This chapter expands on content related to this section of the text that focuses on the healthcare professions core competencies with a discussion of the fifth core competency: utilize informatics/health information technology (IT), which is an important topic in all areas of life today (IOM, 2003) and is included in the Quality and Safety Education for Nurses (QSEN, 2021) competencies. With the explosion of technology, there are many opportunities for communication and sharing of knowledge. The impact of health information technology (HIT) on nursing care is explored here. Other issues that need to be addressed are documentation; confidentiality and privacy of information; and information technology methods used in practice, education, and research. This chapter also includes content about biomedical equipment or medical devices, an expanding area in healthcare technology that affects nurses and nursing care. Some of this equipment also uses IT. Nurses today cannot avoid technology, whether it is used in communication, care provision, or monitoring the quality of care. The chapter concludes with a discussion about the potential conflict between high-touch care versus high-tech care and the need for nursing leadership in health information/informatics, which are important issues for nurses to consider. Figure 13-1 identifies key elements in this competency.
Figure 13-1 Utilize informatics: Key elements.
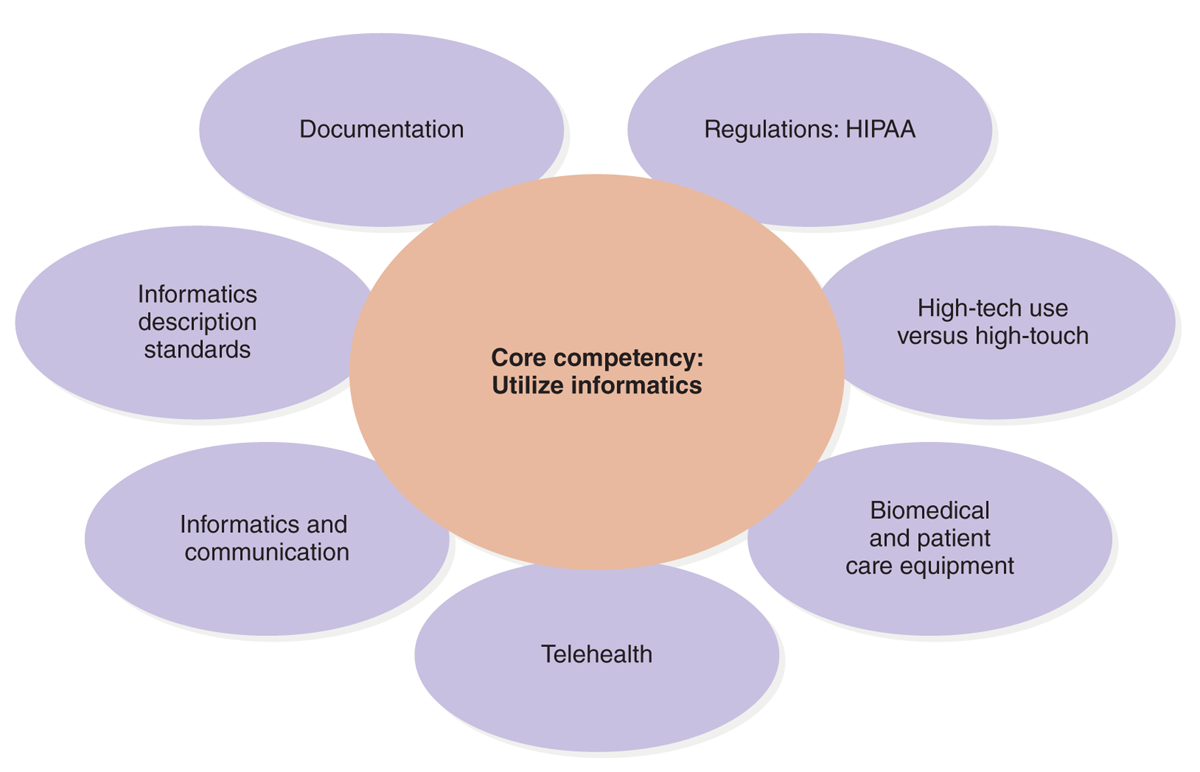
An illustration outlines the key elements of utilizing informatics.
The core competency: utilize informatics is at the center. Surrounding it are the key elements: Documentation, Regulations: H I P A A, High-tech use versus high-touch, Biomedical and patient care equipment, Telehealth, Informatics and communication, and Informatics description standards.
The Core Competency: Utilize Informatics/Health Information Technology
The fifth healthcare profession core competency is “communicate, manage knowledge, mitigate error, and support decision making using information technology” (Institute of Medicine [IOM], 2003, p. 4). Informatics/health information technology entails more than just understanding the meaning of HIT and its clinical implications. It also includes how that technology is used to prevent errors and improve care, particularly in the measurement and analysis of care data. From the initial use of computers to share information, management of financial records, and the current use of informatics with more emphasis on patient care, there has been a major move toward IT application in health care or HIT. Some examples are greater use of IT to find evidence to implement evidence-based practice (EBP); use of IT in research; greater consumer access to information via the internet; and more specific clinical applications, such as reminder and decision systems and digital health, including telehealth/telemedicine, online prescribing, use of email for provider-provider communication and patient-provider communication, and the use of smartphones and apps. The Quality Chasm report on healthcare professions' core competencies concluded that every healthcare professional should meet the following IT competencies (IOM, 2003, p. 63):
- Employ word processing, presentation, and data analysis software.
- Search, retrieve, manage, and make decisions using electronic data from internal information databases and external online databases and the internet.
- Communicate using email, instant messaging, email lists, and file transfers.
- Understand security protections, such as access control, data security, and data encryption, and directly address ethical and legal issues related to the use of IT [HIT] in practice.
- Enhance education and access to reliable health information for patients.
A position statement from the Healthcare Information and Management Systems Society (HIMSS, 2015) addressed The Future of Nursing (IOM, 2011) report from the perspective of IT. The following summarizes the HIMSS recommendations that were made and aligned with The Future report on the key points of nursing leadership, education, and practice (HIMSS, 2015):
- Partner with nurse executives to lead technology changes that advance to improve healthcare delivery.
- Develop informatics departments.
- Establish the chief nursing informatics officer role.
- Include informatics competencies and demonstrable behaviors at all levels of nursing education.
- Promote nursing continuing education, e.g., electronic health records (EHRs), HIT.
- Incorporate informatics competencies into practice standards in all healthcare settings.
- Collect and analyze interprofessional healthcare workforce data by ensuring data.
The statement also indicated that nurses have a critical role in HIT, which has led to expanded roles for nurses-there is strong support for nursing leadership in HIT. “Nurses are key leaders in developing the infrastructure for effective and efficient health information technology that transforms the delivery of care. Nurse informaticists play a crucial role in advocating both for patients and fellow nurses who are often the key stakeholders and recipients of these evolving solutions. Nursing informatics professionals are the liaisons to successful interactions with technology in healthcare” (HIMSS, 2015).
| Stop and Consider 1 |
|---|
| Every nurse applies the informatics/health information competency. |
The Federal Health Informatics Reports
The federal government increased its involvement in HIT, particularly through the U.S. Department of Health and Human Services (HHS), Office of the National Coordinator for Health Information Technology (ONC). This federal government office published Health Information Technology: Patient Safety Action & Surveillance Plan, which identifies advantages for greater use of the electronic medical record (EMR) and is now a critical tool used in many healthcare organizations (HCOs) (HHS, ONC, 2013, pp. 5-6):
- Increase clinician awareness of potential medication errors and adverse interactions.
- Improvement of the availability and timeliness of information to support treatment decisions, care coordination, and care planning.
- Make it easier for clinicians to report safety issues and hazards.
- Give patients the opportunity to provide input more efficiently on data accuracy than information allowed on paper records.
These advantages also link EMRs to quality improvement (QI). The increased use of electronic records was initially driven and is still driven by important federal legislation, the Health Information Technology for Economic and Clinical Health Act of 2009 (HITECH). All of this set the stage for greater federal involvement in HIT.
As part of its HIT initiatives, the HHS published a report, Connecting Health and Care for the Nation: A Shared Nationwide Interoperability Roadmap, Draft Version 1.0, describing a road map supporting interoperability or “the ability of a system to exchange electronic health information with and use electronic health information from other systems without special effort on the part of the user” (HHS, ONC, 2023). This is a critical element in making HIT more accessible and sharing information across systems and providers. This report was followed by the Federal Health IT Strategic Plan, now in its 2020-2025 version, with the following vision guiding the plan: “A health system that uses information to engage individuals, lower costs, deliver high quality care, and improve individual and population health” (p. 3). Figure 13-2 describes the framework for this strategic plan. The key issue is access to information when people need it. This is a good example of how HIT is not just about computers and software. There needs to be a relationship between technology and care delivery-needs, standards, and outcomes and the engagement of key stakeholders. HIT should be used to (HHS, ONC, 2020):
Figure 13-2 2020-2025 Federal Health IT Strategic Plan Framework.
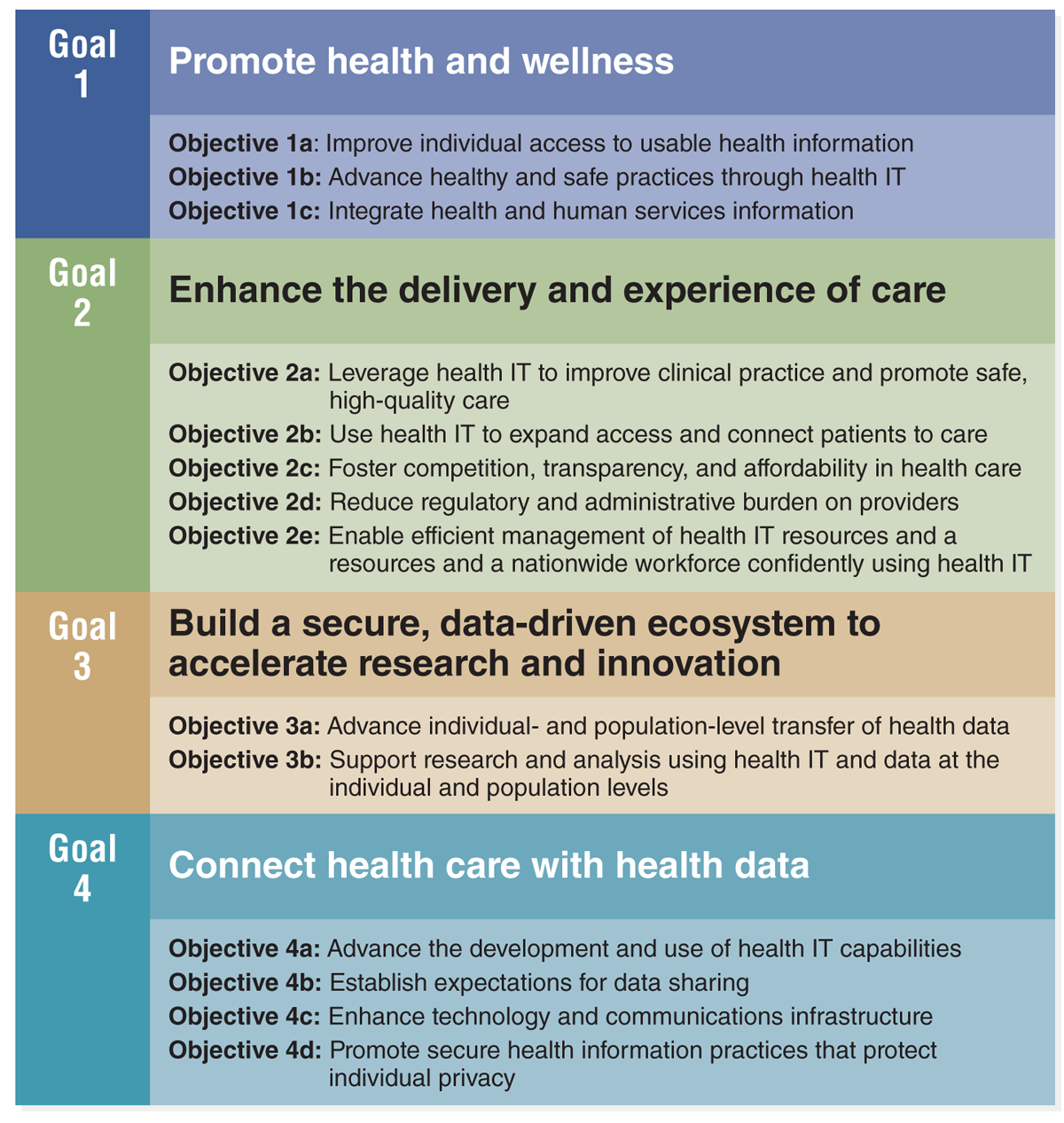
A chart outlines the goals and objectives for promoting health I T.
