expressed concern about what happens when nurses cannot meet this standard. A typical nursing response when this requirement cannot be met is to use workarounds or shortcuts because nurses do not want this delay to be considered an error. The ISMP conducted a survey of 17,500 nurses. Most of the nurses in the survey believed that trying to meet the 30-minute deadline led to problems and errors, increasing pressure on their workload and responses. With electronic methods (medical records and use of bar codes), more data are now available regarding the actual times medications are administered so that it is easier to identify late administration, and then based on the CMS requirement, this might be considered an error. This viewpoint does not consider that most nurses can make common sense clinical decisions and are aware of medications for which administration time is a critical element and when there is a need to consider individual patient status issues. Due to this feedback, the CMS has changed this requirement (NYSNA, 2013). This example demonstrates how analysis of a quality problem may lead to change and improvement, but it also demonstrates that many factors and stakeholders may be involved.
Care Transitions and Handoffs
Care transition is a time of change for the patient, family and caregivers, and staff. It occurs when a patient's care is transferred from one staff member to another, one unit to another, one HCO to another, and from an HCO to the patient's home-it also occurs between students and staff and vice versa. If the transition is ineffective, communication is typically the key cause of problems, but it is also the key strategy to improve handoffs. There are other factors that interfere with effective handoffs, such as a stressful work environment, staffing levels, interruptions, problems with sharing digital information (as discussed in the text's informatics content), HIT equipment problems, leadership and management concerns, lack of staff preparation and understanding of the transition process, multitasking, and ineffective teamwork (Finkelman, 2022). During the pandemic, handoffs were difficult in many situations due to a lack of beds, equipment, such as ventilators and oxygen, the need for careful procedures and equipment to reduce the risk of exposure, and staffing, making handoffs highly stressful for patients, families, and staff. For example, during COVID-19 having patients wait in ambulances before admission to a hospital was not an effective handoff. During handoffs, it is important for staff to ask questions and expect to receive the required information so that patient care can continue as needed and in a safe manner. The use of standardized communication methods, such as SBAR, can help reduce problems, as discussed in this text. There is also a need for supportive communication between staff and the patient, and if the family is present, with the family too.
Failure to Rescue
Failure to rescue (FTR) is a time of potential critical risk for patients; when staff may miss something about the patient's condition and then not intervene as needed. There are many reasons this may occur, such as inadequate staffing levels, staff competency, and ineffective use of critical thinking and clinical reasoning/clinical judgment; ineffective response to alarms or alerts or malfunction of alarm equipment; distractions and emergencies; lack of routine monitoring, such as rounds and surveillance; and ineffective communication from one staff to another (for example, during handoffs). A common method used to reduce FTR is the use of a rapid response team (RRT), which is a team of critical care experts. Early warning systems (EWS) are used to help staff identify patients who are developing signs that they need more help-these are structured methods that hospitals designate for use by their staff so that staff are communicating clearly, consistently, and in a timely manner. The RRT responds to a call to the bedside to further assess the patient and determine the best treatment, which may mean transferring the patient to intensive care (HHS, AHRQ, PSNet, 2019c). A systematic review of studies on the use of RRTs indicated that 20% of the patients in the sample seen by the RRTs had experienced an adverse event, and 80% of these events were preventable (Amaral et al., 2015). Most of the events were not reported through the expected reporting system. The recommendation from this review was that when RRT was requested this assistance should be a trigger to investigate the possibility that an adverse event occurred so that staff can learn from these situations (Jackson, 2017). Another factor that has been examined in research indicates that “Rapid response (RR) systems are associated with decreased hospital mortality. Systemic biases and inequities can negatively impact RR outcomes. Language barriers between patients and providers are associated with worse outcomes, but it is unknown if language barriers are associated with RR outcomes” (Raff et al., 2023, p. 29). This study's findings suggest that language barriers may cause both delays in activating rapid response and the care provided during and after the RR system is activated. As noted throughout this text, health equity and disparities are a growing concern in health care, and this is an example of their impact on care.
