There is much work to do to become a professional nurse. The history of nursing indicates that the development of the profession and its education has been a long process. As you strive to reach your goal, you will find that the nursing program of study is rigorous. This chapter focuses on the nursing student experience-what it is and what you need to understand and do to be successful. Nursing education differs from other types of educational programs and requires extensive experiences in labs, simulation, and clinical settings, requiring longer hours than nonnursing courses. Students are encouraged to assess their learning styles and methods used to successfully meet the educational outcomes. Long-term education is an important part of any profession, but especially for nursing to ensure that care is of the highest quality and based on the best evidence. Caring for yourself is also important both as a student as you prepare to be a nurse and as a practicing nurse.
Your Pursuit of a Profession: Making the Most of Your Educational Experience to Reach Graduation and Licensure
Beginning a nursing program is a serious decision. It means that you have chosen to become a professional registered nurse (RN). This text introduces you to the profession and provides an orientation to a variety of important content that will be covered in more depth in your future courses. One topic that needs to be addressed in the initial stages of your nursing education is how to make the most of the experience to reach your goal of graduation and licensure to practice as an RN and provide quality care. The following content discusses student and faculty roles, tools for success, examples of teaching and learning practices used in nursing education, opportunities to expand your experiences, and caring for yourself. This is all critical content-it may not be something you will be tested on, but the content provides some guidance to help you effectively navigate through the nursing education process.
Nursing education is different from other educational programs and courses. Students who enter a college- or university-based nursing program complete many courses in liberal arts and sciences as prerequisites to entering the full nursing curriculum. When students enter a nursing program, they arrive with certain expectations that are derived from their previous educational experiences. Students expect a didactic course like other courses they have taken, such as an English literature or a math course. That is, they expect to go to the class, sit at their desk and listen, and then periodically turn in assignments and take exams. In some cases, students have taken some of these courses online and now may even expect that nursing courses are online. This method is used in some nursing programs, and during the COVID-19 pandemic, there was increased use of virtual learning methods, as discussed in previous chapters.
Whether you take courses in a face-to-face traditional venue or as e-learning nursing courses, nursing courses demand more. Much of the content relies on knowledge gained in previous courses and builds to subsequent courses with the expectation that students apply content from their previous courses to their current courses and to their clinical experiences. Learning becomes more of a continuum, as opposed to neat packages of content that can be filed away when a course ends. Understanding is more important than memorizing (though some memorization is required), and the application of information becomes more important on exams and in practice. As this chapter makes clear, nursing education is different from other types of education. Nursing education is complex, but how did it get this way, and why is it this way? This content examines this difference.
Nursing education also emphasizes professional socialization in the learning process. Professional socialization focuses on new nurses understanding and integrating nursing beliefs, values, cultural norms, and behavioral expectations so that they will be able to think, act, and provide patient care in ways that are aligned with the values of the nursing profession, including consideration of diversity, equity, and inclusion (DEI) in all types of healthcare settings and for all types of patients (Johnson, 2022). This learning process takes time, is integrated throughout your nursing education experiences, and continues through the first few years of your professional life as an RN.
| Stop and Consider 1 |
|---|
| You need to understand the nursing education experience process and apply this understanding to effective learning and nursing practice. |
Student and Faculty Roles
Throughout your nursing education, you need to assume a very active role in the learning process and take responsibility for your own learning; this is not passive learning. Students who ask questions, read and critique, apply information even if it is risky, and are interested in working with others-not just patients and their families but also fellow students and faculty-will be more successful. Students who wait to be told what to do and when to do it will not be as successful.
Nursing faculty facilitate student learning. This is done by developing course content and by using teaching-learning practices to assist the student in learning the required content and developing required competencies. Faculty enhance learning in the simulation laboratory and in clinical settings by guiding students to practice and become competent in areas of care delivery, applying knowledge to practice. The best learning takes place when faculty and students work together and communicate about needs and expectations. Faculty members not only plan learning activities for a group of students but also assess the learning needs of individual students and work with them to meet course and program objectives or outcomes. A critical key to student success with faculty is communication and meeting outcomes: Ask questions, ask for an explanation if confused, meet course requirements when due, and use the faculty as a resource to enhance learning.
Becoming an RN involves more than just graduating from a nursing program. New graduates must pass the National Council Licensure Examination (NCLEX), a national examination that is not offered by the school of nursing but rather through the National Council of State Boards of Nursing (NCSBN) and state boards of nursing, as discussed in previous content (NCSBN, 2023a). Throughout the nursing program, students may be offered opportunities to complete practice exams and receive feedback. In addition, course exam questions are typically written in the formats found in the NCLEX, such as application of knowledge questions rather than questions relating to memorized content. Becoming comfortable with this format is often difficult for new nursing students because they are accustomed to taking exams in nonnursing courses that focus less on application and do not build on knowledge gained from course to course. For example, in nursing, you complete the anatomy and physiology course, and then you must apply this information later when you take exams on clinical content. You learn about blood flow through the heart, and then, in conjunction with adult health content, you are expected to understand this content and apply it when providing care to a patient with a myocardial infarction (heart attack). Months or more may elapse between your completion of a anatomy and physiology course and when you take an adult health course or care for a patient with a myocardial infarction.
| Stop and Consider 2 |
|---|
| Both faculty and students have responsibilities in the nursing education process. |
Student Learning Styles
As you begin nursing courses, it is helpful for you to consider your own preferred learning style and determine how your style might or might not be effective. If it is not effective, you may need to consider changes.
What does learning style mean? Learning style is a student's preference for different types of learning and instructional activities. There are a variety of views of these styles. When you assess your personal learning style, you might apply Kolb's (1984) learning style inventory, which was further developed by Honey and Mumford (1992). This perspective of learning describes a continuum of four learning styles: (1) concrete experiences, (2) reflective observation, (3) abstract conceptualization, and (4) active experimentation. No person can be placed in only one style category, but most people have a predominant style (MindTools, 2023; Rassool & Rawaf, 2007):
- Divergers: Sensitive, imaginative, and people oriented; often enter professions such as nursing; excel in brainstorming sessions.
- Assimilators: Less focused on people and more interested in ideas and abstract concepts. Excel in organizing and presenting information; prefer formal education formats; prefer reading, lectures, exploring analytical models, and having time to think things through.
- Convergers: Solve problems and prefer technical tasks; less concerned with people and interpersonal aspects; often choose careers in technology; excel in getting things done.
- Accommodators: People-oriented, active learners; excel in concrete experience and active experimentation; prefer to take a practical or experimental approach; attracted to new challenges and experiences.
Adapting Kolb's proposed styles, the following was described by Rassool and Rawaf (2007):
- Activists: Have an experience. Focus on immediate experience; interested in here and now; like to initiate new challenges and be the center of attention.
- Reflectors: Review the experience.
- Observers: Prefer to analyze experiences before acting; good listeners; cautious; tend to adopt a low profile.
- Theorists: Conclude from experience. Adopt a logical and rational approach to problem solving but need some structure with a clear purpose or goal; learning is weakest when they do not understand the purpose, when activities are less structured, and when feelings are emphasized.
- Pragmatists: Plan the next steps. Prefer to try out new ideas and techniques to see if they work in practice; are practical and down to earth; like solving problems and making decisions.
Understanding your style can help you when you approach new content, read assignments, and participate in other learning activities. It can affect how easy or difficult the content and assignments may be for you. You may need to stretch-that is, to try to learn or do something that is challenging for you-and you may need to adapt your learning style.
| Stop and Consider 3 |
|---|
| Your past learning styles may or may not be effective for you in the nursing program. You need to assess your learning process and outcomes and adapt as needed. |
Tools for Success
Organization and time management are very important tools for success in a nursing program. In the past, you may have gone to class for a few hours a day, but in nursing programs, some courses meet once or several times a week for several hours. Some courses may be taught online but may also require some attendance in a classroom setting or are only offered in an e-learning format. In addition, the program's clinical experience requirements have a major impact on your schedule. You need to prepare for the clinical experiences and work this activity into your schedule to meet course requirements. Study skills and test-taking skills are critical to meeting learning outcomes. This educational experience will not be without some stress; thus, if you develop stress management skills to help you cope, you may find that the experience can be better handled. Exhibit 4-1 provides some links to websites with tools for student success.
| Exhibit 4-1 Links for Student Success |
|---|
|
Time Management
Time management is not difficult to define, but it is difficult to achieve. Learning how to manage time and study requirements has an impact on effective nursing practice. Time-management skills in school are not different from what is required for clinical practica (experiences) and after graduation in practice. Figure 4-1 describes how to get started with time management.
Figure 4-1 Getting started with time management.
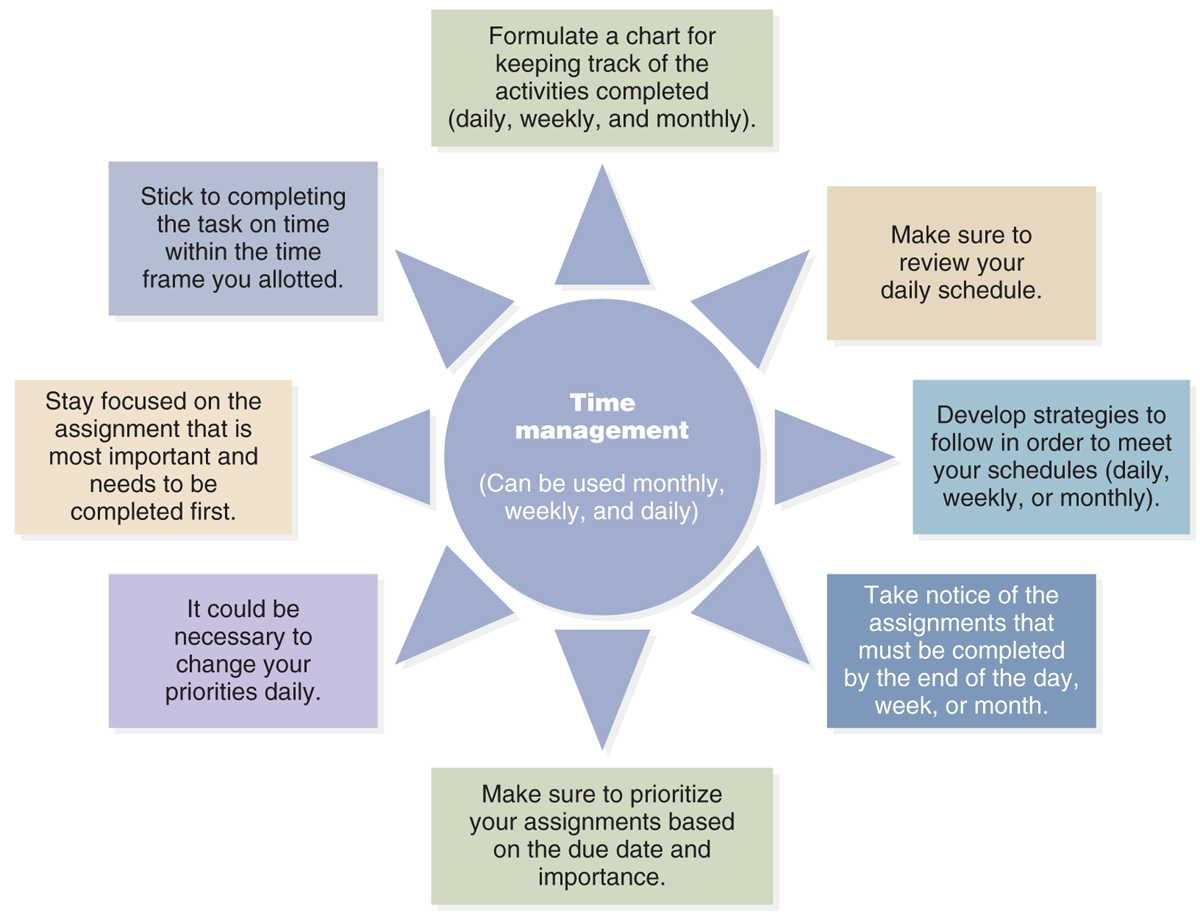
An infographic lists the strategies for effective time management.