The chart is divided into four goals: Goal 1: Promote health and wellness. Objective 1 a: Improve individual access to usable health information, Objective 1 b: Advance healthy and safe practices through health I T, Objective 1c: Integrate health and human services information. Goal 2: Enhance the delivery and experience of care. Objective 2 a: Leverage health I T to improve clinical practice and promote safe, high-quality care, Objective 2 b: Use health I T to expand access and connect patients to care, Objective 2 c: Foster competition, transparency, and affordability in health care, Objective 2 d: Reduce regulatory and administrative burden on providers, Objective 2 e: Enable efficient management of health I T resources and a nationwide workforce confidently using health I T. Goal 3: Build a secure, data-driven ecosystem to accelerate research and innovation. Objective 3 a: Advance individual- and population-level transfer of health data, Objective 3 b: Support research and analysis using health I T and data at the individual and population levels. Goal 4: Connect health care with health data. Objective 4 a: Advance the development and use of health I T capabilities, Objective 4 b: Establish expectations for data sharing, Objective 4 c: Enhance technology and communications infrastructure, Objective 4 d: Promote secure health information that protects individual privacy.
2020-2025 Federal Health IT Strategic Plan Framework. U.S. Department of Health and Human Services (HHS). Agency for Healthcare Research and Quality (AHRQ), Office of National Coordinator for Health Information Technology (ONC). (2020). https://www.healthit.gov/sites/default/files/page/2020-10/Federal%20Health%20IT%20Strategic%20Plan_2020_2025.pdf
- Promote health and wellness.
- Enhance the delivery and experience of care.
- Build a secure, data-driven ecosystem to accelerate research and innovation.
- Connect health care with health data.
There has been increased expansion in HIT use, and because of this the HHS, through the ONC, must now report annually to Congress on the status of HIT. Prior to 2009, most HCOs-including hospitals, physician practices, clinics, and so on-used paper documentation. Sharing information was often done using fax machines, but this has changed.
Annual Update on the Adoption of a Nationwide System for the Electronic Use and Exchange of Health Information. Department of Health & Human Services (HHS) is committed to maximizing the promise of health information technology as a critical component in our efforts to accelerate value-based transformation in health care. HHS is committed to the use of HIT to support the free flow of health information for patients, healthcare providers, and payers as well as to promote competition in healthcare markets. Seamless data flow also accelerates progress on a range of national health priorities that include combatting the opioid epidemic, spurring clinical innovation, and accelerating science. For the past decade, the ONC has been the principal federal entity charged with supporting a nationwide HIT infrastructure, which allows for the electronic access and use of health information. Today, most hospitals and healthcare providers have a digital footprint, information about them that can be found online. As of 2021, nearly four in five office-based physicians (78%) and nearly all nonfederal acute care hospitals (96%) have adopted a certified EHR. This marks a substantial 10-year progress since 2011 when 28% of hospitals and 34% of physicians had adopted an EHR (HHS, ONC, 2022). The increase in the adoption of HIT means most Americans receiving healthcare services now have their health data recorded electronically. However, this information is not always accessible across systems and by all end users-such as patients, healthcare providers, and payers-in the market in productive ways.
Now, more emphasis is placed on creating a more effective, seamless, and secure system that considers interoperability across system components or multiple systems. Value-based care is more important, emphasizing quality, effective outcomes, and lower costs, all of which require effective use of IT, but there are problems that need to be addressed to transition to value-based care. “Provider organizations pursuing new models of healthcare delivery and payment are finding that their electronic systems lack the capabilities needed to succeed. The result is a chasm between the current health IT ecosystem and the health IT ecosystem that is needed” (Adler-Milstein et al., 2017, pp. 1-2).
There is better understanding of what needs to be done to improve the healthcare system, but the problem is one of getting it done, implementing it. We need more than a collection of systems that currently do not support value-based care-better care outcomes at lower cost. Healthcare providers need an effective integrated HIT environment.
| Stop and Consider 2 |
|---|
| The federal government is very involved in ensuring effective health information technology. |
Informatics/Health Information Technology
Informatics/health information technology is complex, and the fact that it changes makes it even more difficult to keep current with this field. Healthcare delivery has been strongly influenced by the changes in IT, but what is IT, and why is it important? Some nurses may hold HIT positions in HCOs, as discussed later in this chapter, but all nurses use HIT in their positions-it is not an area that only concerns a specific nursing specialty. In addition, we are experiencing a time of significant change, some of it initiated by our experiences with COVID-19, but there has been increased technology development. “Nurses are committing to developing and putting novel technologies into practice to meet essential global health goals. Along with their unique and valuable knowledge and abilities to tackle these challenging healthcare objectives, nurses serve as crucial change agents in the creation and application of technological functionality that bridge the delivery of healthcare and social needs in both urban and rural communities. This trend will only increase in the next decade and beyond” (Carroll, 2020).
Informatics/health information has opened doors to many innovative methods of communication with patients and among providers, individuals, and HCOs of all types, and some of them are discussed in this chapter. HIT often saves time, but it can also lead to information overload. With these changes also comes greater risk of inappropriate access to information through hacking and other means. HIT is also used to evaluate HCO and individual healthcare provider performance. The use of HIT has a major impact on quality improvement (Finkelman, 2022). Today, it is much easier to collect, store, and analyze large amounts of data that, in the past, were collected by hand. Insurers rely heavily on HIT as they provide insurance coverage, manage data, and analyze performance, which has a direct impact on whether care is covered for reimbursement. This allows governments at all levels-local, state, national, and international-to collect and use data for policy decision-making and evaluation and allows for greater development of national and statewide quality improvement efforts as well as global comparisons. The World Health Organization (WHO) notes that “digital transformation of health care can be disruptive; however, technologies such as the Internet of things, virtual care, remote monitoring and management, artificial intelligence, big data analytics, blockchain, smart wearables, platforms, tools enabling data exchange and storage and tools enabling remote data capture and the exchange of data and sharing of relevant information across the health ecosystem creating a continuum of care have proven potential to enhance health outcomes by improving medical diagnosis, data-based treatment decisions, digital therapeutics, clinical trials, self-management of care and patient/person-centered care as well as creating more evidence-based knowledge, skills and competence for professionals to support health care (WHO, 2020, p. 4).
HIT has its own language and is a highly specialized area. Nurses do not have to be HIT experts, but they do need to understand the basics. Some common HIT terms that most people know are internet/WIFI and email. Examples of other terms that nurses should know are highlighted here (Glassman & Rosenfeld, 2015):
- Clinical data repository: This is a physical or logical compendium of patient data pertaining to health; an information warehouse used to store data longitudinally, in multiple forms (text, voice, images, and so on).
- Clinical decision support systems (CDSS): These systems are computer applications designed to facilitate human decision-making. Decision support systems are typically rule based, using a knowledge base with a set of rules to analyze data and information to reach recommendations.
- Clinical information system: This is an information system that supports the acquisition, storage, manipulation, and distribution of clinical information throughout an HCO, with a focus on electronic communication, using HIT applied at the point of clinical care. Typical clinical information system components include EMRs/EHRs, clinical data repositories, decision support programs (such as the application of clinical guidelines and checking drug interaction), handheld devices for collecting data and viewing reference material, imaging modalities, and communication tools, such as electronic messaging systems.
- Coding system: This is a set of agreed-on symbols (frequently numeric or alphanumeric) associated with a concept representation or terms to allow the exchange of meaning. Examples are the Syntegrity Perioperative Nursing Data Set (PNDS) and the Clinical Care Classification System.
- Computer literacy: Specific knowledge and skills are required to use basic computer applications and computer technology.
- Cybersecurity protections: These methods, such as access control, data security, and data encryption, ensure that information is not read or taken by unauthorized persons.
- Dashboard: This is a method used to provide a quick view of data guided by key elements to assist in organizing the information.
- Data: These are discrete entities described objectively without interpretation.
- Data analysis software: This type of computer software is used to analyze data and used in health care to meet regulatory requirements, performance assessment and quality improvement, accreditation, and research.
- Data bank: This method is used to store a large amount of information; may include several databases.
- Database: This represents a collection of interrelated data organized according to a scheme to serve one or more applications with data stored so that several programs can use the data without concern for data structures or organization. An example is the National Database of Nursing Quality Indicators (NDNQI), discussed in other content in this text.
- Data mining: This is a method used to locate and identify unknown patterns and data relationships.
- Email list: This is a list of email addresses that can be used to send an email to many addresses simultaneously.
- Encryption: This is a method used to change information into a code, usually for security reasons to limit access to that information.
- Information: This represents data that have been interpreted, organized, or structured.
- Information literacy: This is the ability to recognize when information is needed and then to locate, evaluate, and effectively use that information.
- Minimum data set: This describes the minimum categories of data with uniform definitions and categories; concerns a specific aspect or dimension of the healthcare system that meets the basic needs of multiple data users.
- Nomenclature: This is a system of designations (terms) that is elaborated on according to preestablished rules. Examples include Systematized Nomenclature of Medicine (SNOMED CT) and International Classification for Nursing Practice.
- Scorecard: This is a metric method used by management to assess and track performance, typically related to the HCO's agenda or to a specific unit, service, or department; it can focus on clinical, financial, and other indicators. Another term that may be used is report card.
Data science has become more relevant in nursing: “Whether predicting clinical deterioration, adverse events, or even changes in patient census, data inform clinical care. Nurses play a major role in entering data into electronic health records (EHRs), and we should be using available tools to analyze and use these data to improve care delivery. Although significant advances have been made in collecting and analyzing the large amount of healthcare data now available, clinicians can be easily intimidated by some data science concepts, such as machine learning and artificial intelligence” (Jeffery, 2022, p. 32). Data science includes gathering, preparing, exploring, representing, transforming, computing (with), modeling, visualizing, and presenting data, which applies to nurses in practice, management, research and nursing education.
The role of HIT in e-measurement and quality care has expanded in recent years (Dykes & Collins, 2013). E-measurement is the secondary use of electronic data when using standardized performance measures (NQF, 2023). The National Quality Forum (NQF) is engaged in ensuring that effective e-measures are available so that data can be used for clinical documentation and may be reused to measure clear and consistent patient outcomes. This endeavor, which is very complex, continues.
A current problem in our everyday lives and our professional lives is information (cognitive) overload, which is an “interpretation that people make in response to breakdowns, interruptions, interruptions of ongoing projects, or imbalances between demand and capacity” (Weick, 2009, p. 76). We now have access to a lot of information, and this may be a barrier in effectively assessing and using information. In some cases, this may interfere with our decision-making and work that must be done. Interruptions, attention issues, and limited time can also influence information overload, making it a greater problem. In 2019, the president of the American Organization for Nursing Leadership (AONL), M. Kingston, noted that “The use and promise of technology can also elicit anxiety and concern in many. Nurses in all settings report feeling overloaded with data and often find it difficult to prioritize the volume of incoming information. Without a clear plan and understanding of nursing workflow, implementation of new technology can certainly complicate care. Technology literacy may also be a challenge requiring an individualized approach to education and development” (AONL, 2019). We are attached to our devices personally and now more and more in healthcare delivery. Managing the use of devices and information is a critical requirement for success. Accessibility to information has a positive impact on quality care; however, we are learning that this can also have a negative impact, which may prevent us from reaching outcomes-for example, if we have too much information or we cannot manage the information effectively.
Nursing Standards: Scope and Standards of Nursing Informatics
Nursing informatics (NI) is the “specialty that integrates nursing science, computer science, and information science to manage and communicate data, information, knowledge, and wisdom in nursing practice” (HIMSS, 2023a). It supports consumers, patients, nurses, and other providers in their decision-making in all healthcare settings. This support is accomplished by using information structures, information processes, and HIT. The existence of the American Nursing Informatics Association (ANIA) indicates that this is now an important part of the nursing profession. Its mission is to “advance nursing informatics through education, research, and practice in all roles and settings” (ANIA, 2023).
Undergraduate nursing programs should include HIT in the curriculum, sometimes as a course on HIT, but content should be integrated throughout the curriculum so that students understand the implications in all areas of nursing practice. If this content and experience is not included in a nursing education program, this is a problem because with the greater emphasis on HIT as a competency and now the expanding area of digital health, all nurses need to be prepared and feel competent in using HIT in their practice. Some schools of nursing offer nursing informatics master's degrees, which offers more opportunities for nurses to specialize and then provide these services to HCOs.