Alarm/Alert Fatigue
With the growing use of technology, there is recognition that technology provides many advantages and improves care, but it also may lead to more problems. Alarm or alert fatigue occurs when staff do not respond or are slow to respond to a device alarm, for example, from a cardiac monitor, bedside physiological monitor, infusion pump, or ventilator. Why does this happen when alarms are supposed to direct us to immediate assessment and response? In some cases, on a single unit, such as an intensive care unit, there can be several hundred alarms per patient in a day. If you multiply this number by the number of patients on a unit, it is easy to see how these alarms can, over time, stress staff; added to this is the problem that between 85% and 99% of the alarms are false, requiring no clinical intervention (Finkelman, 2022; Woo & Bacon, 2020). During the COVID-19 experience, many units have cared for many critical COVID-19 patients who required equipment with alarms-it has been very stressful for staff to respond and cope, in addition to the increase in patient deaths. When there are many alarms for multiple patients, the risk of a poor response increases. This problem increased so much that The Joint Commission issued several sentinel event alerts for medical device alarm safety in hospitals and included this topic in its national safety goals (The Joint Commission, 2023f, g). Current research indicates this continues to be a problem: “alarm fatigue contributes to missed alarms and medical errors that result in patient death, increased clinical workload and burnout, and interference with patient recovery” (Albanowski et al., 2023). Alarm management strategies to reduce the problem now include individualized alarm thresholds and changes in devices allowing the standard alarm to provide information more effectively. This is an area of concern that continues to need more monitoring and strategies to resolve. Staff need to be involved in assessing this problem and developing interventions to improve it.
Missed Nursing Care
Missed nursing care is an issue that nurses need to attend to more in their practice and in their QI responsibilities. It is a type of error of omission, representing “needed nursing care that is delayed, partially completed, or not completed at all” (HHS, AHRQ, PSNet, 2019d) Due to the increased concern about this type of error-which has a negative impact on care coordination, implementation of care, and patient outcomes, this may increase risk that the patient will not get required care or other errors might occur. To address this problem, the AHRQ developed a patient safety primer on missed nursing care (HHS, AHRQ, PSNet, 2019d). In a systematic review of 42 studies, 55 to 98% of the nurses in the samples reported that they had missed one or more items required for assessment; most of this occurred during the last shift (Jones et al., 2015). This review also noted that missed nursing care is associated with decreased patient satisfaction and higher rates of adverse events. A study published in 2019 indicated that commonly missed care included ambulation three times per day or as ordered, turning a patient twice per day or as ordered, and medications administered within the time frame ordered (Hassels et al., 2019). The major predictors of risk for missed nursing care are staffing levels, the work environment, and teamwork. Nurses should be alert to the problem and focus strategies on preventing missed nursing care by applying these predictors. When nurses feel time pressure and competing demands during a shift, there is an increased risk something should be done but will not be done or not done completely. We know that efforts to develop a positive work environment with effective teams and team members who help one another, plus a culture of safety that emphasizes QI, supports nurses to work more effectively and improve patient care. Nurses also need to work in environments in which work needs are met, not just appropriate staffing levels, but also access to clinical supplies, equipment, medications, HIT, and staff education and support. Having these resources reduces missed nursing care-care cannot get done if the nurse does not have the resources to provide the care. In addition, work stress and staff fatigue impact missed care, so these factors need to be assessed and resolved.
| Stop and Consider 8 |
|---|
| There are many care situations that are times of high risk for errors. |
Tools and Methods to Monitor and Improve Healthcare Delivery
Other chapters include content about some of the methods used by HCOs to monitor and improve healthcare delivery. Some of these methods are related to nursing professional issues, such as the application of standards of care; application of EBP and evidence-based HCO policies and procedures; implementation of clinical pathways and protocols; staff licensure and credentialing to better ensure competency for practice; effective use of interprofessional teams and teamwork; application of HCO risk management (RM) focused on possible legal concerns that also affect quality care; and application of healthcare regulation and legislation requirements. In this section, we discuss other, more specific CQI tools and methods used by HCOs. Nurses use these tools and methods. This discussion does not include all possible tools and methods. Appendix Aaugments this content.
Evidence-Based Practice
EBP has a direct impact on quality improvement, and additional information about EBP is found in other content. Consideration of the following is important to the effective application of EBP (Leming-Lee & Watters, 2019, p. 1):
- Healthcare providers need to discover new solutions and the possibilities for better healthcare delivery and be change agents.
- Improvement comes from knowledge application.
- The science of improvement is multidisciplinary, using clinical science, systems theory, statistics, psychology, and other fields.
- A translation gap exists between what is known about EBP and best practices by healthcare providers.
- EBP frameworks and models have the potential to increase the use of evidence to guide the care process.