The infographic is centered around the concept of Time management, which is usable monthly, weekly, and daily. The infographic includes various directives for managing time: Stick to completing the task on time within the time frame you allotted, Stay focused on the assignment that is most important and needs to be completed first, It could be necessary to change your priorities daily, Formulate a chart for keeping track of the activities completed, daily, weekly, and monthly, Make sure to review your daily schedule, Develop strategies to follow in order to meet your schedules, daily, weekly, or monthly, Take notice of the assignments that must be completed by the end of the day, week, or month, and Make sure to prioritize your assignments based on the due date and importance. Each box connects logically to illustrate the interconnected steps in managing time effectively.
Wilfong, D., Szolis, C., & Haus, C. (2007). Nursing school success: Tools for constructing your future. Jones & Bartlett Learning.
Most feel there is never enough time, and no one can make more time, so it is best to figure out how to make the most of your available time. Everyone has felt unproductive or been guilty of squandering time. In simple terms, productivity is the ratio of inputs to outputs. What does a person put into a task or activity (resources such as time, energy, money, giving up doing something else, and so forth) that then leads to outcomes or results? For example, one student studies 12 hours for an exam and before the exam gives up going to a film with friends; another student studies 5 hours and goes to the same film. These two students put different levels of resources into exam preparation, and they get different results-the first student makes an A on the exam, and the second a B. The second student then must decide if the result or grade was worth it. Should more time be spent on studying for exams and arranging their personal schedule to allow for some fun after exams? Or is the B grade acceptable? The student with the A grade may decide too much time was spent on studying and could have been organized better to reduce study time and yet meet positive outcomes. This more global perspective is certainly one aspect of time management, but time management also gets into the details of how one uses time to be efficient and effective, such as what the student with the A grade considered. You need to know yourself and what works for you.
Time analysis is used to assess how one uses time and considers available time and other activities. You might keep a log for a week and record your activities, including time spent on each activity and interruption. If you commit to collecting this information, you need to be honest so that the data truly reflects your activities. After the data are collected, you then need to analyze the data using these questions:
- Did you develop a study plan and priorities, and did you apply it? Were there priorities that you now consider less important or should not have been priorities when set? Do you need to adjust how you plan your study activities?
- What were your activities, and how long did each take? If you had a plan, this could help you assess your activities.
- Do you see a difference on certain days as to your activities and time?
- What did you complete, and what did you not complete? Can you identify reasons for not completing a task or project?
- What types of interruptions did you have? How many interruptions were important and unimportant, and why?
- Did you procrastinate? Are there certain activities that you put off more than others? Why?
- Did you jump from one task to another, and why?
- Look at your telephone calls, emails, texting, and so on. How did they affect your time management?
- Did you spend time getting ready to do a task, communicate with others, and so on? Was some of this required, or could it have been done more effectively?
- Did you take breaks? (Breaks are important.) How many breaks did you take, how long were they, and what did you do? Did it refresh you?
- Did you consult your calendar and use it as a guide?
- Are there times during the day when you are more productive? Knowing when you tend to be more productive provides you with the opportunity to capitalize on this and try to do some tasks during this time.
You need to work on time management and planning as a student because nurses need to be able to plan their day's work and still be flexible as changes occur. Ideally, nurses set priorities and follow through, evaluate how they use their time, and cut down on wasted time so that care can be delivered effectively and in a timely manner. They need to use communication effectively and prepare for procedures and other care delivery activities in an organized manner so that they are not running back and forth to get supplies and so on and handle interruptions by determining what is important and what can wait. Your success in meeting these demands relates to your need to assess your own time management and develop time-management skills.
Technology has made life easier and more organized in some respects, especially with the use of computers, smartphones, and tablets, as well as emails, text messaging, and other communication methods. However, these devices and methods can also interfere with time management. For example, you may stop what you are doing to answer an email or a text message that just arrived, or you may spend so much time syncing all this technology that your work does not get done. Managing time today means managing personal and professional technology, too.
Many people struggle with the same time-management problems. Consider these examples and how they might apply to you:
- Lack of planning-not using a calendar effectively or not using one and not developing a study plan or a plan for a course project
- Lack of setting goals and priorities or having unclear goals and priorities
- Allowing too many interruptions
- Lack of preparation for a task or activity (planning)
- Inability to say “No” often leading to overcommitment (the most common problem for many people)
- Inability to concentrate
- Insufficient rest, sleep, exercise, and an unhealthy diet, making one feel perpetually tired
- High stress level
- Too much socializing when work needs to be done-not knowing how to find the right balance
- Ineffective use of communication tools, including overuse of email, computer and internet, cell phone, and so on
- Too much crisis management-waiting too long to act so that it is then a crisis to get the work done
- Inability to break down large projects into smaller projects or steps
- Wasting time-focusing on little tasks, procrastination
Other, more serious problems can have a major impact on time management. These difficulties arise when the student does not feel competent or does not know what is expected. Students often experience these problems, although they may not recognize them or want to admit them. Nevertheless, these feelings can lead to problems with time management as students struggle to feel better and/or try to figure out what they are supposed to do. If you experience one or both feelings, you need to talk openly with faculty about your concerns. You are not expected to be perfect. The educational process is focused on helping you gradually develop your competence. In some cases, perfectionism may become a barrier to completing a task; you may fear that the task will not be completed perfectly, so you avoid the task or work on it longer than needed.
Benner (2001), a nursing education leader, described the experience of moving from novice to expert in nursing, which is viewed as a practice profession. Beginners or novices have no experience as nurses and, therefore, must gain clinical knowledge and expertise (competence) over time. Some beginning students enter a nursing program with some nursing care experience, such as nursing aide experience. This student may then be at a different novice level but still a novice. Most students, however, have no previous experience before beginning a nursing program. It is also important to recognize that a new graduate is not an expert; this comes with time and experience. This change in status can be difficult for students who may have felt that they were competent in understanding the content after a course, such as American History or Introduction to Sociology. Nursing content is different with competency developing over time. Each course and its content are relevant to subsequent courses. There is no neat packaging that allows one to say, “I have mastered all there is to know about nursing” or a nursing topic. With ongoing healthcare changes, the profession must adapt to changes, new knowledge and technology, identification of new health problems, and so on. Caring for a patient is a changing experience, with the nurse adapting as needed.
Another component of time management is setting clear goals and priorities. This helps to organize your time and focus your activities. You need to consider what is needed now and what is needed later. This is not always advice that is easy to follow; sometimes, you may prefer to work on a task that is not due for a while, avoiding work that needs to be done sooner. Sometimes, writing down goals and priorities and putting this information where it can be seen is helpful so that you can focus more on a time-management plan. Delegation is an important activity in health care and is related to time management. One of the key issues when prioritizing is determining who should complete the task and the time frame. Perhaps someone else is a better choice to complete the task; in this case, the task may be delegated, a topic discussed in this text.
Tasks and activities can be dissected. Consider the task elements, schedule and due dates, amount of time required to complete the task, the importance of the task and its impact, and the consequences if it is postponed or not completed. Plan how the work will be done to meet the due date. Large projects are best broken into smaller parts or steps. For example, the preparation of a major paper should be broken into a series of tasks, such as identifying the topic or problem, working with a team (if writing the paper is a team assignment), completing the research for the paper, writing the paper (which should begin with an outline), reviewing and editing, and polishing the final draft to submit by due date. Identifying deadlines for the steps better ensures that the final due date is met. Many large papers or projects in nursing courses cannot be completed overnight. They may require active learning, such as interviews, assessments, extensive research of relevant nursing literature, and other types of activities. A presentation may need to be developed after the paper is written or a poster designed. Often, this type of work is done with a team of students, which is an important experience because nurses work in teams. Group efforts take more time because team members must learn to work together, develop and effectively apply a teamwork plan, and ensure effective communication. Some team assignments are now done “virtually” through online activities in which students never physically meet. Getting prepared for the clinical experience/practicum is also a larger task that is described later in this chapter. All of this requires organization.
Some strategies for improving time management that you might consider include the following:
- Use a calendar or electronic method for a calendar; update it as needed.
- Develop a daily time management plan (see Figure 4-2).
- Decrease socializing at certain times to improve productivity.
- Limit the use of your mobile phone, text messaging, and email during key times.
- Identify typical interruptions and control them.
- Anticipate-flexibility is necessary because something can happen that will disturb the plan.
- Determine the best time for you to read, study, prepare for an exam, write papers, and so on. Some people are more effective in the early morning, others late at night. Know what works best for you.
- Work in blocks of time, minimizing interruptions.
- Develop methods for note taking and organizing learning materials to decrease the need to hunt for these materials.
- Conquer procrastination. Try dividing tasks into smaller parts to get a project done.
- Be prepared for class, clinical laboratory/simulation, and clinical experiences. Preparation means that less time will be spent figuring out what needs to be done when you need to be doing it.
- Do not use electronic communication during class for nonclass-related interaction or during clinical experiences.
- Do the right thing right, working effectively and efficiently.
- Remember that time management is not a static process but rather a dynamic one; your time management needs will change.
- Organize your electronic course files so that they are easy to use.
Figure 4-2 Daily time management worksheet.