Data alone are not useful, but rather understanding data and then using this knowledge are important. This view should be included in discussions with students. The steps in moving from data to wisdom can be described as data naming, collecting, and organizing, following this pattern: (1) information-organizing and interpreting; (2) knowledge-interpreting, integrating, and understanding; and (3) wisdom-understanding, applying, and applying with compassion. Figure 13-3 illustrates this process. Nelson and Joos defined “wisdom” as “the appropriate use of knowledge to manage and solve human problems. It is knowing when and how to apply knowledge to deal with complex problems or specific human needs” (1989, p. 6). Knowledge and wisdom are related: “Knowledge is built on a formalization of the relationships and interrelationships between data and information” (Nelson, 2018; Blum, 1989, p. 24). Data are important in the delivery of nursing care, but without effective data analysis, it is not useful to us. In HCOs, data can be used to evaluate outcomes, identify problems for a specific group of patients, and assist in making plans to improve care. In community/public health, aggregated data are often collected to better understand the health issues in a population or community and to formulate a plan of action.
Figure 13-3 From data to wisdom.
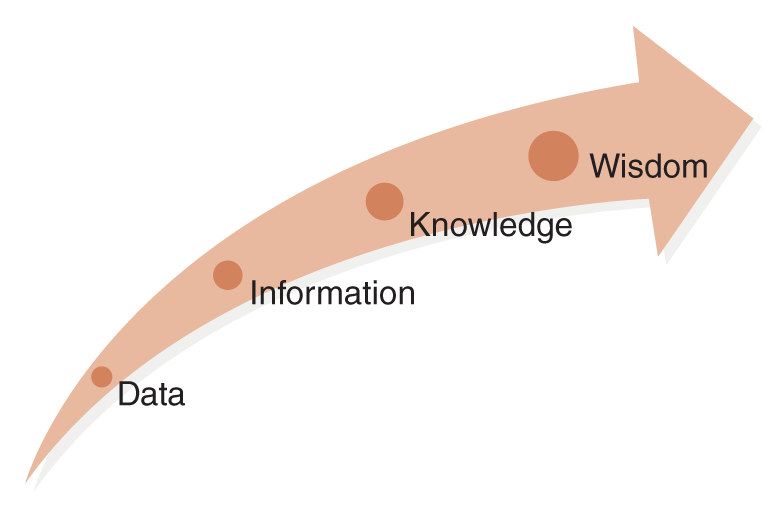
An arrow diagram illustrates the progression from data to wisdom. The arrow points upward, with labels along its length: data, information, knowledge, and wisdom. Each term is represented by progressively larger dots.
U.S. Department of Health and Human Services (HHS). The Office of National Coordinator for Health Information Technology (ONC). (2015). Federal Health IT Strategic Plan. 2015-2020, p. 13 https://www.healthit.gov/sites/default/files/9-5-federalhealthitstratplanfinal_0.pdf
Certification in Informatics Nursing
Nurses can be certified in IT/HIT if they meet the eligibility criteria and satisfactorily complete the certification examination. These are not simple eligibility criteria; they take time to meet. The following list identifies the criteria required to apply for the IT/HIT certification exam sponsored by the American Nurses Credentialing Center (ANCC, 2023):
- Hold a current, active registered nurse license in a state or territory of the United States or the professional, legally recognized equivalent in another country.
- Have practiced the equivalent of 2 years full-time as a registered nurse.
- Hold a bachelor's or higher degree in nursing or a baccalaureate degree in a relevant field.
- Have completed 30 hours of continuing education in informatics within the last 3 years.
- Meet one of the following practice hour requirements:
- The nurse must have practiced a minimum of 2,000 hours in IT nursing within the last 3 years.
- The nurse must have practiced a minimum of 1,000 hours in IT nursing in the last 3 years and must have completed a minimum of 12 semester hours of academic credit in informatics courses that are part of a graduate-level nursing informatics program.
- The nurse must have completed a graduate program in NI containing a minimum of 200 hours of faculty-supervised practicum in IT.
The HIT nurse is involved in activities that focus on the methods and technologies of information handling in nursing, such as the development, support, and evaluation of applications, tools, processes, and structures that help nurses manage data related to direct patient care as well as in nursing education and research. These nurses can be involved in a variety of information system functions, including theory formulation, design, development, marketing, selection, testing, implementation, training, maintenance, and evaluation. They may hold positions in HCOs, such as in clinical practice, management, quality improvement, research, or education and serve as HIT consultants. A nurse who wants to function in this specialty area must have excellent computer skills, understand practice needs for information, and know how best to apply HIT to nursing practice. This work requires effective collaboration in interprofessional teams and leadership. By advocating for the needs of the practicing nurse, the HIT nurse represents all nurses in practice-clinical, management, education, and research.
Informatics/Health Information Technology: Impact on Care
Effective use of HIT can lead to safe, quality care. HIT application, however, does not guarantee perfection. It is commonly thought that work processes will be better if using HIT; however, potential glitches need to be considered to assist in preventing problems. Examples include the following: clear expectations for staff HIT use and outcomes, HIT ease of use, staff time for HIT training, quality and accessibility of HIT training, staff time required to use HIT, monitoring of errors and methods used to address problems, accessibility to HIT, such as on a computer or device that supports the task, acceptance of HIT by staff, effective methods used to introduce HIT changes and communication of these changes, HIT tech support, and so on.
Introducing and maintaining HIT requires careful planning with input from staff that use HIT. Nurses need to assume an active role in the development of HIT for patient care and not wait to be asked to participate. When an HCO is choosing an electronic medical record (EMR) system, nurses need to be involved to ensure that the system meets nursing care documentation requirements and that relevant data can be collected to assist nurses in providing and improving care. Nurses may serve in key HIT roles to guide EMR development and implementation. Nurses may also serve as resources to ensure that the systems are nurse-user-friendly. Many nurses who provide feedback about systems do not have special HIT training. They review the system to determine if it is user-friendly for nurses who have limited informatics knowledge and help to determine if the system meets documentation needs and standards. All nurses need to be skilled in managing and communicating information, but most nurses are primarily concerned with the content of that information and accessing it when they need it.
In the work environment today, nurses routinely use technology, such as the EMR, barcoding for medication administration, patient monitoring devices, communicating with the team, and computerized provider order systems. Even nurse managers and administrators are using more electronic methods, such as the chief nursing officer (CNO) using an electronic tracking tool during management rounds and using this technology to provide peer-to-peer support for new managers (Lindgren, 2023; Meade & Gormley, 2018). This is an electronic web-based tool that supports a feedback loop and clear communication process between the CNO, nurse managers, and clinical nurses. The goal in using electronic methods during practice is to make work more efficient, impacting workflow and supporting quality care. Nurses' attitudes and perceptions of this situation are critical. Time spent on tasks has always been a nursing concern. One hospital conducted a quality improvement project to examine these issues (Higgins et al., 2017). Data collection methods included observation of nurses, nurses' self-report, and a patient survey. The data from the observations and the self-reports were different with nursing staff self-reports illustrating overestimation of time involved in direct care, wasted time activities, and charting. Self-reporting may not be an effective data collection method for this type of question as observation may be more accurate. Nurses' attitudes toward technology were found to be positive, but younger nurses were more positive about its use. In this project, patients were generally satisfied with the level of direct care they received.
In today's dynamic healthcare environment, coordination of care is very important. One of the barriers to seamless coordination and communication has been the lack of interoperable computerized records with hospitals and also office-based clinical practice (Bodenheimer, 2008). This has long been recognized as a national problem that is currently not yet fully solved. For example, it should be possible to share current information among healthcare providers in private practice, clinics, and hospitals when it is needed, but this is not possible. This requires not only effective technology but also greater use of standardized definitions related to data and measurement to ensure objectivity and reliability of data, allow for comparisons, consistently track data over time, and increase opportunity to provide/observe empirical evidence of outcomes (Glassman & Rosenfeld, 2015). The issue of shared information became very important during the COVID-19 pandemic due to the need to track testing, illness, and vaccination. The United States has no national database to collect this information and even few states have electronic documentation of such data, whereas some countries do collect this data, such as Israel-a country with a universal healthcare system and a computerized system that supports sharing across providers with all citizens using a lifetime identification number.
Innovative methods to improve coordination that focus on informatics have been developed. One method is to use electronic referral (e-referral). This approach allows a healthcare provider to send an email to another provider, such as a medical specialist, with information about the patient and ask for consultation. In some situations, this communication eliminates the need to see the patient. The specialist reviews information, such as lab reports, surgical reports, and so on, and the specialist can share opinions and treatment recommendations with another healthcare provider. It is critical that reimbursement is available for this type of service, or it will not be used. Health Insurance Portability and Accountability Act of 1996 (HIPAA) requirements must also be considered, with all parties working together to ensure patient privacy. Timely information flow from the hospital to posthospital care should improve patient coordination. Not having this communication option is a major drawback; even though the technology to improve is available, it is not used as much as it should be.
Implications for Nursing Education and Nursing Research
IT is important not only for practice but also in nursing education and research. Today, there is greater use of IT in nursing education than was the case in the past. The increased use of e-learning throughout the nursing curriculum, at both the undergraduate and graduate levels, has revolutionized nursing education, and the COVID-19 pandemic expanded its use. These changes have led to the need for faculty to consider the use of more interactive learning methods. Moreover, as students use more technology in their personal lives, they expect correspondingly greater use of IT in education. Such tools as tablets, smartphones, and internet tools and apps, methods that provide instant information and can be very interactive. These methods can also be used to increase student-faculty communication and have the potential to provide different means of student-faculty supervision in the clinical area. This is particularly true in areas such as public/community health when students visit multiple sites and faculty move from site to site to spend time with students. Informatics also affects simulation experiences for students, allowing faculty to create complex learning scenarios that use the computer and computerized equipment, for example, to provide an opportunity for students to use an EMR system in a simulated environment before using an EMR in a clinical setting.
Today, there is a greater opportunity to collect data due to HIT and improve care as a result of this opportunity (Classen et al., 2018). Nursing research uses informatics in data collection and analysis; it saves time and improves the quality of data collection and analysis. Researchers have greater access to tools that can make their work easier and organize and save data for later use. It is then easier to analyze data to determine research results. Nurse researchers and their staff do some of this work, and specialists, such as statisticians may assist. There is also much more data available for research that can be collected from the many healthcare data technology methods, such as the medical record. As noted earlier as important, HCOs and healthcare providers need to consider the importance of data science, “the systematic study of the organization and use of digital data in order to accelerate discovery, improve critical decision-making processes and enable a data-derived economy” (Ahalt et al., 2014, as quoted in Nelson-Brantley et al., 2019, p. 176).
| Stop and Consider 3 |
|---|
| Health informatics is now integrated in practice, management, quality improvement, education, and research. |
Documentation
Clinical documentation has a major impact on patient care and patient outcomes, providing critical information in a timely manner for healthcare providers and serving as a source of clinical data for clinical research and education. Documentation is expected to be accurate and accessible to those who need access but must apply confidentiality and privacy law requirements. Many different staff document in the medical record, and it is important that nurses describe nursing practice. Both nurse managers and nurses involved in direct care are accountable for ensuring that documentation meets expected standards. Nurse educators in academic and HCO settings are also involved in ensuring effective documentation. Documentation meets many needs, such as clear communication for the team and others who need the information to provide care and meets legal and ethical, accreditation, documentation, reimbursement, and budget requirements.
The format and content of nursing documentation have changed as changes have occurred in knowledge and healthcare services. It is a professional responsibility to document planning, actual care provided, and outcomes. Care coordination and continuity are supported by documentation. With many different staff caring for patients around the clock and use of interprofessional teams, it is critical that a clear communication mechanism exists, and the key mechanism is documentation. Verbal communication is important, but a written document is critical. Staff can refer to such documentation when other care providers are not available. Through documentation, outcomes and evaluation of patient care are made clear.
The medical record is also a legal document, and as such, rules must be followed when creating and amending it. Once care has been documented, changes to documentation must be accompanied by a note indicating who made the change(s) and when (date and time), following HCO policy and procedure. Only certain staff may document; they must note the date and time in the documentation and include their name and credentials. If there are questions about care or a legal action, such as a malpractice suit, the medical record is the most important source of evidence. Consequently, medical records must be saved. A nurse can say certain care was provided, but if it is not documented, then it is as if that care did not occur.
The following describes the advantages of using electronic documentation (HealthIT.gov, 2023).