Utilization Review/Management
Utilization review/management (UR/UM) is the process of evaluating the necessity, appropriateness, and efficiency of healthcare services for specific patients or patient populations. HCOs use utilization review data in several ways-for example, to determine access and usage of services, if a service is no longer needed, whether a new service is needed, and to understand the relationship of data to patient outcomes. Data are primarily obtained from medical records to determine the necessity, appropriateness, and timeliness of healthcare services. Utilization review data are connected to financial concerns for the HCO and its budget (for example, whether the HCO is serving enough patients to meet its budget, types of procedures and their reimbursement, and so on). Utilization review is administered by HCO administration, although nurses may participate as data collectors and in the analysis process. Nurses should participate in making decisions about changes that might be made in clinical services that are based on UR data.
Benchmarking
Many hospitals and other types of HCOs use benchmarking. This is the process of comparing HCO performance to an external standard. It can help staff members and management understand how their performance compares to other HCOs, and this may then motivate them to engage in improvement. Benchmarking supports effective competition and improved performance (HHS, AHRQ, 2016).
One popular benchmarking approach is Six Sigma. This rigorous and systematic methodology utilizes information (management by facts/data) and statistical analysis to measure and improve an HCO's operational performance, practices, and systems by identifying and preventing defects in processes. The goal is to anticipate and exceed stakeholder expectations and increase effectiveness (Six Sigma, 2022).
Assessment of Access to Healthcare Services
Access to healthcare services is important to monitor and improve as part of the QI process, and it is now considered an integral element related to diversity, equity, and inclusion (DEI). According to the HHS, access to health care is recognized as a social determinant of health (SDOH). Communities are concerned about whether their citizens have access to care. Healthy People 2030 considers access to be a critical issue across the United States for all types of healthcare needs (HHS, ODPHP, 2023). The NHQDR also monitors access to care. When a patient does not have access, the patient's health status is at risk, and further complications may occur.
Policies and Procedures
Policies and procedures are part of all HCO structures and processes. Their purpose is to guide decision-making and practice to ensure more effective care and staff work processes. A key question always is: Do staff members use policies and procedures effectively? A study was conducted to examine this question (Kelly et al., 2020). In a sample of 235 practicing nurses, most used policies and procedures at least monthly, and the most important barrier to frequent use was their length. This is an ongoing issue as policies and procedures are not new to health care, but their quality may be questioned. They need to be clear and accessible, which is now best done through electronic means, and this should increase accessibility to information when needed.
Medication Reconciliation
Patients often take many medications, and a key concern is how these medications interact with one another. Medication reconciliation refers “to the process of avoiding such inadvertent inconsistencies across transitions in care by reviewing the patient's complete medication regimen at the time of admission, transfer, and discharge and comparing it with the regimen being considered for the new setting of care” (HHS, AHRQ, PSNet, 2019e). Responsibility for completing the medication reconciliation procedure needs to be clarified in a policy and procedure. Use of routine tracking is important. HCOs should have a standardized form on which to record the information in the documentation system. If the patient takes a lot of medications and cannot remember all the information, medication reconciliation can take time to complete and may be inaccurate. The Joint Commission now requires that its accredited HCOs use medication reconciliation routinely. If problems arise in reconciling medications, then errors may result due to omitted medications, incorrect dosage, incorrect route, incorrect timing, use of the same medications but with different formulations, use of drugs that do not interact effectively or safely with one another, and failure to discontinue contraindicated medications (HHS, AHRQ, PSNet, 2019e).
Standardized Communication Methods
HCOs are now using more standardized communication methods; some have been discussed in other text content. This increased use is mostly due to the recognition that errors are often associated with ineffective communication. There are many methods now used or incorporated with other methods to address CQI problems. An example of the latter is that during handoffs, HCOs may require the sharing of specific information. Staff members are trained in using the structured script to provide critical information and thus make sure this information is not forgotten. In a study of standardized communication used during handoffs, recurrent types of content covered in various standardized methods were identified and now considered important, including introduction, patient/administrative data/necessary patient information, danger or risk(s), background/history, situation/story/framework, follow-up care needs, awareness of error risk to prevent errors, dialogue, questions, ownership/custody, document, and thank you (Nasarwanji et al., 2016). Two common examples of standardized communication methods discussed are situation-background-assessment-recommendations (SBAR) and checklists:
- SBAR is discussed in more detail in content about teams, but it is important to recognize that this method is part of CQI. It is used to prevent QI problems by ensuring clear communication during times when important information is required. It is easy to get off track in communication, but during communication from one healthcare provider to another, such as a nurse calling a physician about a patient, it is important to stay on track. SBAR and other similar methods help to focus the conversation (IHI, 2023f).