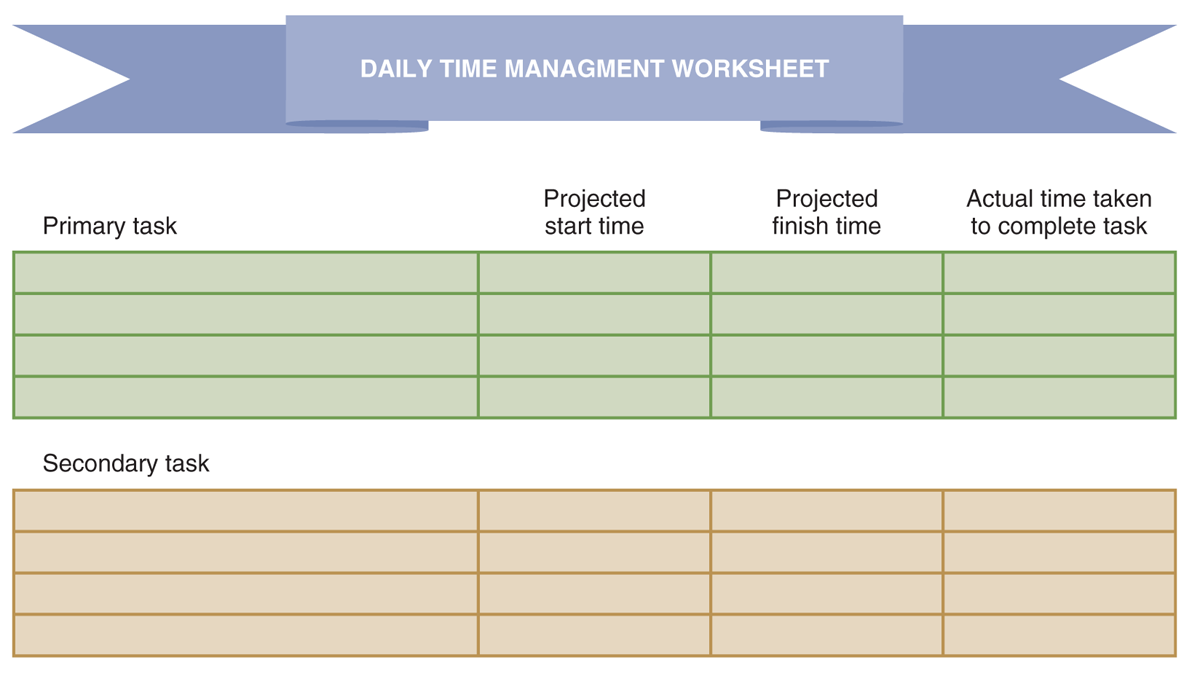
A worksheet template for daily time management with sections for primary and secondary tasks.
The worksheet is designed to organize tasks into primary and secondary categories. Each task category has columns labeled Projected start time, Projected finish time, and Actual time taken to complete task. The primary and secondary task sections have multiple rows for detailed time planning.
Wilfong, D., Szolis, C., & Haus, C. (2007). Nursing school success: Tools for constructing your future. Jones & Bartlett Learning.
Study Skills
Study skills are developed over time; however, this does not mean that these skills cannot be improved. You may also find you need to use different study skills for nursing courses and clinical experiences. This is the time to review your study skills and determine what can be done to improve them. Typical components of study skills are reading; using class time effectively; preparing written assignments and team projects; and preparing for discussions and other in-class learning activities, quizzes, and exams. In nursing, clinical preparation, which is new for students entering nursing programs, is also a key preparation area.
Preparation
Students need to prepare for class, whether it is a traditional classroom, a seminar, or an online course/distance education. The first issue is what to prepare. The guide for this is the focus of the experience and its objectives/learning outcomes. Use the course syllabus and other course materials as a guide for meeting course and student expectations. The learning format influences preparation, for example, attending a class session with 60 students versus a seminar with 10 students. The latter is an experience in which the student will undoubtedly be expected to respond to questions and discuss issues. A classroom setting may use varied teaching-learning methods; it might be a straight lecture, with little participation expected, or it might include participation requiring preparation-class team discussion. You need to be clear about the course expectations. If the course syllabus or other course materials do not provide clear explanations, you are responsible for asking about expectations or seeking clarification of confusing expectations. You then need to complete any work, such as reading or researching a topic, that is expected prior to the class for the experience to improve your learning and participation. Class time in nursing courses often emphasizes the application of information, which means you need to be prepared for the course sessions and participate.
Reading
There is a lot of reading to do for courses in a nursing program, ranging from textbooks and published articles to internet resources and handout materials that faculty provide. It is very easy to become overwhelmed by these materials. When you begin a course, explore the textbook(s) from front to back. Sometimes, students do not realize that a textbook has a valuable glossary, appendix, and index that could help them. Review the table of contents to become familiar with the text preface or introduction and the organization of the content. Some faculty may assign specific pages rather than entire chapters, so noting the details of a reading assignment is critical. Review a chapter to become familiar with the text chapter structure. Typically, there are objectives or outcomes, a chapter outline, and key terms; content divided into sections with headers and subheaders; additional elements, such as exhibits, figures, and boxed information; and the summary, learning activities, and references. An increasing number of textbooks have an affiliated website that offers additional information and learning activities and, in some cases, quiz-style questions.
Many textbooks are now published as e-books or offer this option, published as e-book and hard copy. E-books are often highly interactive (for example, you can highlight material, take notes, and search for content in the text), and the e-book can be downloaded to computers and tablets, smartphones, and so on.
This may be overwhelming, and where does one begin? How do you make the best use of your reading time? Reading should focus on four goals:
- Learning information for recall is memorizing. This is important for some content, but if it is the only focus of reading, you will not be able to apply the information and build on learning.
- Comprehension of general principles, facts, and examples is an important component of effective reading.
- Critical evaluation of the content should be part of your reading process. Ask yourself questions and challenge the content. Does it make sense?
- Application of content is critical in nursing because nursing is a practice-oriented profession. For example, at some point, you will take a course that focuses on maternal-child content; later, you will be expected to apply that content in a clinical pediatric unit. How you read and understand the content will make a difference in your ability to apply the content to a case in the classroom, a simulation experience, or in a clinical setting.
As noted in the previous section on time management, time is valuable. The student who is trying to develop more effective reading skills should not waste time but rather should accomplish specific goals in a timely manner. The following are some tips to use in reading a textbook chapter:
- Take a quick look at the chapter elements-objectives/outcomes, terms, headers, and subheaders-and compare them with the course content expectations. Pay particular attention to the chapter outline, if there is one, and to the summary, conclusions, highlights, and/or key points at the end of the chapter.
- Read through the chapter but not for details; the goal is to get a general idea of the content. Chapter headers and subheaders are good guides in understanding the chapter's organization.
- Go back and highlight key concepts, terms, and ideas. If this is done first, it can lead to over-highlighting. Using different colors for different levels of content may be useful for some students. You will need to go back and study the content; just highlighting content is not studying. The goal is to find a system that works for you. If using an e-book, understand and use its features.
- Note exhibits, figures, tables, and boxes. (This is when it is important to check the reading assignment. Does it specify pages or content to read or ignore?)
- Some students make notes in the margins, highlight key points, and so on. Others may jot down key points to refer to later in notes.
Figures 4-3 and 4-4 illustrate two different formats for organizing notes from readings (if notes are taken).
Figure 4-3 Taking two-column notes.
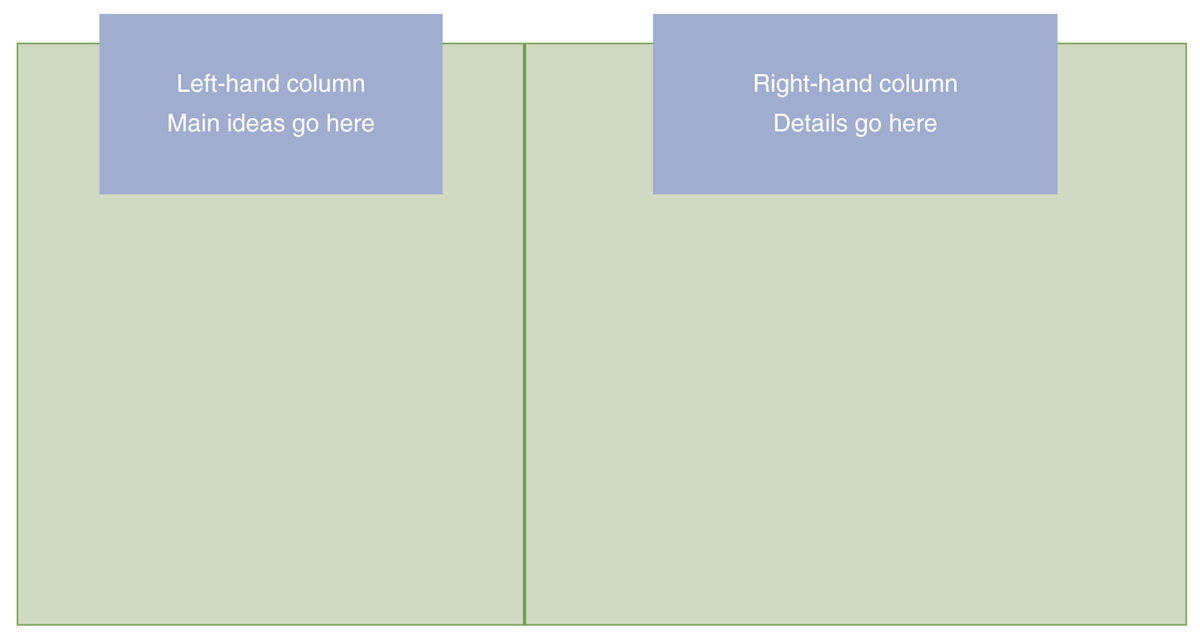
A template for two-column note-taking with designated areas for main ideas and details.
The template depicts a note-taking template structured into two columns. The left-hand column is labeled Main ideas go here and the right-hand column is labeled Details go here.
Wilfong, D., Szolis, C., & Haus, C. (2007). Nursing school success: Tools for constructing your future. Jones & Bartlett Learning.
Figure 4-4 Unit organizer.