Our world has been radically transformed by digital technology-smart phones, tablets, and web-enabled devices have transformed our daily lives and the way we communicate. Health care is an information-rich enterprise. A greater and more seamless flow of information within a digital health care infrastructure, created by electronic health records (EHRs), encompasses and leverages digital progress and can transform the way care is delivered and compensated. With electronic records, information is available whenever and wherever it is needed for (HHS, HealthIT.gov, 2023):
- Providing accurate, up-to-date, and complete information about patients at the point of care
- Enabling quick access to patient records for more coordinated, efficient care
- Securely sharing electronic information with patients and other clinicians
- Helping providers more effectively diagnose patients, reduce medical errors, and provide safer care
- Improving patient and provider interaction and communication, as well as health care convenience
- Enabling safer, more reliable prescribing
- Helping promote legible, complete documentation and accurate, streamlined coding and billing
- Enhancing privacy and security of patient data
- Helping providers improve productivity and work-life balance
- Enabling providers to improve efficiency and meet their business goals
- Reducing costs through decreased paperwork, improved safety, reduced duplication of testing, and improved health.
The following summary of documentation guidelines is still relevant today. Some apply to written records and some to both written and electronic (Iyer & Camp, 1999):
- Do not include opinion but only objective information in documentation. The nurse does not make subjective comments (for example, comments about the patient being uncooperative, lazy, or impolite). Nurses document only what they have done and objective data. A nurse does not document another staff member's actions. Supervision of care, however, can be documented.
- Write neatly and legibly for any handwritten documents. For an electronic system, typos (typographical errors) may be a problem. Other issues may arise in electronic systems that use a checklist for a particular section of the EMR but do not allow for narrative notes. Nurses and others may be frustrated when they cannot add a narrative note.
- Use of copy and paste feature in an EMR/EHR increases risk of errors, particularly perpetuating an error, as this is often done with insufficient thought or can be put in the wrong place in the record.
- Use correct spelling, grammar, and medical terminology.
- Use authorized abbreviations. Using unapproved abbreviations increases the risk of errors. For example, The Joint Commission (2023b) identifies abbreviations that should not be used, and their accredited HCOs notify their staff not to use these abbreviations.
- Use graphic records to record specified patient data, such as vital signs and medication administration.
- Record the patient's name on every page (for hard-copy medical records); this should be part of the EMR.
- Follow HCO policies and procedures about verbal and telephone orders.
- Transcribe orders carefully as per written orders; double-check and ask questions if an order is not clear. In electronic systems, orders do not need to be transcribed; however, this does not mean that there is no risk of an error. All orders need careful review, and if they are not clear, they may require follow-up.
- Document omitted care.
- Document medications and outcomes.
- Document patient noncompliance/nonadherence and the reason(s) for it.
- Document allergies and use this information to prevent errors and complications.
- Document sites of injections and other procedures.
- Record all required information about intravenous therapy and blood administration.
- Report abnormal laboratory results.
- Document as soon as possible after care is delivered. If documentation is done late, note this in the record. The nurse should not leave blank areas to come back to for later documentation.
- When quoting, use quotation marks and note the person who made the statement, date, and time.
- When documentation is corrected because of a mistake, follow the HCO policies regarding corrections as per a hard-copy record or electronic record. Medical records are never rewritten or destroyed by staff.
- Document patient status change.
- When contacting the physician, document the time, date, name of the physician, reason for the call, content, physician response, and steps taken after the call. This note should not include a subjective analysis of the response, such as the physician's attitude.
Another documentation consideration today is the recognition of diversity, equity, and inclusion (DEI). “Nurses play a prominent role in building equitable healthcare systems that address diversity and inclusion. Collecting information about race, ethnicity, sexual orientation, and gender identity can help organizations and nurses improve care and outcomes. From an organizational perspective, accurate patient data aid inclusive service design, provide insight into areas that require additional services, and inform strategic hiring. From a nursing perspective, awareness about a patient's race, ethnicity, sexual orientation, and gender identity helps to ensure individualized care tailored to a patient's unique needs and determine appropriate available services” (Park, 2022). This type of information should be integrated as needed with consideration of DEI. Nurses need to be sensitive when asking questions and documenting responses related to race, ethnicity, sexual orientation, and gender identity, demonstrating a nonjudgmental attitude. This information is important to individual patient care, ensuring patient/person-centered care, and important information for healthcare providers and organizations as they plan, implement, and evaluate services.
The Joint Commission (2023a) does not provide details as to what must be included in a medical record, but in general, documentation should include relevant information about the patient's needs and care and be accessible to staff, though the format is prescribed. It is important for HCOs to have clear documentation policies and procedures and ensure that staff are aware of them and follow them. When changes occur, staff must be informed so that new requirements will be met.
| Stop and Consider 4 |
|---|
| Documentation is a critical communication method for the care team. |
Meaningful Use
“Beginning in 2011, Promoting Interoperability (formerly the Medicare and Medicaid EHR Incentive Programs) was developed to encourage eligible professionals (EPs) and eligible hospitals and critical access hospitals (CAHs) to adopt, implement, upgrade (AIU), and demonstrate meaningful use of certified electronic health record technology (CEHRT)” (HHS, CMS, 2022). The meaningful use initiative is even more important now due to changes in IT that focus on the following objectives and associated measures, all of which promote interoperability, to better ensure the exchange and use of information:
- Electronic prescribing
- Health information exchange
- Provider-to-patient exchange
- Public health and clinical data exchange
Meaningful use is concerned with the use of certified EHR technology to improve communication and care and ensure effective processes and efficiency along with care coordination. It identifies specific objectives that eligible professionals and hospitals must achieve to qualify for CMS reimbursement. Given that most hospitals receive CMS reimbursement, most hospitals must meet these requirements. This provides a strong incentive to make changes so that reimbursement can be received. When decisions about HIT are made, meaningful use must be considered. Nurses should be involved in these changes, particularly if they are in leadership positions. Ultimately, it is hoped that meaningful use compliance will result in the following benefits, and this list demonstrates that it applies to healthcare practice, education, and research:
- Better clinical outcomes
- Improved population health outcomes
- Increased transparency and efficiency
- Empowered individuals
- More effective research data on health systems
All the purposes for meaningful use are in line with the Quality Chasm reports on quality and are associated with continuous quality improvement (CQI).
| Stop and Consider 5 |
|---|
| Meaningful use is associated with nursing practice. |
Standardized Terminology
Health care has expanded in multiple directions and includes services from many different healthcare providers. Ensuring effective communication among many types of healthcare providers is not always easy. Certainly, there are issues regarding willingness to communicate, lack of time to communicate, and so on, but a critical problem is the lack of a common professional language/terminology. For those entering a healthcare profession, such as nursing students, this is probably a surprising comment. There are some common medical and healthcare terms, but each profession has some specific terminology that is often not known or understood by other healthcare professionals. “Creating a common language is no small task. Developing and adhering to distinct profession-specific terms may be a manifestation of professionals' desire to preserve identity, status or control” (IOM, 2003, p. 123). This problem affects all the core healthcare profession competencies and the ability to develop educational experiences that meet the competencies across healthcare professions, such as nursing, medicine, pharmacy, and allied health and support more effective interprofessional teamwork. The issue of shared terminology is even more important in HIT because it is dependent on language, requiring a shared terminology. A standardized terminology is a collection of terms with definitions for use in information systems, databases. This enables comparisons, for example, the same term is used to denote the same condition, and it is also necessary for effective documentation in EMRs/EHRs. Healthcare professionals need to be willing to actively work together to achieve greater acceptance of terminology. This will require compromises and has yet to be fully accomplished. The ANA position statement on EHRs noted that it supports “the use of recognized terminologies supporting nursing practice as valuable representations of nursing practice and to promote the integration of those terminologies into information technology solutions. Standardized terminologies have become a significant vehicle for facilitating interoperability between different concepts, nomenclatures, and information system” (ANA, 2015). These statements are examples of why developing and accepting a universal language is difficult but necessary, but they also illustrate how it is easy to approach this issue from silos-focused on individual healthcare professions. These statements are nursing focused, but all healthcare professions need to address this issue using interprofessional collaboration.
Determining how best to move from a specific profession approach to a collaborative approach to solve this problem is a challenge. The National Library of Medicine (NLM), serving as the coordinating body for clinical terminology standards within HHS, offers products and services for HCOs and healthcare professionals that support interoperability and the unambiguous exchange of health data (NIH, NLM, 2019). The Healthcare Information and Management Systems Society (HIMSS) has developed standards to better ensure effective communication-“the ability to represent concepts in an unambiguous manner between a sender and receiver of information. Most communication between health information systems relies on structured vocabularies, terminologies, code sets and classification systems to represent health concepts. Standard terminology provides a foundation for interoperability by improving the effectiveness of information exchange. Using standard terminology should be a simple and logical step in health IT. However, with the complexities of many diagnoses systems, clinical narrative transferred via PDF format, various coding systems, and the cost of digitizing volumes of reference material/dictionaries, it is not as easy to accomplish” (HIMSS, 2023b).
| Stop and Consider 6 |
|---|
| Standardized terminologies are needed for effective healthcare professional communication. |
Systems and Terminologies
IT includes more than consideration of email and the internet. IT in general and HIT include many database systems, equipment, terms, and other factors that make this a complex area. The following provides examples illustrating the complexity of HIT.
Systematic Collection of Nursing Care Data or Data Element Sets
- Nursing Minimum Data Set: This clinical data set describes patient problems across healthcare settings, different populations, geographic areas, and time. It provides clinical data to assist in identifying nursing diagnoses, nursing interventions, and nursing-sensitive patient outcomes. In addition, the Nursing Minimum Data Set is useful in assessing resources used in the provision of nursing care. The goal is to link data between HCOs and providers. Data can also be used for research and healthcare policy.
- Nursing Management Minimum Data Set: This management data set focuses on nursing administrative data elements in all types of settings.
Interface Terminologies
- Clinical Care Classification: The clinical classifications software for the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM), is a diagnosis and procedure categorization scheme that can be used in many types of projects to analyze data on diagnoses and procedures. The software is based on ICD-10-CM, a uniform and standardized coding system. ICD-10-CM includes more than 14,000 diagnosis and procedure codes (HHS, CDC, NCHS, 2021).
- Nursing Intervention Classification and Nursing Outcome Classification: The North American Nursing Diagnosis Association (NANDA) focuses on nursing diagnoses, Nursing Intervention Classification (NIC) on nursing interventions, and Nursing Outcome Classification (NOC) on nursing outcomes (NANDA, 2023).
- Omaha System: The Omaha System is a comprehensive, standardized taxonomy designed to improve practice, documentation, and information management. It includes three components: the problem classification scheme, the intervention scheme, and the problem rating scale for outcomes. When the three components are used together, the Omaha System offers a way to link clinical data to demographic, financial, administrative, and staffing data (Omaha System, 2023). The system is used in nursing home health care and community/public health services.
- PNDS: The PNDS is a standardized nursing vocabulary that addresses the perioperative patient experience from preadmission until discharge, including nursing diagnoses, interventions, and outcomes. This set was developed by a specialty organization, the Association of periOperative Registered Nurses, and recognized by the ANA as a data set useful for perioperative nursing practice. This standardized system is now called Syntegrity PNDS (AORN, 2023). It is a HIT tool that can be personalized by HCOs to meet individual organizational needs. The framework supports electronic documentation, patient quality and EBP, a common language/terminology, and a method to collect and compare data, connecting nursing diagnoses, care implementation, and assessment to measure outcomes.
Examples of Multiprofessional Terminologies
- Current Procedural Terminology CT: This code is used for reimbursement (AMA, 2023).
- Systematized Nomenclature of Medicine-Clinical Terms SNOMED CT: This comprehensive clinical terminology is one of several standards approved for use in U.S. federal government systems for the electronic exchange of clinical health information (NIH, NLM, 2019). The system is applicable to nursing and other healthcare services and focuses on diagnoses, interventions, and outcomes.