- Checklists are also discussed in content about teams, but it is a method or tool used as part of CQI. It is a common tool used to guide staff during certain aspects of care with the goal of ensuring that critical steps are taken. Teams provide collective vigilance when they use checklists to identify potential risks of errors or to quickly identify when an error has occurred, shifting from individual accountability and thus providing a better chance to catch a missed error or potential error (Jeffs et al., 2012). The most common area of use is in surgery-prior to surgery and/or after surgery. When checklists are used, any staff member may interrupt and ask questions-for example, a step was missed, or something was done that should not have been done according to the checklist. This method may be used in many situations, but the HCO should have clear and approved checklists that staff understand. Staff should be involved in the development of checklists, provide feedback for improvement, and consistently use HCO checklists, as a checklist that is not used is ineffective. Use of checklists not only acts as a method to prevent CQI problems, but this tool may also provide useful CQI data.
Rounds and Shift Reports
Rounds have been used in health care for a long time. The types of rounds, however, have changed over time. Rounds provide an opportunity to gain information through observation and communication. They may be used by an individual staff member to check assigned patients or by teams, which may be profession specific (such as a nursing team or physicians/residents/medical students) or interprofessional. All units should use some form of interprofessional rounds to ensure consistent assessment, clearer communication, and planning for patient care. Some HCOs use nurse-led interprofessional bedside rounds and apply a structured method, such as Plan-Do-Study-Act process (PDSA) (Gormley et al., 2019). In this example, staff members use a standardized communication plan with a clear delineation of roles for team members during the rounds. Teams can be varied, including staff from nursing, medical, respiratory therapy, pharmacy, dietary, social services/case management, and management. It is important to periodically evaluate rounds and get feedback from those who participate-and use this information to improve. Some common issues that act as barriers to success are difficulty getting a time that works for most staff, allowing the patient to participate with consideration of patient privacy, inconsistent participation from staff, and poor structure, making it difficult to complete what needs to be done during the rounds, and time limitations that may impact routine work.
Rounds do not always focus directly on the patient. Some rounds are teaching rounds led by medical staff, or nursing education rounds. There may also be administrative or management rounds when the nurse manager makes rounds in the unit (demonstrating the role of the bedside leader) and focuses on issues such as safety, cleanliness, and work environment. They may also observe patient care in the process or talk to patients and families. Safety rounds may be used when certain staff, often managers, but also clinical staff, use rounds in the unit to assess staff and patient safety risks.
Clinical rounds focus on the patient and should include patient engagement, which may seem strange, but it is important. In the past, rounds were often done around the patient with little effort made to include the patient. It is also important to recognize that rounds may disturb patients, for example, interrupting rest and quiet, patient concerns about privacy, and patient concerns that others may be making decisions in which they have no input or limited input.
Rounds may be routine or unscheduled, such as when a nurse decides to check assigned patients. Routine rounds happen at scheduled times, with specific staff involved, and the purpose is clear. Documentation may be part of rounds, either during rounds, which is typical, or immediately after rounds. CQI concerns may be identified during rounds. If so, they require follow-up. HCOs should have policies and procedures about rounds and how they relate to the QI program.
The shift report is another routine communication method used. Some of these reports are conducted only with staff present and others may be conducted at the bedside with the patient integrated into rounds and the report. It is important for reports to be consistent and required (Schneidenhelm & Reitz, 2019). It is not only a method to ensure clearer communication on a routine basis, but also, if used at the bedside, it engages the patient in the care planning process, which is more effective than just a staff-focused report. Patients are more satisfied with this type of communication. Care needs to be taken to ensure that the patient understands the conversation and that staff do not slip into jargon that cuts the patient out. Nurse managers need to support this type of report and attend reports as needed.