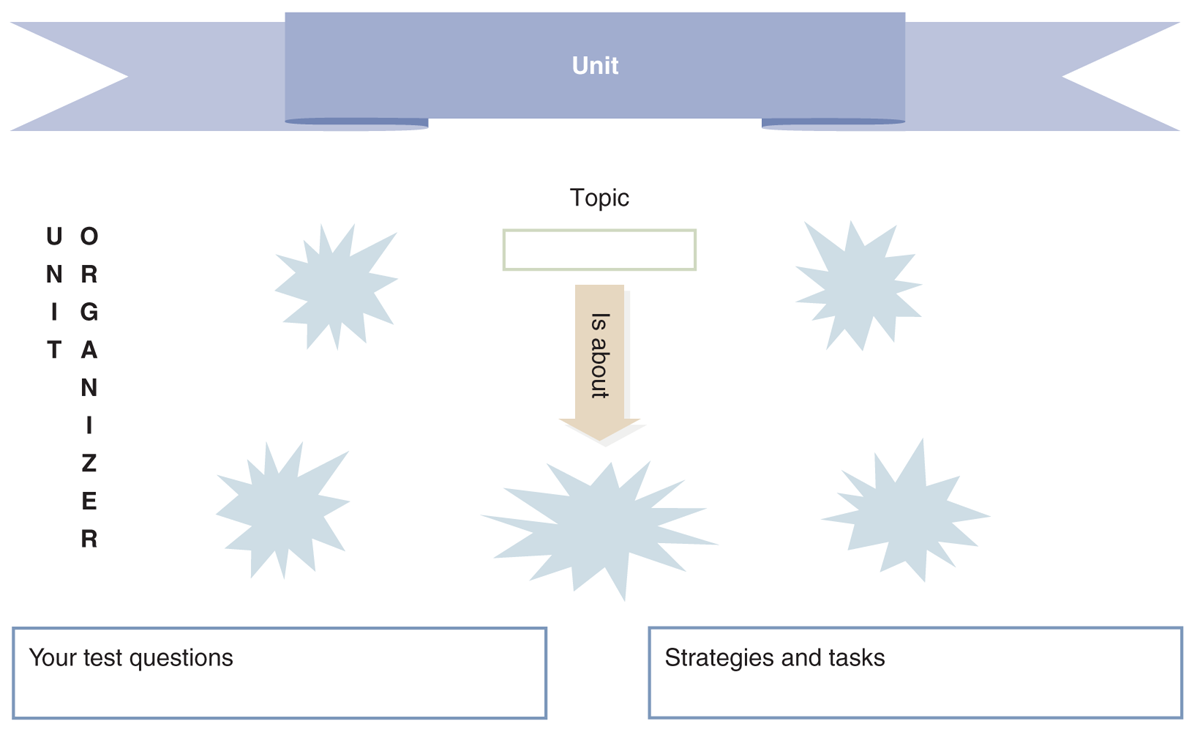
An educational unit organizer template with sections for unit, topic, test questions, and strategies.
At the top, a banner labeled Unit indicates where the unit title is noted. Below this, a central section titled Topic contains a box to specify the topic. Arranged around the topic are several blank spaces, representing what the topic is about. The bottom of the template features two boxes: Your test questions on the left for listing potential exam questions and Strategies and tasks on the right for outlining study strategies and tasks related to the unit.
Wilfong, D., Szolis, C., & Haus, C. (2007). Nursing school success: Tools for constructing your future. Jones & Bartlett Learning.
Using Class Time Effectively
Attending a class session can be a positive or negative learning experience. Preparation is important. In addition, how you approach the course and an individual course session is important. If you have trouble concentrating, sitting in the back of the room may not be the best approach. Sitting with friends can be helpful, but if it means you cannot concentrate, alternatives need to be considered. It is often difficult to disconnect from other issues and problems, but class time is not the place to focus on them. One of the most common issues in class sessions involves students who use class time to prepare for another class-working on assignments, studying for an exam, and so on. In the end, the learning experience on both ends is less effective. Students waste their time if they come to class without completing the reading, analyzing the content, or preparing assignments.
Another element of preparation for class and other learning experiences involves identifying and accessing needed resources, such as the textbook, a notebook, assignments, and so on. Some students use laptops and tablets in class, so planning for access if the battery runs out is important. Learning in the classroom will be compromised if a student uses electronic equipment, such as a laptop, tablet, or smartphone, for purposes that do not involve course content. Today, electronic devices are used more frequently in the classroom and for studying. Student options with these devices have expanded with the development of apps and pens for tablet writing and access to e-books. If you choose to use these options, research carefully what is available and how it might provide support for your learning. Make sure you know how to use the new options prior to using them in a course. The internet includes a lot of information, software, apps, and so on that may be used by students.
If a course has face-to-face sessions, taking notes is important, for example, using the methods noted above in Figures 4-3 and 4-4. It is critical to find a note-taking strategy that works for you and the content. Some students may be visual learners, in which case they may draw figures, charts, concept maps, and so on to help them remember something-for example, using a tablet with a stylus pen to make sketch figures. Going back and reviewing notes soon after a class session will help you remember items that may need to be added and recall information over the long term. As notes are taken in class, include comments from faculty that begin with “This is important,” “You might want to remember this,” and similar indicators of the material's importance. Questions that faculty ask should be noted.
It is easy to get addicted to PowerPoint slide presentations and think that if you have the slides available in a handout or in electronic form, learning has taken place. In reality, presentation content is only part of the content that nursing students are expected to learn-and just having presentation slides does not mean you understand the material. The faculty may make additional comments related to the content on the slides. Students need to pay attention to content found in reading assignments, research, written assignments, and clinical experiences and how they interrelate. Online courses may also include slide presentations, and some may have audio components, as well as other learning resources and activities. Students should use these options to augment their learning, even if not required.
Using the Internet
The internet has become a critical tool in the world today. As students increasingly turn to the internet to get information, it is important that reputable websites are used. Government sites are always appropriate sources, and professional organization sites also have valuable and appropriate information. Identify who sponsors the site. Bias is always a concern; for example, the site for a pharmaceutical company will inevitably praise that company's own products. Wikipedia is often used by students, but it is not always considered a scholarly resource for references. It is important to ask faculty about using this resource in assignments. When using a site, check its current date and or when it was last updated. Sites that are not updated regularly have a greater chance of including outdated information.
In addition, the internet is now used frequently for literature searches, usually through university libraries that offer online access to publications. Students need to learn about the resources available to them through their school libraries and learn how to use them effectively. Often, libraries offer short workshops (face-to-face and online) and orientation materials on the library website to assist students. It is important to properly attribute the source for content taken from the internet for an assignment, using the correct citation format required by your school of nursing.
Preparing Written Assignments and Team Projects
The critical first step for any written assignment is to understand the assignment-what is expected. Read directions for assignments carefully and ask questions if unsure about expectations. What are the evaluation rubrics? You then complete the assignment based on these expectations. If the assignment describes specific areas to cover in a paper, this should be an important part of the outline for the paper-and these areas may even be used as key headers in the paper. Faculty will look for content based on the assignment outline. If you have questions about the assignment as you work, ask faculty prior to submission and preferably before you get too far along.
For some assignments, students select their topics. If possible, selecting a topic like one used for a different assignment might save some time, but this does not mean that the student may submit an assignment that was done for another course. Plagiarism and submitting the same paper or assignment for more than one course are not acceptable. You need to be aware of and apply your school's honor code. These codes relate to cheating on exams or quizzes and to plagiarism, which demonstrates a lack of professional ethics.
Correct grammar, spelling, writing style, and citation format are critical for every written assignment. Nurses need to know how to effectively communicate, both orally and in written form. Use your school's required method for citations. Editing your work and checking it carefully are your responsibilities before you submit an assignment.
Some assignments require that you work with a team or group of students. Some students do not like this type of project, but these experiences provide opportunities to learn about working in teams, which is important in nursing. Teamwork requires clear communication among members and an understanding of the expectations that the team needs to meet. Effective teams spend time organizing their work and determining how they will communicate with one another. To complete team projects successfully, teams must decide how to complete the assignment, which might involve analysis of a case; writing a paper; developing a poster, presentation, or educational program; or another type of activity. Having a clear plan of what needs to be done, by whom, and within the timeline will help guide the work and decrease conflict. Everyone is busy, and preventing conflicts and miscommunication decreases the amount of time needed to do the work. If serious problems arise with communication or workload equality that the team cannot resolve, faculty should be consulted for guidance. Conflicts may occur, and these conflicts need to be dealt with before they get worse. If the student team is required to document its work and evaluate peer members, this should be done respectfully, honestly, and objectively, with appropriate feedback and comments about the work. Such evaluations are not easy to do. Additional information on teams is provided in other chapters in this text and applies to work you may do with a student team to complete a team project, team discussions, and so on.
Preparing to Take Quizzes and Exams
Quizzes and exams are inevitable parts of nursing education. Students who routinely prepare for them will experience less pressure at quiz or exam time-but this takes discipline. Building reviews into your study time, even if a review lasts for only a short period, makes a difference in quiz and exam preparation.
As is true for any aspect of a learning experience, knowing what is expected is the first step in quiz and exam preparation. What content will be covered in a specific quiz or exam? What is the time frame for the quiz or the exam? What types of questions are expected, and how many? Exams in nursing typically use multiple-choice, true-or-false, essay, and some fill-in-the-blank questions, although the most common format is multiple-choice questions. The first quiz or exam in a course is always the hardest, as students need to get to know the faculty and the style of questions. Some faculty may provide a review guide, which should always be used.
Before a major exam, getting enough rest is an important aspect of preparation. Fatigue and sleep deprivation interfere with functioning-reading, thinking, managing time during the exam, clinical practice, and so on. Eating is also important. Students usually know how they respond if they eat too little or too much before an exam.
One aspect of nursing exams that seems to create problems for new students is the use of application questions. Preparing for a nursing exam by just memorizing facts will not lead to a positive result. You need to know the expected information, but you must also know how to use the information in examples. This approach will help you prepare for the NCLEX exam.
Another common exam-taking problem is the inability to understand a multiple-choice question and its possible responses/answers. Students may skip over words and think something is included in the question that is not. They may not be able to define all the words in the question and may not identify the keywords. Reading the question and the response options carefully will make a difference. You should identify the keywords and define them. If you do not know the answer to a question, you should narrow the choices by eliminating responses that you understand or think might be wrong. Then, you should look for qualifiers, such as “always,” “all,” “never,” “every,” and “none,” because these may indicate that an option is not correct. Figure 4-5 describes a system for preparing for multiple-choice exams.
Figure 4-5 Multiple-choice exams.