With the increased use of technology for documentation, nursing continues to be more concerned about two issues (Schwiran & Thede, 2011):
- How to differentiate nursing's contributions to patient care from those of medicine
- How to incorporate descriptions of nursing care into the health record in a manner that is commensurate with its importance to patients' welfare
This requires systems that can meet these needs; therefore, nurses need to engage in HIT so that nursing can be better represented in decisions about EMRs. In an earlier study conducted by Schwiran and Thede (2011), the researchers examined nursing knowledge of and experience with standardized nursing technologies. The results indicated that most nurses did not have much knowledge of or experience with standardized nursing systems, such as the NIC, NOC, and NANDA. The nurses may have used them in their nursing education but not in practice after graduation. Given the increasing use of IT in healthcare settings, a lack of knowledge and experience may hamper nurses' ability to participate actively in HIT development and evaluation. “The use of standardized nursing terminologies and classification systems are a way that nursing documentation can be leveraged to generate evidence related to nursing practice. Several widely reported nursing specific terminologies and classifications systems currently exist including the Clinical Care Classification System, International Classification for Nursing Practice®, Nursing Intervention Classification, Nursing Outcome Classification, Omaha System, Perioperative Nursing Data Set and NANDA International. However, the influence of these systems on demonstrating the value of nursing and the professions' impact on quality, safety and patient outcomes in published research is relatively unknown” (Studwick & Hardiker, 2016, p. 215). We have developed systems, but the review of studies, such as the Studwick and Hardiker study, indicated the use of these systems to generate new knowledge and validate nursing practice was not yet at the level it should be. NANDA International is an important resource now, and its purpose is the “implementation of nursing diagnosis [that] enhances every aspect of nursing practice, from garnering professional respect to assuring consistent documentation representing nurses' professional clinical judgment, and accurate documentation to enable reimbursement. NANDA International exists to develop, refine and promote terminology that accurately reflects nurses' clinical judgments” and its current mission is found at the NANDA website (NANDA, 2021).
| Stop and Consider 7 |
|---|
| Nursing is involved in the development and improvement of health information technology. |
Informatics Health Information Technology: Types and Methods
For HIT to be effective, three concerns must be addressed. First, the HCO must have effective and accessible IT support services. Staff must be able to easily request and get this support. Failure of the information system has major implications for patient care and increases staff stress, so backup systems are critical. There are also financial implications because HIT data are also used to support reimbursement and maintain the budget. The second critical concern is staff training. This requires resources: financial resources, time, and trainers. Time is needed for staff to attend training, and there must be recognition that it takes time for staff to learn how to use a system and apply what they have learned. It is also important to recognize that during training and when changes are made, there is an impact on care and work processes. Incorporating HIT with any of the methods described here (and others that are not included here) requires changes in care delivery. The third concern notes that change is stressful for staff and for management, and it needs to be planned. Trying to implement too many changes at one time may increase this stress, affect the success of using more HIT in the future, decrease staff motivation to participate, and increase the risk of errors that might affect patient outcomes. Change is discussed in several chapters in this text.
It is not difficult to find nurses who will complain about a hospital's attempt to increase the use of HIT, particularly if it was badly planned. Often, in these complaints, staff members note that the system selected was not effective, and they had no part in the decision and implementation process. Equipment and software are very costly, and decisions about them are critical. Implementation of an ineffective system only increases costs, management and staff time, and stress. To avoid these problems, time must be taken to carefully evaluate equipment and software to make sure they meet the needs and demands of the HCO and users such as nurses. Examples of current HIT methods that require careful assessment and staff training are automated dispensing of medications and barcoding; computerized monitoring of adverse events; EMRs/EHRs, provider order-entry systems, clinical decision support systems, use of devices, such as tablets and smartphones, and computer-based reminder systems; access to patient records at the point of care; prescribing via the internet; use of nurse call systems, voice mail, telephone for advice, and other similar services; use of internet or virtual appointments; and online support groups for patients and families. These methods are discussed in this section.
It is important to note that there is now a new serious security risk with the use of electronic methods for documentation and communication. Hacking has become more common with HIT in general, and there have been incidents of hacking health records. In March 2020 during the COVID-19 pandemic, 400 U.S. hospitals experienced a ransomware attack, and other countries also experienced these attacks (Wolf, 2020). Ransomware is a type of hacking where an external source uses encryption (scrambling data into a secret code) to gain control over a data system (Fox, 2023; Neprash et al., 2022; McAfee, 2021). During the pandemic, this added to the stress that health systems experienced due to overload on all fronts-for example, two healthcare systems were hacked in early 2021, and information was shared on the internet (Collier, 2021). Why would this be done? One reason is health records often include personal identification information that might be used for illegal purposes, such as to obtain addresses, telephone numbers, email addresses, credit card information, and Social Security numbers (Peterson, 2015; McCain, 2014; Pagliery, 2014). Another experience that some HCOs have had is a hacker got access or control of the HCO's data system and then the hacker(s) demanded a ransom or money for the HCO to regain access to the system (Conn, 2014). This can happen to small or large HCOs. All of this emphasizes that the data we have are important-valuable-not only to us and to our patients but also to others who may not have the same goals. We must be careful and use appropriate passwords and procedures to protect data and report any changes that do not make sense in the organization's IT system. There is also increased use of emails as a method to communicate with patients-sharing important personal information. Is this wise? Patients are often asked and encouraged to provide their email-but it is their choice to make, and in all cases, it should be their decision. We need to take care with what we put in emails or what we ask patients to send in an email-for example, personal addresses, social security numbers, credit card numbers, and insurance identifiers should never be sent in an email. When we keep data for healthcare purposes, we have ethical and legal responsibilities to ensure that information is accurate and secure.
Automated Dispensing of Medications and Barcoding
Pharmacies in all types of HCOs are using or moving toward expanding the use of automatic medication dispensing systems with barcoding. These systems select the medication based on the order and prepare it in single doses for the patient. The barcode is on the packaged dose. To ensure the correct match between an order and a patient, this code can be compared with the barcode on the patient's identification band and the medication using a handheld device. This type of system can decrease errors, and it supports all five rights of medication administration, as discussed in other content in this text. Barcoding can also be used to collect data about prescribed and administered drugs. Data may then be used for monitoring QI and for research. Barcoding systems are expensive to install and maintain, but they can make a difference in reducing errors and time required for all medication administration steps and are now common in use.
Computerized Monitoring of Adverse Events
Computerized systems that monitor adverse events assist in identifying and monitoring adverse events. Developing and using a database of these events facilitates the analysis of data and the development of interventions to decrease adverse events. A major problem with data collection, such as collecting data about adverse events, is not using structured collection and possibly overdoing collection, and then ending up with data that are not needed or not in a format that could be easily used. Careful planning is required to identify information or data needed and determine how it will be accessed and effectively used. Technology and HIT can be used but require research to determine the best use; for example, a study examined the use of remote patient monitoring to reduce falls and patient harm (Zimbro et al., 2023). Using electronic medical record data from 13 hospital integrated healthcare systems the study concluded that this monitoring reduced harm and improved patient care.
Electronic Medical/Health Records
EMRs/EHRs are replacing the written medical record for an individual patient when the patient receives care within a specific healthcare system. A second type of electronic documentation system is the personal health record (PHR). The PHR is less common than the EMR, but it is hoped its use will become standard in the future. The PHR is a computer-based health record used to collect data over the long term-for a lifetime. With the patient's permission, the healthcare provider can access this record and easily obtain information. To reach this point, there must be agreement on a minimum data set-uniform definitions of data (that is, standardized language/terminology) to enable all healthcare providers to input data consistently and understand and use the information. There is still much to be done to make this a reality in every HCO, including clinics and medical offices. We have the technology to do this but need to implement it.
The EMR/EHR is a record of the patient's history and assessment, orders, laboratory results, description of medical tests and procedures, documentation of care provided and outcomes, and patient identifier information, such as birth date, age, gender, race, and so on. Other information commonly included is allergies, smoking status, immunizations, medical history, and more. Current requirements for electronic records, referred to as the Common Clinical Data Set, guide EMR content. Care plans are also included in the EMR. It should be easy to input, search, and review the plan information and possibly print reports.
Electronic data can be stored over the long term, which is harder to do with written records as this requires significant storage space and may not be easy to find once archived. In addition, written records may be less readable over time. The hard-copy record is not always easy to access when it is needed in a hospital unit. If one person is using the record, others cannot use it at the same time. With the EMR, if staff can access the computerized record system, then there is less of an access problem. EMR systems require security and backup systems to ensure that data are not lost in the event of a power outage, natural disaster, or other event (such as ransomware attacks mentioned earlier in this chapter) that may then make access difficult.
Electronic documentation has many advantages, such as providing a record of the timeliness of care and impacts on quality care (HIMSS, 2022). Staff can document as care is provided or soon after, providing a system for all members of the team to view the care process when needed. Documentation may take place in the unit workstation, a hallway computer station, the bedside in the hospital, or a clinic examining room. Bedside systems are better because they are easy to access when the nurse or other healthcare professional needs information, enhancing point-of-care documentation and timely input of information. This all improves documentation and communication. Other advantages are greater legibility; easier access to records for multiple users; increase in efficiency and effectiveness in the work environment; less opportunity to change records inappropriately; inclusion of safety elements, such as automatic alerts for allergies or incompatible drug orders and reminders to do certain tasks or add certain information to the record; ability to print records when needed; and more accurate and accessible data for reimbursement, budget, and quality improvement.
It is important to recognize that when HCOs change to electronic documentation or make changes in a current electronic system, this may be a time of disruption in clinical practice and workflow processes, especially if there are negative staff responses to the change process and/or the change itself (Ford et al., 2016). A study conducted by Barnett and colleagues (2016) also referred to disruption in work processes during transition to electronic records, particularly noting the negative impact on patient outcomes. In this study of 17 hospitals transitioning to electronic methods, the hospitals experienced more problems with adverse patient outcomes than hospitals that were not transitioning to electronic records. All of this affects the culture of safety and increases the risk for errors. HCOs and their providers must have time to adjust to change and recognize the benefits and, during change, be alert to prevent errors. This concern also applies to the experience of making changes in an existing electronic system.
Clinical Provider Order-Entry System
A clinical provider order-entry system (CPOES) may be included in an EMR, although it may also be a stand-alone system. The healthcare provider inputs orders into this system rather than using a hard-copy record. This is an expensive system to implement. One clear advantage of the CPOES is legibility, as handwritten orders are often very difficult to read because handwriting varies, and this may cause errors. It also takes time to transcribe written physician/provider orders into a form in which the orders can be applied. During this process, the risk of transcription errors increases. Typing orders into a computer can lead to typos, but this is less of a problem than errors with handwritten orders. A systematic review of 34 studies on CPOES identified key areas of the EMR and its CPOES that may be associated with CPOES errors: computer screen display, drop-down menus and auto-population, wording, default settings, nonintuitive or inflexible ordering, repeat prescriptions and automated processes, users' work processes, and CDSS (Brown et al., 2017). The studies reviewed identified examples of EMR and its CPOES weaknesses-such as use of an incomplete medication list that led to prescription error, misinterpretation of text, and lack of flexibility in the CPOES causing use of a workaround (bypassing a problem)-increasing the risk of an error. Drop-down menus need to include safeguards to prevent selection errors. Another study examined alerts of automated identification of antibiotic overdoses and adverse drug events via a CPOES (Kirkendall et al., 2016). This study highlighted alert fatigue, which is discussed in this text. If providers get several alerts, there is an increased chance that they will override the alert because of too many alerts-viewing them as irritants to getting work done or may even ignore an alert. These systems need to be carefully reviewed and revised to reduce alerts that are not critical or are inaccurate. Clinical decision support systems can be included with the CPOES. Brown and colleagues' systematic review concluded that the development of better CDSS might reduce errors and improve workflow (2017).
CPOES is not only a clinical tool to assist in providing effective care, but it also offers a source of data that may be used by the QI program. For example, an analysis of provider voiding of medication orders provides critical information about reasons orders are voided after they were written, or in some cases, the system may void the orders at the time they were put into the system (Kannampallil et al., 2017). This study examined 6 years of CPOES data, looking at voided and unvoided orders and reasons for the voiding. In the sample, 0.49% of all orders were voided, with most voided due to medication ordering errors. The use of voiding provides the HCO with an easy method for self-reporting near-miss medication ordering errors. The data should be used to assess the status of medication order errors within the HCO and develop strategies to reduce the need for voiding orders.
Clinical Decision Support Systems
Clinical decision support systems (CDSS) have led to major changes in healthcare delivery. These systems provide immediate information that can influence clinical decisions (HHS, AHRQ, 2019). Some of the systems intervene when an error is about to be made. For example, when an order for a medication is put in a patient's EMR, the CDSS might indicate the patient is allergic to that medication by immediately sending an alert and stopping the order. The nurse can also get alerts for a variety of potential problems, such as patients at risk for falls or decubiti.