Incident Reports
Incident reports have long been used by HCOs as a method for staff to report errors or care problems. HCOs have policies and procedures to guide staff in the use of incident reports. An HCO standardized form is completed by staff involved in an event. The HCO identifies the types of events that require reporting. These forms are used by the QI program to track events, such as infections, medication errors, treatment and procedure errors, patient complaints, falls, security issues, harm to staff, sentinel events, and regulatory compliance (HHS, OIG, 2012). Management, including nursing management, reviews the reports to provide up-to-date information on CQI and assist in identifying situations that require an immediate response. Incident reports have been used in “blame cultures” to identify staff involved and then to identify the steps to take to resolve problems, focused on staff actions and the staff member-often leading to punitive responses. This has been described as the “blame game” (IOM, 1999). Over time, this had a negative impact on staff completion of incident reports, which is not helpful because valuable information is lost (HHS, OIG, 2012). This underreporting leads to missed opportunities to improve (Copeland, 2019). It is critical that staff engage in this process to improve; for example, HCOs might emphasize staff awareness of actual and potential safety events, provide more staff education on safety, increase leader visibility and guidance, avoid punitive measures, encourage transparency, and use huddles and rounds to discuss real patient safety issues (Copeland, 2019). There is now more effort in cultures of safety to view incident reports as a source of data to be used in HCO QI efforts to assess care processes from a system perspective, moving away from the blame game.
Sentinel Events
As described earlier, sentinel events are “unexpected events that happen to patients resulting in major negative outcomes, such as unexpected death or critical physical or psychological complications that can lead to major alteration in the patient's health” (Finkelman, 2022, p. 221). These are events that require an immediate response-for example, a suicide in the hospital, wrong-site surgery, or a life-threatening postoperative complication. Staff responsible for CQI must analyze the event (use of root-cause analysis [RCA], discussed in the next section) and collaborate with other staff to respond. The Joint Commission publishes sentinel event alerts on its website based on the information it receives from its accredited HCOs. This information is provided so that others can be alert to potential risks, some are identified in this content (The Joint Commission, 2023h). Not all errors are sentinel events, and HCOs need to determine if the event is classified as a sentinel event. Often, sentinel events are unique or happen rarely, but response is required, including steps to prevent reoccurrence.
| Stop and Consider 9 |
|---|
| There are many methods and tools used to prevent or resolve quality care concerns. |
Measurement and Analysis
Measures/indicators provide performance data to better understand actual practice, identify problems, and assist in best practice changes for improvement by identifying topics that will be monitored to determine performance and expected outcomes. A measure is a “standard used as a basis for comparison, a reference point against which other things can be evaluated, and indicators are measures of healthcare quality” (HHS, AHRQ, 2018). Data from indicators provide information about potential quality concerns and areas that need more examination and help track changes over time. “Measuring a health system's inputs, processes, and outcomes is a proactive, systematic approach to practice-level decisions for patient care and the delivery systems that support it. Data management also includes ongoing measurement and monitoring. It enables an organization's CQI team to identify and implement opportunities for improvements of its current care delivery systems and to monitor progress as changes are applied. Managing data also helps a CQI team to understand how outcomes are achieved, such as improved patient satisfaction with care, staff satisfaction with working in the organization, or an organization's costs and revenues associated with patient care” (HHS, HRSA, 2023). It is important to recognize that once something is identified as a measure, this puts that situation or action on the list of important activities-it draws attention to the issue and typically means staff will pay more attention to the issue, and more resources may be directed at interventions to prevent or resolve a problem. This may or may not be a positive result-for example, if the measure is not that important, something that is more important may be ignored.
Measurement must be planned, evaluated, and revised as needed. The HCO QI program is responsible for the measurement plan and then its implementation. “It is critical that an HCO's QI program and plans identify clear steps to be taken to ensure that the CQI activities have direction. This direction is provided by overall goals, which typically are universal and often focus on the six aims (STEEEP®); however, more specific direction is required. Measures/indicators provide this direction to assist in reaching the overarching goals” (Finkelman, 2022, pp. 329-330).
Data Collection
An HCO QI program collects data to monitor and assess its CQI status. There are many sources of data. Some of the sources are designed specifically to collect CQI data. Other sources, such as medical records, are primarily used to document patient care for clinical purposes-sharing information; documenting what will be done and what was done; records of testing, procedures, and medication administration; monitoring, such as vital signs; and so on (Soriano et al., 2019). This, however, is also valuable data for CQI. When using data from methods that were not primarily designed for CQI data collection, there is some risk that the data will not provide the needed information; and data may be missing, not understood, or difficult to retrieve. The QI program must plan carefully what data will be collected and the best source for the data.
The focus previously mentioned examined HCO data collection; however, CQI data are also collected for broader purposes. The government (state and federal) collects data, as has been discussed in this text for Healthy People 2030, the NHQDR, NQS, CMS programs, and many other initiatives. The NDNQI is an example of a health profession database (nursing) that requires data collection. The Joint Commission and the Magnet Recognition Program® also collect data from HCOs that are accredited or recognized by these organizations. Data collection and measurement are complex processes and, at times, confusing with multiple measures and indicators.