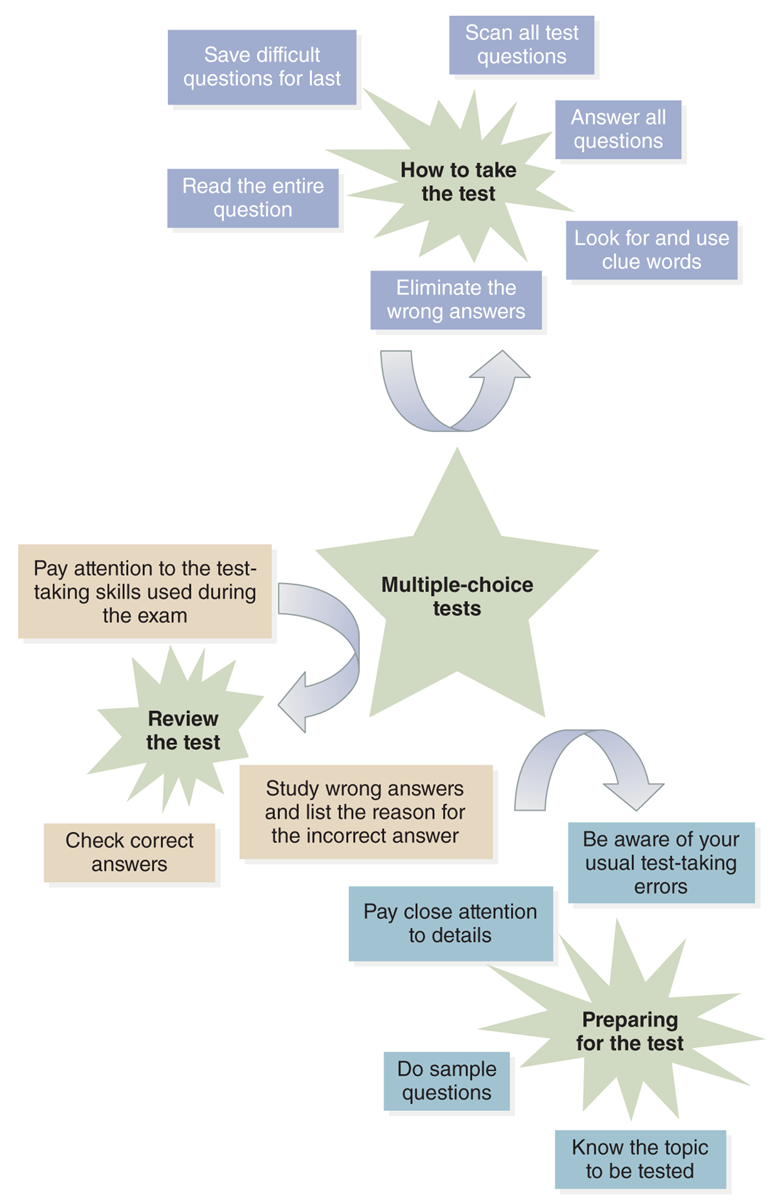
A diagram illustrates strategies for preparing, reviewing, and taking multiple-choice tests.
The strategies are as follows: The test taking tactics include the following: Scan all test questions. Answer all questions. Look for and use clue words. Eliminate the wrong answers. Read the entire question. Save difficult questions for last. The second diagram highlights preparation strategies, starting from Multiple-choice tests and proceeding through Know the topic to be tested, preparing for the test, Be aware of your usual test-taking errors. Pay close attention to details. Do sample questions. Study wrong answers and list the reason for the incorrect answer. Review the test. Check correct answers.
Wilfong, D., Szolis, C., & Haus, C. (2007). Nursing school success: Tools for constructing your future. Jones & Bartlett Learning.
Essay questions require different preparation and skills. You need to have a greater in-depth understanding of the content to respond to an essay question. Some questions may ask for opinions. In all cases, it is important that your answer is clear and concise, provides rationales, includes content relevant to the question and to the material covered in the course, and presents the response in an organized manner. This requires that you read the question carefully and make sure you understand it. Sometimes, the exam directions may provide guidelines as to the length of response expected, but in many cases, this must be judged according to what is required to answer the question. The amount of space provided on the exam may or may not be a good indication. Grammar, spelling, and writing style are also important. Jotting down a quick outline will help you to focus your response and manage your time during the exam. It is important for you to review the essay response to make sure the question (or questions) has been answered. As is true for all types of exams, you must pace yourself based on the allotted time for essay questions and other types of exam questions. Spending a lot of time on questions that may be difficult is unwise. You can return to difficult questions and should keep this tactic in mind when managing time during the exam.
Participating in Team Discussions
Nursing courses often include team discussion in the classroom and/or online. You need to focus on the assignment requirements, such as the questions to consider. These are critical learning experiences that allow you to apply content; use critical thinking, clinical reasoning, and judgment; and develop communication and teamwork skills. Faculty may assign students to small teams to analyze and discuss cases in the classroom or work on projects in and outside the classroom. You may work with the same team throughout the course or work with a team for a specific assignment; sometimes, multiple teams may work together. Why is this not called group discussion? Nurses are members of teams in healthcare settings, not members of groups. Students need to think of themselves as team members and consider how they participate in teams and teamwork in the classroom or during e-learning experiences, simulations, and clinical experiences. The critical factor with these experiences is each student must feel responsible for the work that needs to be done in these learning activities, which may and often does include preparation prior to the experience, such as reading assignments or researching for more information. During the experiences, all students on the team should be actively engaged in the activity.
Effective Engagement in E-Learning
Engaging in e-learning requires many of the same approaches as a traditional classroom, but there are also differences. Class attendance is important, especially in courses that use active student learning methods. Students are expected to participate in course discussions and activities. Expectations for discussions are described in the criteria provided by the faculty.
The following are some guidelines, but it is also important that students follow specific course guidelines provided by their faculty and school.
- In e-learning courses delivered solely on the internet, you are guided through various activities designed to assist you in meeting the course learning objectives/outcomes. The course is not an independent study and requires you to meet certain objectives per week and interact with faculty and other students routinely. Modules may include reading assignments from a variety of resources, reviewing websites, or collaborative and individual learning activities, including written papers. You are expected to keep track of due dates (be aware of time zones if this is a relevant factor; for example, you live in a different time zone from your school's location) and participation requirements, so keep a detailed schedule and work plan.
- It is important to get oriented to the technology used by your school prior to the course start date.
- Review the faculty information for contacting the faculty.
- Keep the information for contacting tech support handy. If you have problems, contact them. If this is not helpful, inform the faculty. If a tech issue will delay the required participation or submission of an assignment, contact your faculty, even if this means calling the faculty. Keep notes on any tech issues.
- Follow any required policies and procedures related to computer security.
- Follow Health Insurance Portability and Accountability Act (HIPAA) requirements when posting information. (See other content in the text on HIPAA and patient confidentiality and privacy.)
- Communication using internet tools increased the need for a protocol called “netiquette” that encourages respectful, efficient, and effective communication while discouraging abuse of email, chat sessions, and message boards and inappropriate communication. Professional communication is expected in all forms of communication.
- You are responsible for all information you post on the course site.
- Note the course and school policy regarding cancellation of classes, which may be different from traditional courses.
- Look over the course schedule, which provides an overview of each module, to understand what is required. Review the syllabus. Make a copy of the schedule to guide your work.
- Get acquainted with your assigned discussion team and complete the orientation assignment to get to know one another.
- Complete the assigned readings and apply as needed in discussions and assignments.
- View the presentation slides and/or lecture content and handouts that accompany the modules. Slides may have audio. Some courses have live lectures, so you need to note the times you must be online to attend.
- Participate actively in the online discussion and engage other team members in the discussion.
- Review criteria for assignments and follow them. (This is your checklist for the assignment.) Complete all assignments by the due date/time. It is important to note time zones in case you are in a different time zone from the faculty or school-typically, due dates include a time in addition to a date.
- Contact faculty whenever you have questions. For some e-learning, it is not possible to meet face-to-face with faculty. You are expected to inform your faculty of any problems that you may have with the course or problems you have that might interfere with your meeting course requirements. This should be done in a timely manner so that questions can be addressed and, if needed, a plan developed so that you can successfully complete this course.
- You will be working in teams for discussion and other assignments. Typically, for these courses, all the work can be done virtually-you do not have to meet in person. All students are also expected to participate actively in their assigned teams. Individual grades are received for participation and for discussion assignments. For all discussions, all students are expected to respect one another and the ideas proposed and use appropriate feedback communication.
| Stop and Consider 4 |
|---|
| Trying out different tools for success in learning may lead you to greater success. |
Clinical Learning Experiences
As a student begins a nursing program, it usually quickly becomes clear that nursing programs are different from past learning experiences. Students need to develop competencies to provide quality care to patients, families, communities, and populations. Nursing education uses not only traditional didactic learning experiences, which may be offered through face-to-face classes offering didactic/theory- or content-focused experiences, but also clinical experiences in clinical and simulation labs and clinical experiences in healthcare settings (practicum). What does this mean to you as a student?
Clinical Lab and Simulation
Schools of nursing use a variety of methods for developing student clinical competencies. A competency is an expected behavior that you must demonstrate. Two methods used to develop clinical competencies that have become common in nursing education are the clinical laboratory (lab) and simulation learning, which is often combined with the lab experience. The simulation lab is a learning environment that is configured to look like a hospital or other type of clinical setting and provides structured learning experiences. The lab may take the form of a hospital room, a room with multiple beds, or a specialty room, such as a procedure room or operating room. It contains the same equipment and supplies that are used in a healthcare setting, typically a hospital. Some schools have a simulation area that looks like a patient's home so that students can practice home health care prior to an actual home visit or a clinic. The clinical lab is typically not configured to replicate a clinical setting in the same way as a simulation lab; although it will have some of the same equipment, it typically does not use high-level equipment, such as a simulation manikin or trainer. Some schools have only one type of lab-that is, a lab for developing basic nursing skills-with less opportunity for more complex learning in a simulated environment.
Students are assigned specific times in the lab as part of a course. Some didactic content may be delivered prior to the lab experience. Students are expected to come to the lab prepared (for example, having completed a reading assignment, viewed a video, or completed online learning activities). Preparation makes the lab time more effective, and well-prepared students will be better able to practice applying what they have learned. To succeed in this setting, students need to be motivated and self-directed learners. (This is true for any learning experience in the nursing program.) Schools have different guidelines about dress and behavior in the lab. In some schools, the lab is treated as if it were an actual clinical setting/agency with certain dress and behavioral expectations, such as wearing the school uniform or a lab coat and meeting all other uniform requirements related to appearance and professional behavior in the clinical setting.
Simulated-based education (SBE) is an effective method to develop clinical competency and is used for nursing students' educational experiences at all levels-prelicensure and graduate (NLN, 2022). This method is supported by research and positive outcomes, but nursing programs must consider quality, time, and costs as they develop, implement, and evaluate SBE. Some nursing programs, in addition to using complex simulation manikins and equipment, have expanded their simulation experiences to include human role players (Cowperthwait, 2020). This provides a more engaging experience for students but requires preparation of the human role players/standardized patients or actors so that they provide realistic experiences as they role play patients based on a script. SBE provides students with as near-to-life experience as possible without patient risk. Levels of simulations vary, ranging from low fidelity to high fidelity (use of more complex equipment). The key difference between levels is how close the simulated scenario comes to reality (Jeffries & Rogers, 2007). Simulation may also involve task trainers for learning skills, such as IV insertion.