In the past, nurses depended on textbooks or journals available in the unit or hospital library to find information, and such searches for information were often not done effectively. Easy electronic access to current information eliminates many problems related to obtaining information when needed. This, too, can improve the quality of care. EBP relies heavily on access to EBP literature, which is most easily accessible via the internet and EBP databases. As is true for all electronic methods, healthcare professional critical thinking, as well as clinical reasoning and judgment, must still be applied. Errors can still be made with technology.
More research is needed to fully understand the impact of CDSS on patient outcomes. Romano and Stafford's (2011) study indicated that there was no consistent association between such systems and the quality of care in a study that included 3 billion patient visits. Only one of 20 indicators-diet counseling for high-risk adults-demonstrated significantly better performance when CDSS were utilized. In contrast, earlier studies indicated that use of the CDSS improved outcomes. This study questioned whether results were influenced by the following factors: (1) CDSS rules may have been different in the systems studied; (2) the study focused on medication management, whereas earlier studies were broader; and (3) the study looked at the outcome of a single visit rather than the cumulative effect. More research is needed to understand the use of this method and better determine the effectiveness of using CDSS, which is a complex research area. When HIT is used, staff may go on “automatic pilot,” assuming the electronic system will catch all potential errors, which is not always the case.
Tablets and Smartphones
Tablet computers are very popular with the public and in the workplace. Smartphones offer internet capability and options for information storage. These phones give users quick access to information, the internet, email, text messaging, and, of course, telephone service. These handheld devices can hold a significant amount of information, serve as a calendar, keep contact information, monitor tasks, and so on. They are primarily an effective method for the transmission of information and can easily be used by nurses in practice.
Nurses who use tablets and/or smartphones carry information with them and can search for information about medication side effects or any other type of medical information necessary as they provide care. In some cases, with special access privileges, the nurse can access EMRs to get to patient information through a tablet or a device that can access this information. Many textbooks can now be uploaded onto tablets and smartphones, such as pharmacology and clinical laboratory resources, and even this text. This provides useful information for the nurse-accessible in seconds at the point of care. Nurses working outside a structured setting, such as in public/community health or in home health care, may also find this type of system useful to access support information and for documentation needs (patient information, visit data, and so on); however, they must be very careful to maintain HIPAA regulations. Electronic devices are used in public/community health to collect data such as health assessments. For example, data are stored locally on the tablet and then uploaded to a secure cloud server for the home healthcare agency (that is, a server that is encrypted to protect personal health information) when the user is back in network/wireless range. Anytime such technology is used, the data must be protected to keep information secure and confidential. There is not only the concern about information security but also the devices that can be lost or stolen. To prevent access if a device is missing, security codes should be used. HCOs should have clear policies and procedures related to actions staff should take if a device is lost or a person(s) who should not have access to the information gains access to the device. When these devices are used for oral communication in any location, healthcare providers must be careful to ensure privacy.
Computer-Based Reminder Systems
Computer-based reminder systems are used to communicate with patients via email or text messages to remind them of appointments and screenings and discuss other health issues. In the future, these methods will most likely take the place of telephone calls to remind patients of appointments. Any reminder system must also maintain HIPAA regulations. For example, the healthcare provider must ensure that only authorized parties have access to the computer and email data. Only the patient should have access to the information unless the patient wants the information shared. An example of concern about privacy is using a patient's work email or work mobile phone. Employers have the right to view employee emails and phones, and thus, if the employer views employee information and devices, private health information may be shared.
Access to Patient Records at the Point of Care
Many hospitals are moving toward providing access to patient records either in the patient's room or in the hallway via computers and, in the case of ambulatory care, in areas where patient-provider services are provided. In the future, more nurses will carry small electronic devices that allow access to the EMR when needed for work requirements. This reduces time spent returning to the workstation to get information and allows for more timely documentation, which can be completed as soon as care is provided. This reduces errors and improves quality because information is readily available to assist in decision-making and providers will know when care has been provided in a timely manner. Point-of-care access decreases the chance that details may be forgotten, documented incorrectly, or not documented at all. In addition, it saves nurses time and eliminates the need to delay documentation. For example, if they do not have this type of immediate access, nurses may document at certain times during the shift, such as midmorning or near the end of a shift, requiring them to find a block of time to complete documentation without interruptions. This is an approach that can lead to errors, incomplete data in the record if the nurse forgets information, and situations in which other providers need current patient information that has not yet been documented.
Internet Prescriptions
There has been rapid growth in consumer access to prescribed medications via the internet often referred to as ePrescribing. The medications are then mailed to the patient. The consumer must be careful and check the legitimacy of the source to prevent errors. In addition, consumers may reorder medications on the internet and then pick them up at the pharmacy or have them delivered.
Nurse Call Systems
Nurse call systems are a form of informatics that is very important to daily communication within a healthcare system. They allow for improved and efficient communication and eliminate the old method of yelling out for a staff member or a unit speaker system calling for staff. Many types of nurse call systems exist, such as pagers, light signals, buzzers, methods that allow patients to talk directly to nurses through an easily accessible direct audio system, smartphones, miniature lapel microphones, and locator badges. The goal is to get a message to the right person as soon as possible while maintaining privacy and confidentiality. Doing so can improve care-improve communication and patient satisfaction, reduce errors, and increase efficiency, thus preventing the unnecessary work of trying to obtain and share information.
Voice Mail and Texting
Computer-based messaging systems are found in all healthcare settings today so that staff and others can leave and receive voice and text messages; for example, staff and patients can use these systems, often reducing the need for callbacks. However, complicated systems may annoy consumers, and this form of communication has an impersonal quality, though it is part of everyday life today. Staff must be careful about leaving voice messages and even text messages to ensure HIPAA requirements are met.
Telephone for Advice and Other Services
Mostly, insurers use patient advice systems, although some HCOs and providers provide these services as well. In such systems, staff members determine the caller's problem or questions and provide advice. Typically, insurers develop standard protocols or clinical pathways that nurses use to respond to common questions, but nurses must still use professional judgment when providing advice. This type of service should not become “cookbook” care in which there is no consideration of assessment and individual patient needs. Assessment is the key to successful telephone nursing because it enables providers to identify the caller's problems and consider needed interventions that may or may not be found in the guidelines. Some physician offices have telephone advice services that are manned by a physician in the practice or by a nurse. Pediatric practices are a common type of practice using this system. Patient telephone advice systems require clear documentation policies and guidelines that include content related to who called, when, and for what reason; the required assessment data; possible problem(s); and recommended interventions-as well as any follow-up action, such as a return call by the service to check on the patient. Telephone advice systems are typically used to answer questions, remind patients of appointments, and check in on how a patient is doing. The COVID-19 pandemic increased the use of these systems to reduce the need for patients coming into a care setting and, thus, reducing the risk of exposure to the virus.
Many hospitals now use the telephone to begin the admission process for patients with scheduled admissions, procedures, and testing. Patients are called before the scheduled date, asked questions related to required information, and told what to expect and any required preparation. Pretesting may also be scheduled prior to hospital admission. This saves the hospital time, is more cost-effective, and may be more convenient for the patient. This method can also identify problems that may affect patient care so that they can be addressed early on.
Internet or Virtual Appointments
The internet may be used as a means for increasing accessibility to physicians, advanced practice registered nurses, and other healthcare professionals or for making appointments-digital health. The internet is used today to obtain advice from health professionals and, as noted previously, for telephone advice; use of this method increased with the COVID-19 pandemic. Portable family histories can be maintained in this fashion and passed on to a new primary care provider. Patients and families who have limited resources-financial, transportation, or insurance-can more easily receive medical advice in this format if they have internet access. It also keeps some patients from missing work or the need to take a child or other family member to an appointment. Some virtual methods allow the patient and the healthcare provider to see each other, which may provide more effective communication between the patient and provider. Many of these sites link to cellular devices to send an alert of high importance to whoever is on call for virtual patient hours. These types of services have increased, providing quick connections with health professionals to get answers to questions, provide patient monitoring data, and/or make decisions about next steps such as an appointment or need for emergency services. Mental health services may also be provided in this format.
Apps
The AHRQ developed an app to help patients and families with their visits to healthcare providers (HHS, AHRQ, 2022) known as the AHRQ QuestionBuilder app. It is free and can be downloaded on a variety of devices. Prior to an appointment (whether in person or digital health) the patient uses the app to prepare questions, organize them, and even take photos-for example, of skin, pills, and so on. These options are only accessible to the patient who has downloaded the app. The AHRQ provides information on the use of the app.
Online Support Groups for Patients and Families
Online support groups can focus on any problem or disease. Patients and their families may use chat rooms, email, and websites for information sharing. Consumers gain information, education about their health and health needs, and support from others with similar problems. A healthcare provider may or may not be involved. Privacy issues must be discussed with participants, along with the risk of lack of privacy. Blogging has also become very popular and can be done by anyone with some basic technology information. This can make consumer information from some consumers more available to other consumers; however, as is true with any information available on the internet, the accuracy of that information is important-getting medical advice from laypeople is not necessarily the best choice. Blogging can, however, lend support and let consumers know they are not alone with their problems.
The internet can be an excellent source for all types of information, including health and medical information. When the internet is used as a source of health information, it is important to evaluate the websites because they are not all of the same quality. A nurse needs to consider the following factors when evaluating a website and guide patients in their use:
- The source or sponsor of the website: The government, academic institutions, healthcare professional organizations, and HCOs sponsor the most reliable websites.
- Status of the information: When was it posted or revised?
- Accessibility of the information on the site: Can one find what one needs?
- References provided for content when appropriate: Sources should be cited, and data should be current.
As is true with all methods such as the ones discussed in this section, patient privacy and confidentiality must be maintained. Notably, the risk of confidentiality problems increases with the use of technology. There are many ways that privacy can be violated, such as viewing data, overhearing conversations, and obtaining actual documents. It is the responsibility of healthcare providers, HCOs, insurers, and consumers (patients, families) to consider privacy a critical issue whenever technology is used and ensure as much as possible that information is safe-available only to those who need the information and with whom the patient wants the information shared.
| Stop and Consider 8 |
|---|
| During a single shift, a nurse will interact and use multiple HIT methods. |
The Future of Health Information Technology and Medical Technology
The future will continue to bring about expansion in the use of technology, informatics, and medical devices. This expansion is already in process. Cutting-edge technology is sometimes hard to believe, and examples of some of these changes are discussed next.
Nanotechnology
Nanotechnology-microscopic technology on the order of one billionth of a meter-will likely affect the diagnosis and treatment of many diseases and conditions in the future (Nanowerk, 2023; Gordon et al., 2007). Some examples are highlighted here:
- Sensing patients' internal drug levels with miniature medical diagnostic tools that circulate in the bloodstream
- Chemotherapy delivered directly to a tumor site, reducing systemic side effects
- New monitoring devices for the home: a talking pill bottle that lets patients push a button to hear prescription information, bathroom counters that announce whether it is safe to mix two medications, a shower with built-in scales to calculate body mass index (BMI), measuring devices in the bathroom to track urine frequency and output and upload data to a system or care manager, noninvasive blood glucose monitors to eliminate sticks, and sensors to compute blood sugar levels using a multi-wavelength reflective dispersion photometer
- Fitness monitoring
- Diagnostics and prevention methods
Wearable Computing
A computer can be worn, much as eyeglasses or clothing is worn, that interacts with the user based on the context of the situation, such as portable diagnostic devices (ANA, 2024). Wearable fitness tools are now popular. With heads-up displays, embedded sensors in fabrics, unobtrusive input devices, personal wireless local area networks, and a host of other context sensing and communication tools, wearable computers can act as intelligent assistants or data collection and analysis devices. Many of these devices are available now using smart fabrics. Sensors and devices can gather data during the patient's daily routine, providing healthcare providers or researchers with periodic or continuous data on the person's health while at work, school, exercising, or sleeping rather than the current snapshot captured during a typical hospital or clinic visit. A few applications for wearable computing devices include sudden infant death syndrome monitoring, ambulatory cardiac and respiratory monitoring, monitoring of ventilation during exercise, monitoring activity level of poststroke patients, monitoring patterns of breathing in asthma, assessment of stress in individuals, arrhythmia detection and control of selected cardiac conditions, and daily activity monitors (Ootex Specialty Narrow Fabrics, 2019).
Remote Telemetry Monitoring
Remote telemetry monitoring technology informs staff when a patient's condition has changed. Remote monitoring requires that the patient is placed on a monitor, and then signals are sent to staff through a pager system, which today may not even be within an HCO but, rather, an external alert to a healthcare provider. Staff may be informed, for example, of the patient's identity, heart rate, readout of rhythm without being right next to the patient, status of labor contractions, and other monitoring needs. This method is used more now in digital health.