Analysis
Data analysis or review of performance based on data is a complex process conducted by HCO QI programs. The goal is a better understanding of the data. The data may be analyzed from a broad perspective, such as data about all HCO medication errors; from a more focused perspective, such as intensive care unit medication errors or the HCO's intravenous medication errors; may compare data using benchmarking, for example, comparisons with other, similar HCOs or comparing clinical units within one HCO; and the analysis may focus on specific incidents using root cause analysis (RCA) to understand an incident or event. Root cause analysis is now used by most HCOs, particularly hospitals. It is an error analysis process that recognizes when an error occurs system factors are more important than individuals. The RCA process includes the following steps (Finkelman, 2022; HHS, AHRQ, PSNet, 2019a):
- Select the team to complete the RCA. The team should include experts related to the event. For example, if the error occurred in surgery, team members should include representatives of the surgical staff from the operating room, anesthesiology, and other relevant healthcare professionals, such as other surgeons and nurses, laboratory technicians, radiologists, infusion team members, pharmacists, infection control staff (depending on the error), and management. Staff educators may also participate. The size of the analysis team may vary.
- As the team analyzes the situation and the error, it creates a flow chart describing the situation.
- The team then examines the flow chart for areas of failure.
- The team uses CQI tools to consider the data collected and possible root causes.
- The team redesigns the process for improvement (if required) based on the analysis results.
- The HCO implements the changes, ideally first through a pilot, and then spreads the changes to other areas of the HCO as appropriate for the improvement strategy/intervention.
Key questions the RCA team asks during the process are:
- What happened?
- Who was involved?
- When did it happen?
- Where did it happen?
- What is the severity of the actual or potential harm?
- What is the likelihood of reoccurrence?
- What are the consequences?
The team analyzing the problem or error may use brainstorming, flow charts, or cause-effect diagrams to clearly describe the problem and factors related. Typical contributing factors are categorized, such as (Finkelman, 2022, p. 363):
- Environmental factors (for example, work environment, staff safety, safety culture type, ethical-legal concerns)
- Organizational factors (for example, staffing levels/mix, staff availability and roles, support staff, clear policies, administrative support, effective leadership, access to equipment and supplies, documentation, use of rounds and other communication methods, attitudes toward patients and families/patient/person-centered care)
- Staff/team (for example, supervision of staff, communication, team membership, quality of teamwork, team leadership and functioning, availability of expertise)
- Individual staff factors (for example, level of knowledge, competency, and experience, fatigue, stress, expectations, position description, staff safety)
- Task factors (for example, clear protocols and/or guidelines, use of checklists, lab tests and other procedures, description of tasks, policies)
- Patient factors (for example, stress, communication, accessible patient information, diversity factors, comorbidities, status on admission, history, 30-day unplanned readmission, discharge plans)
Work in healthcare environments is complex, and many factors affect how staff perform (Roth et al., 2015). Common human factors that affect staff performance, and thus quality care, are fatigue and sleep problems, stress, incivility, hunger, illness, unfamiliarity with a task, inexperience, shortage of time, inadequate checking, interruptions, noise, unclear procedures, unwillingness or inability to ask for help, and language and cultural factors (Finkelman, 2022). Recognizing these factors can be helpful in developing strategies to improve care by preventing these factors or reducing them.
The RCA must lead to clear views of issues so that the analysis results can be used to plan interventions to prevent problems or solve problems. Gap analysis, described earlier in this content, may be part of the process-identification of where you want to be and comparison with status. Staff members need to be informed about the analysis and results. If they are not informed, it is very difficult to engage them in CQI. Nurses should be involved in all phases of analysis.
| Stop and Consider 10 |
|---|
| Nurses should be involved in CQI measurement and analysis. |
Patient Outcomes and Nursing Care: Do We Make a Difference in Quality Improvement?