Practice is important, but guided practice is even more important, and ideally, this should be risk free. Practicing on a real patient always carries a risk. It is not realistic to expect that a student will be able to provide care without some degree of potential harm. For this reason, practicing in a setting without a real patient allows students to develop competence and gain self-confidence. What does the student learn in the simulation experiences? Most procedures and related competencies, such as health assessment, wound care, catheterization, medication administration, enema, general hygiene, safe patient mobility, infection control, and much more, can be taught in a lab. Complex care may also be practiced in the simulation lab setting using teams of nursing students, such as trauma care post-surgery procedures.
Simulation also allows faculty to design learning experiences that meet a variety of learning styles-visual, auditory, tactile, or kinesthetic-and give students time to incorporate their learning with real-time and postactivity feedback and interact with different students and situations. Time is also allocated to discuss the care provided without concern for additional care that needs to be provided, as would occur in a clinical setting. This type of debriefing is an important component of the simulation experience. During a simulation, students may work alone, with faculty, and with other nursing students, as well as with other healthcare professional students in an interprofessional team. Faculty can better control the types of experiences in which students engage, whereas, in the clinical setting, it is not always easy to find a patient who needs a specific procedure or has certain complex care needs at one time. Simulation is an active learning method, which helps the student improve critical thinking/clinical reasoning and judgment (Billings & Halstead, 2020). Some schools have developed interprofessional simulation experiences that involve medical, pharmacy, respiratory therapy, and other healthcare professional students. These experiences are very important and improve interprofessional teamwork. This also supports the healthcare core competencies that apply to all healthcare professionals (IOM, 2003) and supports the nursing education standards (AACN, 2023a; CNEA, 2021).
Clinical Practice Experiences or Practica
Clinical experience or practicum is part of every nursing program. This experience occurs when students, with faculty supervision, provide care to patients. Such care may be provided to individual patients or to their families or significant others (for example, providing care to a patient after surgery and teaching the family how to provide care after discharge), to communities (for example, working with a school nurse in a community), or to specific populations (for example, developing a self-management educational program for a group of patients with diabetes). Some nursing programs begin clinical experiences early in the program curriculum and others later, but all programs must have clinical practica. In addition, many nursing courses include a clinical or practicum component, or they may have no didactic component and only a clinical focus. A student might think that these courses are equivalent to a chemistry lab, but this is not a fair comparison. A nursing clinical experience/practicum usually includes several hours per session and, in some cases, can require 8 to 12 hours several days each week. Students must prepare for these experiences and participate in the experience for the designated hours as students. Faculty members are available to guide student learning, and in some situations, students are assigned to preceptors who are nurses working in the HCO. Students participate in clinical experiences in a variety of clinical settings, such as hospitals, clinics, homes, and community settings, such as schools, public clinics, worksites, and so on.
Typically, the practicum is conducted in blocks of time-for example, students are in clinical practice 2 days a week for 6 hours each day for one course. Faculty may be present the entire time or may be available at the site or by telephone. The amount of faculty supervision depends on the level and competency of the student, the type of setting, and the objectives of the experience. The clinical setting may also dictate the student-faculty ratio and supervision. Settings are highly variable in their requirements, and the types of patient experiences are provided-a hospital, clinic, physician's office, school, community health service, patient home, rehabilitation center, long-term care facility, senior center, child day-care center, or mental health center, and others. Some experiences require that a student is with a group of students; in others, a student may be alone with staff. In the latter case, for example, a student may be assigned to work with a school nurse or with a preceptor in the intensive care unit.
Participating in clinical experiences requires preparation. For many assigned experiences, you may need to go to the clinical practicum site before the clinical day begins (sometimes the day before) to obtain information about your preassigned patient(s) and plan the care for the assigned time. This is done so that you are ready to provide care. You need to understand the patient's history and problems, laboratory work, medications, procedures, and critical care issues and plan care effectively. Often, the student develops a written plan-perhaps in the form of a nursing care plan that is evaluated by faculty. Students who arrive at clinical care settings unprepared will likely be unprepared to meet the requirements for that day. Typically, the clinical day begins with a short preconference where faculty may highlight goals for the day's experience, and students may introduce their assigned patients by sharing information. The clinical experience ends with an in-depth postconference to discuss the experiences and outcomes, offering opportunities for debriefing and for students to share and learn from a variety of student experiences. In some clinical situations students may attend or participate in nursing team care meetings.
Sometimes, students are assigned an observation experience in a clinical setting. In this case, the student does not participate in the care provided but observes care that is provided by qualified staff. If the student knows about the observation ahead of time, the student should prepare by reviewing relevant information. During the observation, the student should note factors, such as patient information, what was done, team member roles and communication, quality care, and so on. Time should be provided to discuss the observation or other methods should be used to report on the observation, such as a written summary. These are important learning activities allowing students and faculty to reflect on content and application in practice. Student responses to observation experiences can also be shared in online team discussions so that students can learn from one another and expand their experiences. As required for all sharing of information, students need to consider patient and staff privacy and confidentiality during these discussions.
Another important aspect of clinical experiences relates to professional responsibilities and appearance. When a nursing student is providing care, the student is representing the profession, which is pertinent to the content in this text about the image of nursing. The student needs to meet the school's uniform requirement for the assigned experience, be clean, and meet safety requirements (such as the appearance of hair) to decrease infection risk-for example, washing hands as required. Students who go to their clinical experience site and do not meet these requirements may be sent home. Making up missed clinical experiences is very difficult and, in some cases, impossible because it requires reserving a clinical site again and securing faculty time, student time, and so on. Minimizing absences is critical; however, if the student is sick, the student should not care for patients. Schools have specific requirements related to illness and clinical experiences that should be followed. You should show up for every clinical experience dressed appropriately, prepared, and with any required equipment, such as a stethoscope. In addition, you need to be on time-set your alarm to allow plenty of preparation time and plan for delays in traffic. All this relates to the practicing nurse: Employers expect nurses to come to work dressed as required, prepared, and on time. The COVID-19 pandemic increased the need for students to use personal protective equipment (PPE) in some situations and use masks. If use is required for patients with communicable diseases or there is a risk for these diseases, students need to be provided with the equipment, taught how to use the equipment, and follow the guidelines provided by faculty and clinical staff.
Students need to recognize that when they are in clinical, they should practice at their expected education level and respond in a professional manner. Faculty expects this as do staff. Family view students as part of the healthcare team and expect the faculty and staff to supervise students. Students should ask for help when they are in situations where they do not feel comfortable. A critical factor with students is communication at times of patient transition or handoffs, a topic discussed further in quality improvement content. Students are responsible for sharing information with staff just as the staff is responsible for providing information the students need to care for patients.
| Stop and Consider 5 |
|---|
| Your preparation for clinical experiences makes a difference in your learning. |
Additional Learning Experiences to Expand Graduate Competency
When students approach their first nursing job after graduation, many experience reality shock. This is a shock reaction that occurs when an individual has attended a nursing education program in which one view of nursing is emphasized, and then a new nurse encounters a different view of nursing in the practice setting (Duchsher & Windey, 2018; Kramer, 1985). Not all new graduates experience reality shock, but many do. One strategy that can prevent reality shock is developing better stress management techniques during the nursing education experience. This will not make the difference between your clinical experience and the real world of work completely disappear, but it will help the new graduate cope with this change in roles and views of what is happening in the healthcare delivery system. Another method that helps with adjustment later after graduation is discussing clinical situations with faculty that seem out of sync with what should be done in practice. Faculty should be used as resources to openly discuss your concerns and to learn from these experiences. Concern about reducing postgraduate stress as one transitions to practice and professional nursing has led to an increasing number of HCOs creating externship/internship and residency programs to guide students and new graduates through the first year of transition to practice. Some schools of nursing have also developed cooperative learning experiences for their students. Nursing, unlike medicine, pushes its “young” out of the nest without the safety net of a residency period (Goode et al., 2009). Some of these newer methods may assist with this problem are described in the next section of content.
Cooperative Experiences
Some schools of nursing offer cooperative (co-op) experiences during the nursing program. These experiences are not common and vary in their design. This program allows students (or even requires students) to take a break from courses and work in healthcare settings. Students receive guidance in job searches, résumé development, interviews, and selecting the best experience. Some schools maintain lists of HCOs that students often use to identify co-op programs. A co-op experience typically means the student is hired by the HCO for several months and functions in an aide or assistant position supervised by RNs.
Nurse Internships/Externships
Students frequently want more clinical experiences in the summer, when many schools of nursing do not offer courses, and they also want to be employed. The nurse internship/externship is a program that offers this type of opportunity for students. Students are often concerned about their upcoming first job as a nurse. They wonder if they are ready, and this type of experience can help students later as they adjust to their first RN positions. Nurse internships/externships are available in some communities as opportunities sponsored by hospitals (Meeker, 2022). These programs are not usually associated with a school of nursing. They are short programs, such as 10 weeks, usually offered in the summer for students who will enter their senior year in the fall. There is variation in the length of these programs, in what is offered to the student in the program, and in how much support the student receives in the program. The student is employed by the hospital and provided with an orientation to the hospital, some content experiences, and preceptor and/or mentor experiences. Students need to investigate these programs and find out what each program offers and whether it meets their needs. This type of program is particularly helpful if students want more time in an HCO to determine if they want to work in the HCO after graduation.
Nurse Residency Programs
Because of concern about nursing staff turnover, replacing nurses who leave, and other job-related issues, such as staff burnout and concern about the level of new graduate preparation and retention, some hospitals have developed nurse residency programs (Knighten, 2022). After the new graduate passes the licensure exam, the residency program offers the new nurse a structured transition to professional nursing practice.
The American Association of Colleges of Nursing (AACN) conducted a pilot program to examine the use of a national accreditation program based on standards it developed for nurse residency programs. The Vizient/AACN Nurse Residency Program offers a structured approach for HCOs to develop and maintain nurse residency programs (AACN, 2023b, c). In 2022, this residency program included 32,000 nurse residents in 650 sites, representing 47 states. The program is integrated with an HCO orientation, can be customized as needed, and emphasizes staff satisfaction, quality care (efficiency and safety), reducing staff turnover, teamwork, patient satisfaction, decision-making and evidence-based practice, leadership, professional development, and more. Nurse residency programs should have a designated staff person to lead the program to ensure that it is effective-using planning, implementation, evaluation, and collaboration (Windey et al., 2018). Often, this staff member is part of the nurse professional development team/department as they work to provide an environment in which new graduates can transition to their new role. Both The Future of Nursing report (Institute of Medicine [IOM], 2011) and Benner and colleagues' nursing education report (Benner et al., 2010) recommended residency programs as a standard part of nursing education, although at this time, they are not required. The progress report for The Future of Nursing report also supports the need for more residency programs in acute care and also in public/community care and continues to support this need in a later report (National Academy of Medicine [NAM], 2016; 2021).