Robotics
The use of robots has been expanding for years to deliver supplies to patient care areas. There have also been direct patient benefits, such as hand-assist devices to help patients regain strength after a stroke (Science Daily, 2016). Robots may provide a remote presence to allow physicians to virtually examine patients by manipulating remote cameras (Thomas, 2015). This technology is also used in remote surgery and virtual reality surgical procedures-for example, microscopic, minimally invasive surgical procedures might use the da Vinci surgical system that helps surgeons perform procedures for mitral valve repairs, hysterectomies, and prostate surgeries (Intuitive Surgical, 2023). This type of surgery has increased, decreasing some of the past surgical risks, decreasing the need for long hospital stays, and supporting more rapid overall recovery. In the future, robots may also be used more in direct patient care-for instance, to help lift obese patients, reducing staff risk of injuries.
Artificial Intelligence
Artificial intelligence (AI) and machine learning are growing areas of IT and have an impact on HIT; for example, they are related to the HHS mission “to enhance the health and well-being of all Americans” and are defined by the HHS (2023) as:
- Artificial intelligence enables computer systems to perform tasks normally requiring human intelligence.
- Machine learning, a type of artificial intelligence, gives computers the ability to learn without being programmed by humans.
With the expansion in AI, some AI tools are now used more in clinical care and are related to clinical decision support, mobile health, sensor-based technologies, and voice assistants and robotics (Douthit et al., 2022). As AI expands in HIT, healthcare education, and practice, it is important that nursing and other healthcare professional leaders consider the application of AI and develop relevant policies to address decisions about its use in education and ensure safe and quality care and support affecting practice and healthcare professions. The development of AI requires evidence from research to support effective EBP in using AI and consideration of legal and ethical issues related to its use. As some experts have noted, the boundaries between human- and nonhuman-driven issues need to be clearer (Johnson et al., 2023). The HHS notes that “artificial intelligence (AI) and machine learning are critical to the U.S. Department of Health and Human Services in accomplishing our mission to enhance the health and well-being of all Americans” (HHS, 2023).
Genetics and Genomics
Since 1997, the CDC's Office of Public Health Genomics has served CDC programs, other federal agencies, state health departments, and other external partners by identifying, evaluating, and implementing evidence-based genomics practices to prevent and control the country's leading chronic, infectious, environmental, and occupational diseases. In 2019, the office's name was changed to the Office of Genomics and Precision Public Health to reflect increasing emphasis on nongenomic precision health applications in public health (HHS, CDC, 2022). Genomics and precision public health are now important considerations in the healthcare system (HHS, CDC, 2023). Genetic data, especially when the data are integrated into EMR/EHR/PHR, are expected to advance customized patient care and medications targeted to individual responses to medications-precision medicine is recognized as a critical aspect of future health care. This is leading to more precise customization of treatment and medication based on the patient's unique DNA profile and past patient response to medications and other interventions. This will dramatically change how patient care is managed for specific diseases and conditions and will also apply to the prevention of some diseases. The inherent complexity of customized patient care will demand computerized clinical decision support that reflects individual needs and health history. Predictive disease models based on patient DNA profiles are an emerging medical development driven by a better understanding of DNA mapping. These advances have implications for a new model of care, HIT, and nursing care.
Nurse participation in the development of genomic HIT solutions is important. Nurses may collaborate with bioengineers and IT experts to develop new products, participate in research using these products, and help develop implementation and evaluation plans for use with these products. More than ever, patients will need to be partners in this development as part of patient/person-centered care.
Medical Devices
The development of medical devices has improved medical care. Some of these devices assist with diagnosis and others with treatment, rehabilitation, and ongoing health maintenance. Nurses use medical equipment daily, some of which is associated with HIT. The HCO is responsible for ensuring that equipment functions effectively and responding when questions are asked about its use or repair is required. Nurses also have responsibilities for reporting problems to appropriate persons in the organization. As the use of medical devices has expanded, so have adverse events associated with devices-safety is a critical concern: Is equipment working correctly and maintained, and does staff know how to use it correctly? One concern that is not yet clear is incident reporting of medical device concerns, which may result in underreporting of these incidents (Barlas, 2017; Polisena et al., 2015). The FDA MedWatch adverse event reporting program focuses on reporting medical device concerns, noting examples of medical devices that should be reported when adverse events occur. For example, several events could occur with devices, such as electric beds (electric shock, patient entrapment), patient lifts (patient and staff injuries), peritoneal dialysis machines (increased intraperitoneal pressure), and Foley catheters (infections, breakage). The FDA provides updated information on medical device problems on its website and examples of types of FDA-regulated products relevant to health (HHS, FDA, 2023):
- Prescription and over-the-counter medicines including those administered in a hospital or outpatient infusion center.
- Biologics, such as blood components, blood/plasma derivatives, blood transfusions, gene therapies, and human cells and tissue transplants.
- Medical devices, such as diabetes glucose test kits, hearing aids, breast pumps, and many more products.
- Combination products, such as prefilled drug syringes, autoinjectors, metered-dose inhalers, contact lenses coated with a drug, and nasal spray.
| Stop and Consider 9 |
|---|
| The nursing profession needs to be up to date on changes in technology because many will affect nursing practice. |
Digital Health
One of the major changes that is currently occurring in healthcare delivery is the expansion of digital health (telehealth/telemedicine), and many of the methods and examples discussed earlier in this chapter relate to this topic. The FDA describes digital health as:
The broad scope of digital health includes categories such as mobile health (mHealth), health information technology (IT), wearable devices, telehealth and telemedicine, and personalized medicine. Digital health technologies use computing platforms, connectivity, software, and sensors for health care and related uses. These technologies span a wide range of uses, from applications in general wellness to applications as a medical device. They include technologies intended for use as a medical product, in a medical product, as companion diagnostics, or as an adjunct to other medical products (devices, drugs, and biologics). They may also be used to develop or study medical products. (HHS, FDA, 2020)
The FDA identifies several benefits of using digital health:
- Reduces inefficiencies
- Improves access
- Reduces costs
- Increases quality
- Makes medicine more personalized for patients
Digital health requires the use of telecommunications equipment and communication networks for transferring healthcare information between participants at different locations, applying telecommunication and computer technologies to the broad spectrum of public health and medicine. It is part of the development of digital health. This healthcare delivery method has become a disruptor of health care, changing traditional care as it decreases travel time and use of time for patients and the provider (Finley & Shea, 2019). Telehealth supports PCC, and it also can assist in meeting STEEEP®. Healthcare providers need to understand how technology and digital health can positively impact quality care, which includes safety. It is important to maintain patient privacy, which is more at risk with the use of technology. Informed consent when using digital health is important and should be part of the care process. There are now more professional conferences on this topic and digital health indicating increased importance and need for research and publications along with more inclusion of content in healthcare profession degree programs. This technology offers opportunities to provide care when face-to-face interaction is difficult to access (such as in-home health care, school-based care, and rural areas). It is particularly useful when there is an increased health risk if face-to-face for the patient and healthcare provider, such as during the COVID-19 pandemic. Digital health can be used in a variety of settings and situations if the equipment is available (HHS, AHRQ, 2023a). Currently, two-way interactive video is the most effective digital health method. Telenursing refers to the use of telecommunications technology used to provide nursing care. This virtual method of care may be done with audio and/or visual methods. Telediagnosis is also a growing area, and the COVID-19 pandemic increased the use of telediagnosis along with digital health in general, expanding its use (HHS, AHRQ, 2023b). As an example, Figure 13-4 provides an overview of telediagnosis. The long-term impact of the growing use of digital health and telediagnosis is unknown-will it continue when the pandemic resolves and will its use evolve? For this process and its methods to be effective and provide quality care requires patient engagement and provider communication competency. It is also important to consider disparity issues, for example, access to the internet if required.
Figure 13-4 Stem-level and contextual factors impacting telediagnosis (tele-dx).
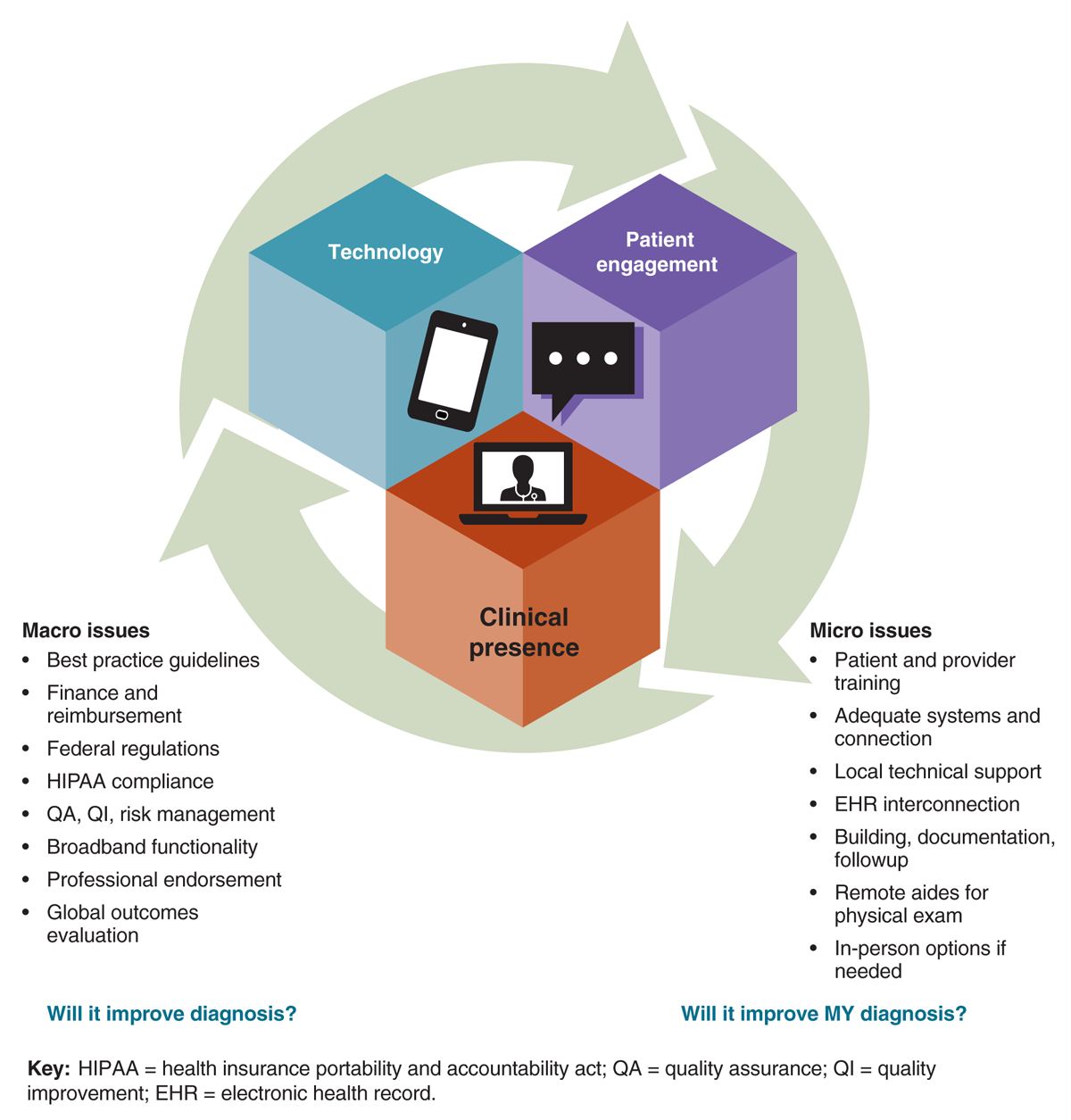
An infographic titled Stem-level and contextual factors impacting telediagnosis presents three interconnected cubes representing key components: Technology, Patient Engagement, and Clinical presence.
The technology cube includes an icon of a tablet, the patient engagement cube features an icon of a chat bubble, and the Clinical presence cube features an icon of a video call. On the left, under Macro issues, the diagram lists best practice guidelines, finance and reimbursement, federal regulations, H I P A A compliance, Q A, Q I, risk management, broadband functionality, professional endorsement, and global outcomes evaluation. On the right, under Micro issues, it lists patient and provider training, adequate systems and connection, local technical support, E H R interconnection, building, documentation, follow-up, remote aides for physical exam, and in-person options if needed. At the bottom, the text reads, Will it improve diagnosis? and Will it improve my diagnosis?