Keeping Patients Safe: Transforming the Work Environment of Nurses (IOM, 2004b) is an early Quality Chasm report that focused on acute care; however, it is relevant here because much of the content can still be applied to nursing and to a variety of healthcare settings. This report also has a different focus from the later reports The Future of Nursing, Leading Change, Advancing Health (IOM, 2010) and The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (NAM, 2021). The 2004 report stated, “When we are hospitalized, in a nursing home, or managing a chronic condition in our own homes-at some of our most vulnerable moments-nurses are the healthcare providers we are most likely to encounter, spend the greatest amount of time with, and be dependent upon for our recovery” (IOM, 2004b, p. ix). This report emphasized designs for a work environment in which nurses could provide safer, higher-quality patient care. The content discussed changes in nursing shortage and staffing, healthcare errors, patient safety risk factors, the central role of the nurse in patient safety, and work environment threats to patient safety. In discussing errors, the focus moved away from a punitive, blaming environment and emphasized the need to view errors more from a system perspective, supporting the major message from To Err Is Human (IOM, 1999). Some of the factors that influence errors from a system perspective were highlighted in this report, including equipment failures, inadequate staff training, lack of clear supervision and direction, and inadequate staffing levels-all of which continue to be CQI concerns. The central message in the report was the healthcare work environment needed to be transformed, and this is viewed as an ongoing need and need for greater emphasis on health equity. The 2004 critical nursing report identified six major concerns for direct care nursing, which continue to be relevant (IOM, 2004b):
- Monitoring patient status or surveillance: This is different from assessment. Surveillance is defined as “purposeful and ongoing acquisition, interpretation, and synthesis of patient data for clinical decision-making” (McCloskey & Bulechek, 2000, p. 629). If surveillance is not effective, the result may be described as failure to rescue-missing an opportunity to prevent complications.
- Physiologic therapy: This is the most common visible intervention performed by nurses.
- Helping patients compensate for loss of function: Teamwork is important to accomplish this goal.
- Providing emotional support: This is a critical need for patients and their families.
- Education for patients and families: This is often difficult to accomplish due to work conditions, staffing levels, patient acuity, and shorter lengths of stay.
- Integration and coordination of care: Complex patient needs and care often require multiple forms of care provided by different providers.
The report recommended (1) adopting transformational leadership and evidence-based management, (2) maximizing the capability of the workforce, (3) understanding work processes so that they can be improved, and (4) creating and sustaining cultures of safety (IOM, 2004b). Nursing leadership must be very active throughout the HCO, representing staff, supporting the need for effective change, facilitating input from direct care nursing staff, and expanding communication and collaboration. Leadership is a recurring theme throughout this text. HCO leadership needs to support ongoing staff learning-for example, through effective orientation for an appropriate length of time, ongoing staff education, nurse residency programs, funding support for nurses to return to school to complete higher degrees, establishing partnerships with schools of nursing, providing opportunities for interprofessional educational experiences, and so on. All of this requires resources that management must ensure are available-for example, adequate staffing is critical. All HCOs struggle with the challenges of how best to fill positions and retain staff. Excessive documentation can lead to less time for patients, which can affect safety and quality. There is a need for effective computerized documentation with decision-making support. Work design includes issues related to physical space, for example, lighting, size of the unit, and the ability to get to equipment easily and quickly, all affect staff and patient safety (IOM, 2004b, 1999). The Future of Nursing report also emphasizes nursing leadership and the need for nurses to be leaders in HCOs and in CQI (IOM, 2010, NAM, 2021). Woven throughout all the recommendations for these major reports on nursing is the need for EBP-basing decisions on evidence for quality care.
Based on what is known about CQI and its importance, it is natural to assume that nurses are very active in CQI and have assumed leadership in improving care, but this is not necessarily the case, particularly for new nurses. When a 2008 survey on this topic was sent to nurses who graduated between 2004 and 2005, 436 responded (a rate of 69.4%). According to the researchers, “Overall, 159 (38.6%) of new nurses thought that they were ‘poorly' or ‘very poorly' prepared about or had ‘never heard of' QI. Their perceptions of preparation varied widely by the specific topic. Baccalaureate (BSN) graduates reported significantly higher levels of preparation than associate degree (ADN) graduates in EBP; assessing gaps in practice, teamwork, and collaboration; and many of the research-type skills such as data collection, analysis, measurement and measuring resulting changes” (Kovner et al., 2010, p. 29). The data are from several years ago, but during that time, there should have been a greater emphasis on CQI in nursing education given the many initiatives to examine the need for better CQI.
Subsequently, a second study was done that compared the 2004-2005 graduates with graduates from 2007-2008 (539 RNs who worked in 15 states). Not much difference was apparent in their responses, indicating little had changed in nursing education to better prepare new nurses for CQI (Djukic et al., 2013). Although more hospitals are providing staff education on CQI for new graduates, hospitals in general need to collaborate more with schools of nursing so that nursing graduates are better prepared, and then there will be less need for HCO QI staff education directed at new graduates, which is costly for the hospitals.