Nurse residents are in paid positions, and typically, the nurse resident must commit to working a specified period for the HCO after completion of the residency. Such programs are helpful for new nurses and decrease new graduate turnover, improving staff retention. However, not all hospitals have residencies, and admission to these programs is competitive. Most programs are in acute care, but with the increasing need to attract staff to public and community health and improve these nursing services and the experience of the COVID-19 pandemic that highlighted weaknesses in public health, some residencies are now offered for these services (Manske, 2022).
Some HCO residency programs partner with schools of nursing-a relationship recommended by the AACN residency standards, which focus on leadership, patient safety outcomes, and professional development (AACN, 2023a). In the first 6 years of the implementation of the AACN's residency program, the organization established 62 sites in 30 states, and more have been added since that time (AACN, 2023a, 2023b). These programs can receive accreditation from the AACN.
Students who are interested in a residency experience need to investigate these opportunities in their junior year or early in their senior year. Only baccalaureate degree in nursing (BSN) graduates can participate in residency programs that follow the AACN residency model, but some other residency programs do not require a BSN and are open to associate degree in nursing (ADN) graduates. These programs usually encourage new ADN graduates to consider completing a BSN degree.
Transition-to-practice programs, such as internship and residency, emphasize the need to reduce stress for new nurses as they transition to practice, reducing reality shock. A systematic review of studies focused on this type of program was conducted (Weller-Newton et al., 2022). The review indicated that there is mixed evidence supporting the success of these programs due to inconsistencies across clinical settings, organizations, and preceptorship/mentoring training as per sites in the samples. Two factors that were notable were the program's length and the amount of formal contact or study days in the program. This indicates that we need to know more about these programs and outcomes and improve them when needed. This requires feedback from nurse residents and HCOs as well as from nursing education. It is also important since we now have residencies in acute care and in public health, that we understand similarities and differences in these programs and ensure effective outcomes based on the practice area.
Networking and Mentoring
Professional nurses use networking and mentoring to develop themselves and to help peers. Consequently, you need to understand what these activities offer and begin to work toward using networking and mentoring.
Networking is a strategy that involves using contacts that might be helpful to you professionally. Applying networking effectively is a skill that takes time to develop. Nurses typically use networking at professional meetings. You can begin to network in student organizational activities, whether local, statewide, or national. Networking allows a person to meet and communicate with a wide variety of people, exchange ideas, explore new approaches, and obtain information that might be useful. Examples of networking skills are knowing how to meet new people, approaching an admired person, learning how to start a conversation and keep it going, remembering names, asking for contact information, and sharing because networking works both ways. Networking can take place anywhere: in school, in a work setting, at a professional meeting or during organizational activities, and in social situations. It can even happen online using social networking media and other digital methods, but you must be careful with what is communicated and how-today, information can become public very quickly, and once public, it is difficult to change it or delete it.
Mentoring is a career-development tool. A mentor-mentee relationship cannot be assigned or forced. A mentor is a role model and a career advisor. The mentor should not have a formal relationship, such as a supervisory or managerial relationship, with the mentee. This type of mentorship could cause stress and not allow the mentor and mentee to communicate openly without concern about possible repercussions; however, there may come a time when a past supervisor becomes a mentor to a former employee. The mentee needs to feel comfortable with the mentor and usually chooses the mentor. The mentor, of course, must agree to be part of this relationship. A mentorship can be short term or long term. It does take time to develop the mentor-mentee relationship. Today, such a relationship could occur virtually, expanding options.
When entering a nursing education program, you might think about acquiring a mentor, yet not know when a possible mentor might be met. Be alert for possible future mentors as you interact with nurses. The mentor may be a nurse who works in an area where a student has clinical experience/practicum. New graduates can benefit from a mentorship relationship to help guide them in early career decisions. Mentors can provide constructive feedback about a new graduate's strengths and limitations and suggest improvement strategies. The mentor does not make decisions for the mentee but rather serves as a sounding board to discuss options and allow the mentee to benefit from the mentor's expertise. In this way, the mentor acts as a guide and a teacher. An effective mentor has the following characteristics:
- Expertise in an area related to the mentee's needs and interests
- Honest and trustworthy
- Professional
- Supportive
- Effective communicator
- Teacher and motivator
- Respected and influential
- Accessible
| Stop and Consider 6 |
|---|
| Nurse residency programs might be a good choice for you. Why might you consider a residency? |
Continuing Professional Development
Engaging in ongoing learning or continuing professional development (CPD) is one of the major characteristics of a professional. This model of learning includes three major components:
- Academic education: The courses students take for academic credit-undergraduate and graduate-in an institution of higher learning that typically leads to a degree or completion of a certificate program. Nurses who return to school are pursuing lifelong learning goals.
- Staff education: The systematic process of assessing and developing oneself to enhance performance or professional development-continued competence. Staff education includes orientation (the process of introducing nursing staff to the organization and position), training required to do a job guided by the employer's educational needs for staff, and relevant responsibilities to ensure quality, safe care, and professional development.
- Continuing professional development: Systematic professional lifelong learning designed to augment knowledge, skills, and attitudes.
The Association for Nursing Professional Development (ANPD) is the organization that supports nurses who provide staff development/education to advance quality health care by defining and promoting nursing professional development practice (ANPD, 2023). Nursing professional development standards guide the work that is done to ensure staff in practice is prepared (Harper & Maloney, 2022; ANA, 2021).
As a student, you may wonder why lifelong learning is important to you when you are just now entering nursing education. Lifelong learning, or CPD, begins when you enter a nursing education program. Students often have opportunities to participate in some of these learning activities, even as students. These professional educational activities are excellent opportunities to gain further knowledge and better understand the importance of lifelong learning. You also need to know the requirements for continuing education (CE) in the state(s) where you wish to apply for licensure. Continuing professional development must be driven by personal responsibility to improve. Although professional organizations, regulatory agencies, and employers influence whether nurses participate in lifelong learning, successful learning is ultimately in the hands of the learner-that is, the individual nurse. The major report on nursing from the IOM (2010) included the recommendation that the profession ensure that nurses engage in lifelong learning or CPD, which is the current term for this learning. In addition, a major report focused on collaboration between nursing and medicine examined the need for a clearer vision for lifelong learning for nurses and physicians (Sullivan, 2010). The report's recommendations focused on four areas that continue to be relevant: CE methods (for example, meetings, rounds, conferences, and so on), interprofessional education, lifelong learning, and workplace learning. Interprofessional education is mentioned in other content in this text about academic nursing education; however, it is also relevant to CPD. If different professions can continue to learn together after completion of academic programs, this can be supportive of interprofessional collaboration, teams, and understanding the roles and responsibilities of other professions. This report also discusses an issue about CPD regulation that is not often addressed. There is great variation among professions, and even within a profession, such as different state boards of nursing have different requirements for CPD, and accreditation of CPD varies. This needs to be improved because it is confusing and does not promote consistent views on healthcare professional ongoing education.
The natural assumption is that all nurses would want to get more education and stay current, but this is not necessarily the case. Required ongoing education is a great motivator. Many states require CE/CPD courses if nurses are to maintain their licensure after initial licensure is received. In these states, the state board of nursing designates the number of continuing education units (CEU) or credits required for licensure renewal. States vary in terms of what is considered learning experiences for CEU-short, structured programs, often online; academic courses; attending conferences where educational content is presented; publishing; and so on. Nurses must follow their state's licensure requirements. Another reason for obtaining CEU is to meet some specialty certification requirements. The certification body determines the amount and type of required CEU. If a nurse is licensed in more than one state, then the nurse must meet the CEU requirements for all states in which the nurse is licensed, even if the requirements are different.
Approved sources for CEUs are highly variable. Credit can be obtained, for example, by attending a 1-hour or full-day educational offering, attending part or all of a conference, reading an article in a professional journal and then taking an assessment quiz, or participating in an online program. Typically, a fee is charged unless the costs for the program are covered, such as by a grant to the sponsoring organization. Nurses need to be careful and make sure that the education program's credit is accepted by the organization requiring the CEU, so it is best that the CEU comes from accredited programs. The American Nurses Credentialing Center (ANCC) accredits these programs, and some state boards of nursing may offer an accrediting process. Obtaining accreditation is voluntary, but the reality is to get nurses to participate, accreditation is critical. When a CEU program is accredited through an organization such as ANCC, the consumer is assured that national standards of quality education have been applied (ANCC, 2023a). It is assumed that completing CEUs has an impact on patient outcomes and quality care, but this relationship is not easy to prove in a consistent manner. When nurses select CPD programs to attend or complete, they should evaluate the following factors:
- Accreditation of the program
- Acceptance of the CEU by the required body, such as a state board of nursing for licensure or an organization sponsoring certification
- Number of CEU credits and related time commitment
- Schedule and location, including travel
- Cost (registration fee, parking and travel, housing, and meals)
- Qualifications of faculty
- Adult learning principles applied
- Identification of learning needs
- Program's learner objectives
- Use of current and relevant content
- Teaching methods
- Past experiences with the provider of the educational program
- Receipt of documentation of completion with the title of program, sponsoring organization, date, and hours identified
Nurses are responsible for maintaining their own CEU activity records. In states where CEU is required for licensure renewal, nurses may be required to produce documentation of these activities. In addition, nurses need to update their résumés to ensure that learning activities are included. In some cases, employers require documentation of CEU activities, requiring nurses to document learning activities on an annual or biannual basis.
A current CPD issue is the need for greater emphasis on interprofessional CEU to increase support for more interprofessional teamwork. The issue is addressed in a major report, which recommends that a national system be developed to support interprofessional CE: “The current system of continuing education for health professionals is not working. Continuing education for the professional health workforce needs to be reconsidered if the workforce is to provide high-quality health care. A more comprehensive system of CE is needed, and CPD provides a promising approach to improve the quality of learning. An independent public-private Continuing Professional Development Institute will be key to ensuring that the entire health care workforce is prepared to provide high quality, safe care” (IOM, 2010, p. 3). As a follow-up to these proposals, in 2013, CEU accreditor organizations for nursing, pharmacy, medicine, and other healthcare professions met together to discuss interprofessional continuing professional education (IPCE, 2023). Participants in this meeting identified goals, including creating standardized terminology and exploring a shared set of expectations and measures for interprofessional education in support of collaborative practice (ACCME, 2024).
| Stop and Consider 7 |
|---|
| Even after you complete your nursing degree and receive your registered nurse license, you need to continue learning. |
Certification and Credentialing
Certification and credentialing are recognition programs that identify whether nurses meet certain requirements or standards. These recognitions may be required or voluntary, depending on the circumstances. Credentialing is typically required, whereas certification may be voluntary. To obtain certification or meet credentialing requirements, nurses must first be licensed as RNs.