Reproduced from Graber, M. L., Hunte, H. E., Smith, K. M. Telediagnosis for Acute Care: Implications for the Quality and Safety of Diagnosis. Agency for Healthcare Research and Quality (AHRQ). August 2020. AHRQ Publication No. 20-0040-2-EF.
Issues that arise with digital health that may act as barriers include the cost of equipment and its use; staff training and also equipment for patients if they need to actively use the equipment at home, such as computers; limited or no insurance coverage (reimbursement) for these services; the need for clear policies, procedures, and protocols; privacy and confidentiality of information; and regulatory issues (for example, a nurse who is located and licensed in one state providing telenursing for a patient in another state where the nurse is not licensed). A systematic review of issues related to using digital health during the pandemic identified the following about this experience, which may impact continuing use not only during public health emergencies but applied to routine care (HHS, AHRQ, 2023b, p. viii):
- More likely used by people who are young to middle-aged, female, White, of higher socioeconomic status, and living in urban settings.
- When seen, differences in clinical outcomes were generally small and not clinically meaningful when comparing in-person with telehealth care.
- Telehealth may be less suitable and less desirable for patients with complex clinical conditions, those needing physical exams, and for therapies requiring the development of rapport between patients and providers.
- Providers note that the cost of telehealth can be a barrier to care, owing to limits to insurance reimbursement.
- Some patients perceive telehealth as a barrier to improved health outcomes due to the absence of a physical exam and challenges in developing rapport and communicating with their care team, potentially resulting in delayed or missed diagnoses.
Digital healthcare is the most active area of healthcare transformation today, with many more changes expected, and has led to the expansion of virtual nursing. An example of how a hospital is using these methods and developing a model of virtual nursing is using a virtual nurse who is not physically present but assists staff with many care activities, such as assisting staff with advice about patient care, charting, patient education and discharge, and participating or leading rounds (Bruce, 2023). Patients and families can also see the virtual nurse on the device screen and interact. Future applications will arise, and nurses need to consider how these developments might be used more in nursing practice, such as the use of AI. Many aspects of digital health also have implications for international health care because digital health provides a method for connecting expertise to patients who may need care that is not accessible in their home country-for example, during disasters. The AHRQ provides ongoing information and tools focused on assisting HCOs and providers (HHS, AHRQ, 2020).
In addition, the COVID-19 pandemic led to the need to examine innovative methods to meet nursing education needs when students may need to be protected from exposure. The American Association of Colleges of Nursing (AACN) recognized there was a need for faculty preparation to develop virtual education options and the need to adjust clinical experiences, as demonstrated in its special faculty conference in 2021 on this topic (AACN, 2021a). Another example of the increasing interest in preparing nurses for digital health and also examining nursing practice and digital health was the National Institute for Nursing Research webinar on this topic (NIH, NINR, 2021).
| Stop and Consider 10 |
|---|
| Digital health is an expanding area of health care that changes some aspects of current practice, creates new approaches, and includes government engagement. |
It is important to recognize, and the experiences in the pandemic reinforced, there was an academic preparation gap related to digital health and in ambulatory health practice. “Population health and community-focused care, fully leveraging ambulatory and telehealth practices, are the immerging venues of health care and a solution to health care equity and affordability. Accelerated academic reformation is pivotal to fundamentally prepare for the nursing's essential post-pandemic role” (Kollman, 2022, p. 60). The AHRQ Digital Healthcare Research (DHR) Program's vision is to ensure that every patient and care team has easy access to health data and knowledge at the point of care. This is connected to digital healthcare technologies, and related research holds the key to advancing care quality, safety, and effectiveness. The DHR program funds research focused on demonstrating how digital healthcare solutions can be designed and implemented to improve healthcare system performance and patient health outcomes (HHS, AHRQ, 2023c, 2023d). In 2022, AHRQ provided $29 million to support the DRH program's research and related evidence-based practice. Figure 13-5 identifies the DRH key digital health research themes. These themes provide guidance to HCOs and healthcare providers as they develop digital health and apply research evidence. Some of the AHRQ-funded digital health research projects relate to chronic disease management, such as improving the management of multiple chronic conditions with Mobile Patient-Reported Outcomes for Value and Effectiveness (mPROVE), implementation of an electronic care plan for people with multiple chronic conditions (MCCs), Care Transitions App for patients with multiple chronic conditions, using smart devices to implement an evidence-based eHealth system for older adults, and also evaluation of the spread and scale of PatientToc™ from primary care to community pharmacy practice for the collection of patient-reported outcomes (PROs), implementing personalized cross-sector transitional care management to promote care continuity, reduce low-value utilization, and reduce the burden of treatment for high-need, high-cost patient, and real-time symptom monitoring using ePROs to prevent adverse events during care transitions.
Figure 13-5 Key Digital Health Research Themes.

A diagram illustrates major themes in digital health.
The diagram presents three sections. The first section includes an icon of a hand holding patients, with the text Engaging and empowering patients. The second section includes an icon of two healthcare professionals, with the text Optimizing care delivery for clinicians. The third section includes an icon of a hospital building, with the text Supporting health systems in advancing care delivery.
U.S. Health and Human Services Department, Agency for Healthcare Research and Quality. (2023). AHRQ digital healthcare research program, 2022. https://digital.ahrq.gov/sites/default/files/docs/page/ahrq-dhr-2022-year-in-review-at-a-glance.pdf
HIPAA: Ensuring Confidentiality
HIPAA has had a major impact on healthcare delivery systems and healthcare communication. Privacy and confidentiality have long been problematic issues in health care. Because HIPAA focuses on the issue of information and confidentiality, it applies to HIT. The law also requires the implementation of data security and electronic transaction standards. With the growth of information sharing, it became increasingly evident that the existing means of transactions and systems were not ensuring privacy and confidentiality-key elements that had long been part of the healthcare delivery system. Privacy is the right of a person to have personal information kept private. As discussed in this text, this relates to professional ethics and has legal implications. Privacy restrictions even apply to family members, unless an adult patient specifically communicates that it is acceptable for family members to be given information. This cannot be assumed. Patients may also access their medical records.
HIPAA requires that only necessary information be shared among providers, including insurers. Also of concern is healthcare providers openly sharing information-for example, discussing patient information in public places, calling a patient's work or home, leaving a message that reveals information about health or health services, and so on. Carrying documents outside an HCO with patient identifier information is prohibited. This constraint has implications for students who may take notes or have written assignments that include this information. How information is maintained, such as on tablets, laptops, or smartphones, is also of concern. For example, taking pictures on smartphones in clinical settings, such as photos taken during surgery, is a privacy violation (Wilkerson, 2021). Many HCOs and healthcare profession education programs have implemented strict policies about taking patient photos, even if they are de-identified. Nurses and students should make sure they know their employer's or school's policies on smartphone and email use in a clinical setting and follow them.
The development of new technology has been moving so fast that critical prior issues have not always been addressed effectively. The 1996 law, however, requires that staff know the key HIPAA elements and apply them. As a result, HCOs and healthcare profession schools, such as nursing education programs, are required to provide information and training about HIPAA. Patients are informed about HIPAA when they enter the health system; they are given written information and asked to sign documents to indicate that they have been informed. Ensuring that the requirements are met must be incorporated into HIT. It is easy for patients and staff to report HIPAA violations to HHS via its website (HHS, 2022). Violations are examined, and the provider may have to pay a fee for not following HIPAA regulations.
| Stop and Consider 11 |
|---|
| When using HIT there is a high risk of problems with privacy and confidentiality. |
High-Touch Care Versus High-Tech Care
High-touch care is why most people become nurses, but nursing is much more than this today. This chapter describes the growing influence of technology on all segments of health care. This influence will not decrease but rather increase in the future. Nurses need to understand and know how to use technology applied to their practice areas. When possible, they need to be involved in the development and implementation of this technology-but there are concerns. When we “talk” through machines, do we lose information and the personal relationship? How can this be prevented so that we are not disconnected from our patients? How can we ensure that the information we are getting is correct and complete? Are people able to communicate fully through some of these other means? Over time the public has become increasingly comfortable with IT, which they are using more and more in their daily lives, but when it comes to their health care, they may want more personal communication. As nursing increasingly adopts HIT, nurses need to keep in mind the potential for isolation and the continuing need for effective patient communication throughout the care process. Nurses also must not forget the need for touch and face-to-face communication-though during the COVID-19 pandemic, the use of masks by staff and patients limited this type of communication, representing barriers that are difficult to overcome. When a nurse uses a computer or some type of handheld device while asking the patient questions and does not look at the patient, this limits patient engagement in the process.
The future will include many more new uses of technology; change is ongoing. For example, the e-intensive care unit (eICU) is used to monitor patients from afar to improve patient outcomes (Rouse, 2017). In this example, a system was attached to four hospitals in Iowa and their ICUs. This system allowed intensivists at a remote monitoring center to view patients' vital statistics, electrocardiograms, ventilators, and X-ray and lab results. The eICU included a two-way conference video capability so that patients and staff could interact when required. This type of system has advantages; for example, experts can be in one place and consult with staff in multiple locations that may not have the required expertise onsite. This is particularly useful in providing expert medical care for residents in rural and remote areas. There is no reason that this type of system should be limited to physician consultation because nurses can easily use it, too. For example, a nurse clinical specialist might view patient data and consult on patient care with nurses in an ICU in an external location. This increases access to information and expertise. The other side of this innovation coin is its effect on the touch side of care when the provider is not actually in the room with the patient. It is not clear how this might affect care because these types of systems are new. This is an area that is increasing, developing a new care model. Questions to consider as this area of virtual nursing is developed include (Boston-Fleischhaurer, 2017, p. 86):
- What is the core function of the virtual acute care nurse?
- What skills and competencies will be needed?
- How does the virtual acute care nurse interact with the on-site care team?
- Does the virtual acute care nurse interact with the patient and family, and if so, how?
- With increased consumerism, how will this role and this type of care delivery be received by patients and families?
- Will nurses derive professional fulfillment from a virtual role and, therefore, remain engaged?
- How will we measure the impact of virtual nursing care?
| Stop and Consider 12 |
|---|
| A computer can stand in the way of relating to patients. |
Nursing Leadership in Health Information Technology
We are currently at a critical junction for nurses and HIT competency, with all nurses called on to assume more leadership in the expansion of HIT. This call to action corresponds to the recommendations in The Future of Nursing report (IOM, 2011). There are changes in healthcare delivery and more dependence on HIT, and nurse informaticists should be part of the structure that develops and implements greater use of HIT (HIMSS, 2023a). To guide HIT in healthcare organizations, nurse leaders require HIT competencies to be effective in participating actively in HIT decision-making. “Skills in managing large outcomes, quality, and cost data sets are needed to ensure nursing is at the table and is able to advocate for nursing-specific needs” (Collins et al., 2017, p. 215). The competencies focus on the inclusion of nursing values, nursing information in the HIT system, budgeting needs for HIT, data-based planning, the impact on decision-making and utilization within HIT, and collaboration (Collins et al., 2017, p. 217):
- Ability to collaborate with other departments regarding project management and resource allocation for HIT system implementation.
- Ability to collaborate with chief medical officer peers related to HIT and the needs of nurses and physicians, advocating for effective HIT; communication includes benefits for nursing, frontline staff engagement in all levels design, development and evaluation of HIT, recognition of the importance of HIT in strategic planning, and need for quality assessment of HIT.
The AACN nursing education standards strongly support the need for HIT and medical technology content and experiences in nursing education: “Information and communication technologies and informatics processes are used to provide care, gather data, form information to drive decision-making, and support professionals as they expand knowledge and wisdom for practice. Informatics processes and technologies are used to manage and improve the delivery of safe, high-quality, and efficient healthcare services in accordance with best practice and professional and regulatory standards” (AACN, 2021a, p. 11).
The report titled Health IT and Patient Safety: Building Safer Systems for Better Care (IOM, 2012) made a strong statement that HIT was not something that is disconnected from care delivery or the providers of care, and this continues to be important for nursing management and leadership. “We are at a unique time in health care. Technology-which has the potential to improve quality and safety of care as well as reduce costs-is rapidly evolving, changing the way we deliver health care. At the same time, healthcare reform is reshaping the healthcare landscape” (IOM, 2012, p. ix). This report highlighted patient and family concerns about safety and shared responsibility. These same themes continue to be recognized and have also been emphasized throughout this text and relate to HIT.
| Stop and Consider 13 |
|---|
| With the expansion of HIT in all sectors of health care, nurses need to be leaders by participating in this expansion and providing feedback. |