A 2015 publication discussed education gaps and solutions for early-career, frontline nurse manager education, and participation in CQI (Djukic et al., 2015). These are key concerns that need to be addressed to improve care. We need leaders at all levels in CQI, but unit managers have a major impact on CQI and in increasing staff nurse engagement, but are these managers prepared to meet this goal? A sample of 42 early-career, frontline nurse managers was part of a study examining this issue. The results indicated that about 30% of the sample thought they were very prepared based on 12 CQI indicators. Thirty-five percent of the sample noted they were engaged in specific clinical efforts to improve care on their unit more than once a month. More than 50% indicated that they received good organizational support for CQI efforts, with 30% receiving rewards for their CQI contributions. This study demonstrated that some nurse managers were prepared and participated, though the sample for the study was small. The authors of all of these studies indicated that more needed to be done in nursing education on this critical content to help students see the connection between CQI concepts and practice (Altmiller & Hopkins-Pepe, 2019).
It is clear nurses need to participate actively in local, state, and national initiatives to improve care. Although historically nurses have provided weak CQI policy leadership, this is changing. Active nurse engagement at all levels will make a difference in effective CQI efforts. We need to continually assess our impact in QI. For example, the American Association of Critical-Care Nurses (AACN) conducted a study to examine calculated decisions nurses made to not speak up about errors (Maxfield et al., 2011). One aspect of the study examined the use of four common survey safety tools (universal protocol checklist, WHO checklist, SBAR used with a handoff protocol, and drug-interaction warning systems). In this study, nurses were asked how often they had been in situations where one of these tools was effective, warning them of a problem that might have been missed and patient harm if a tool had not been used. The results indicated that 85% (2,020) of the nurses said they had been in this situation at least once, and 29% (693) said they experienced this situation at least a few times a month. This indicated that these tools make a difference and lead to improved care. The data from this study was also examined to describe the effectiveness of these safety tools, which may be undercut by “undiscussables” as noted in their sample: 58% (1,403) of the nurses said they had been in situations where it was either unsafe to speak up or they were unable to get others to listen. Seventeen percent (409 of the 1,403) of the sample said they were in this situation at least a few times a month. This type of data attests to the complexity of CQI. Understanding data requires consideration of the problems; the challenges in identifying, monitoring, and measuring the problems; and the influence of human factors. Findings reported in this “silent treatment” study demonstrated that only a small minority of nonsupervisory nurses spoke up when they had a concern related to dangerous shortcuts, incompetence, or disrespect. Only 9% spoke up in all three of these situations, and only 14% spoke up in two of the three. Thus, it is important to support staff to share experiences about near misses, patient injuries, or examples of when they discussed error prevention and harm to a patient. Staff can relate more to descriptions of these experiences, and it is easier for staff to remember them.
Nurses should engage in error recovery. We know that not all errors can be prevented, though we are making efforts to reduce errors. Medical error recovery “includes identifying, interrupting, and correcting medical errors in a timely fashion” (Gaffney et al., 2016, p. 906). When a near miss occurs, nurses may not complete what needs to be done for error recovery. A systematic review of studies on error recovery noted that nurses typically used strategies to identify, interrupt, and correct errors that included knowledge of the patient and the patient's problems, knowledge of the environment, and awareness of the plan of care (Gaffney et al., 2016). Nurses gain this knowledge, which may affect error recovery, through collection of data, surveillance, communicating with others (team), continuity of care, asking questions, and sharing information. “When these strategies were not effective, being physically present was key in verbally interrupting or creating delays to correct potential errors” (Gaffney et al., 2016, p. 914). The development of clinical judgment comes with experience, and this assists in error recovery.
Other ways that more nurses can participate in the quality agenda are through the development and implementation of standards; involvement in shared professional governance and decision-making about CQI; serving on CQI committees in HCOs and for professional organizations; engaging in health policy development at the local, state, and national levels; undertaking research and using evidence to improve practice; and engaging in active discussions with colleagues and other healthcare professions about CQI. There is a need for change in the healthcare system, and the following continues to be critical:
The 21st century healthcare system envisioned by the committee-providing care that is evidence based, patient/person-centered, and systems oriented-also implies new roles and responsibilities for patients and their families, who must become more aware, more participative, and more demanding in a care system that should be meeting their needs. And all involved must be united by the overarching purpose of reducing the burden of illness, injury, and disability in our nation. (IOM, 2001a, p. 20)
| Stop and Consider 11 |
|---|
| Every nurse must engage in CQI every day. |