Credentialing is a process that ensures practitioners, such as RNs, are qualified to perform as demonstrated by having licensure (ANCC, 2023a). Typically, it is used by HCOs to check if healthcare professionals (such as nurses, physicians, and so on) are licensed in the state to practice and to monitor continued licensure. Nurses are required to show their current license to their employer, and the employer may then keep a copy of the license. States provide access to online checks of licensure status. Education, certification, and maintenance of malpractice insurance may also be reviewed, although this practice varies from one HCO to another. The goal is to protect the public by ensuring that specific state requirements are met.
The ANCC provides nongovernmental certification that “enables nurses to demonstrate their specialty expertise and validate their knowledge to employers and patients. Through targeted exams that incorporate the latest clinical practices, ANCC certification empowers nurses with pride and professional satisfaction” (ANCC, 2023b). It is a method for recognizing expertise through the successful completion of an exam focused on the certification specialty, recognition of completed education, and the description of clinical experience in a designated specialty area covered by the certification. Certification of nurse practitioners in the areas of adult, family, and adult-gerontology primary care is managed through the American Academy of Nurse Practitioners Certification Program (AANPCP). Other specialty nurse practitioner certifications are managed through different organizations. Pursuing this type of recognition is voluntary, with nurses not required to have certification, but many employers acknowledge its importance, and some may require certification for certain positions-for example, for advanced practice registered nurses (APRNs). This recognition is now available in most specialty areas. The ANCC offers certification in multiple nursing specialties. After a nurse receives the initial certification, recertification is accomplished through demonstrating ongoing practice and through CPD. Nurses may be certified in multiple areas if they meet the requirements for each area. Professional certification in nursing is a measure of distinctive nursing practice, and the benefits of certification are widely accepted. The value of certification is not just significant for nursing practice, but a focus on professional certification is also essential to meet multiple standards within the ANCC's Magnet Recognition Program® for excellence in nursing services (ANCC, 2023c). Certification may also be given by an HCO for accomplishing a specific competency goal, such as learning to perform cardiopulmonary resuscitation, but this is not the same type of certification that is awarded after meeting specific professional standards described previously.
The nursing profession developed and implemented a consensus model for regulation that includes licensure, accreditation, certification, and education to ensure greater consistency and clarity for APRN practice (NCSBN, 2023b; ANA, 2023a). This model reflects ongoing concern about the need for uniformity in educational requirements and regulations related to APRNs, easing mobility across state lines to practice. Over time, there will be changes in the various approaches for ensuring competency, and this process of reviewing and improving the approaches requires active engagement from nurses.
| Stop and Consider 8 |
|---|
| Certification recognizes specialty nursing. |
Caring for Self
Caring for others is clearly the focus of nursing, but the process of caring for others can be a drain on the nurse. Students quickly discover that they are very tired after a long day in their clinical sessions. The number of hours and the pace of clinical experiences affect staff fatigue, but stress also has an impact. When you graduate and practice, you may find that this stress does not disappear, and, in some cases, it may increase, particularly during your first years of practice. Nurses often feel that they must be perfect. They may feel guilty when they cannot do everything they think they should be doing, both at work with patients and in their personal lives. There is still much to learn about nursing, working with others, pacing oneself, and figuring out the best way to mesh a career with a personal life-finding a balance and accepting that nursing is not a career of perfection.
Learning how you routinely respond to stress and developing coping skills to manage stress can have a major impact and, it is hoped, prevent burnout later. Symptoms such as headaches, abdominal complaints, anxiety, irritability, anger, isolation, and depression can indicate a high level of stress. A review of anatomy and physiology explains how stress affects the body. When you experience stress, two hormones-adrenaline and cortisol-trigger the body to react and put the nervous, endocrine, cardiovascular, and immune systems in a state of alert. This physiological process is helpful because it improves coping with stress. The problem may increase when these stress responses happen frequently and over a period of months or years. Stress can be felt from a real or imagined threat, and the stressed person feels powerless. Exposure to constant or frequent stress may lead to chronic stress, which may have an overall impact on a person's health.
The National Institute of Occupational Safety and Health (NIOSH) provides support for employees, including nurses, to ensure a safe and healthy work experience for employees in the United States. Figure 4-6 describes a model of job stress. Six factors generally impact job stress in a variety of settings and influence this model (Health and Human Services [HHS], Centers for Disease Control and Prevention [CDC], NIOSH, 2014):
Figure 4-6 Model of job stress.
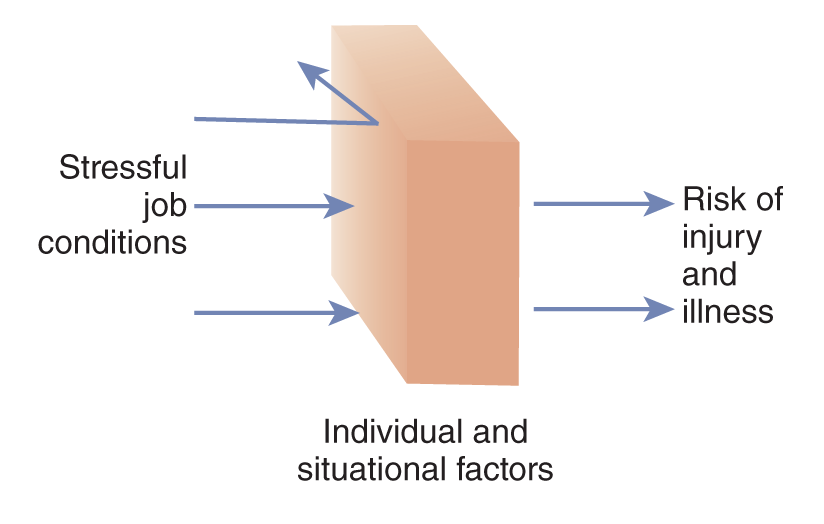
A model illustrates how stressful job conditions can lead to a higher risk of injury and illness, influenced by individual and situational factors.
U.S. Department of Health and Human Services (HHS). Centers for Disease Control and Prevention (CDC). National Institute of Occupational Safety and Health (NIOSH). (2014). STRESS . . . At Work. http://www.cdc.gov/niosh/docs/99-101/default.html
- Design of tasks: Aspects to consider are work hours, heavy workload, frequency of breaks, shift work, lack of routine and increased hectic work environment, feeling of loss of control when required to do tasks, and so on
- Management style: Lack of staff input into decisions, poor communication, lack of clear policies, and so on
- Interpersonal relationships: Poor social environment and communication, lack of support, and so on
- Career concerns: Job insecurity, lack of advancement, changes in staff and management, and so on
- Environmental concerns: Risky work environment, high levels of noise, air pollution, ergonomic risk, and so on
Nurses are at greater risk for stress when they experience work overload, time pressure, lack of social support, staff incivility, exposure to infectious diseases, risk of needlestick injuries, exposure to work-related violence or threats, sleep deprivation, role ambiguity and conflict, understaffing, career development issues, and need to care for difficult or seriously ill patients (HHS, CDC, NIOSH, 2014).
The best time to begin stress management is now, while you are still a student. Strategies for coping with stress can be found in a great variety of resources. Exhibit 4-2 identifies some websites that provide general information about stress. The following are some guidelines that can prevent and/or reduce stress:
| Exhibit 4-2 Links to Help You Cope With Stress |
|---|
|
- Set some goals to achieve a work-life balance.
- Use effective time-management techniques and set priorities.
- Prepare ahead of time for assignments, quizzes, and exams.
- Ask questions when confused and ask for help-do not view this as a sign of weakness but rather a strength.
- Take a break-a few minutes of rest can do wonders.
- Get an appropriate amount of exercise, sleep, and a healthy diet. (Watch excessive use of caffeine.)
- Practice self-assertion.
- When you worry, focus on what is happening rather than what might happen.
- When you approach a problem, view it as an opportunity.
- Use humor.
- Set aside some quiet time to just think-even a short period can be productive.
Nurses experience burnout and compassion fatigue, and these experiences might be described as the costs of caring and directly related to the need to effectively manage stress. They are similar but have some major differences. They lead to similar difficult physical and emotional responses and affect quality of care and staff retention.
Burnout occurs when assertiveness-goal achievement intentions are not met, and compassion fatigue occurs when rescue-caretaking strategies are not successful (Peters, 2018). Burnout is often a reaction response to work stressors, such as staffing, workload, managerial style, staff behavior, and so on, and occurs gradually. All nurses need to be aware of the potential for burnout, which is caused by unmanaged, chronic workplace stress and can lead to emotional exhaustion, depersonalization, and reduced personal accomplishments. Burnout is very common among nurses-results from a 2020 survey indicate that almost two-thirds of nurses (62%) experience burnout. It is especially common among younger nurses; 69% under 25 experience burnout (ANA, 2023b). A recent study indicated that nurse burnout continues to be a significant problem (Shah et al., 2021). It impacts healthcare quality and staff and patient safety; increases staff turnover with related job dissatisfaction; reduces productivity; increases healthcare costs, such as the use of more referrals and tests; increases staff turnover costs related to recruitment and orienting new staff; and impacts personal consequences for staff-their mental and physical health, including substance abuse and suicidality and personal relationship issues. Another study noted that in its sample, 1 in 10 nurses worldwide indicated they experience burnout (Aoyjai et al., 2021). The same study concluded that nurse burnout is a significant factor in predicting medication administration errors. There needs to be more research on staff burnout to better understand it and develop strategies to prevent it and, when it occurs, respond effectively (Dyrbye et al., 2017). For example, nurses need to be aware of their work-life balance, which is “a state where the needs and requirements of work are weighed together to create an equitable share of time that allows for work to be completed and a professional's private life to get attention” (Heckerson & Laser, 2006, p. 27).
Burnout is often considered a characteristic of an unhealthy work environment that is stressful and may be characterized by disruptive or uncivil staff behavior and lack of staff well-being. The nurse may reach the point of not wanting to go to work and have difficulty completing work and working with others (Shah et al., 2021). In a systematic review of 27 studies that measured staff well-being and patient safety, it was noted that in 16 of the studies, there was a significant correlation between reduced staff well-being and risk to patient safety (Yellowlees & Rhea, 2022). This is important information because it demonstrates that staff status (burnout, well-being, stress levels, compassion fatigue, and so on) affects performance, which also affects patient outcomes, such as safety, and, ultimately, quality of care. The HHS notes in a special report that burnout has negative consequences on patients, as described in Figure 4-7.
Figure 4-7 Healthcare Worker Burnout Can Have Negative Consequences.
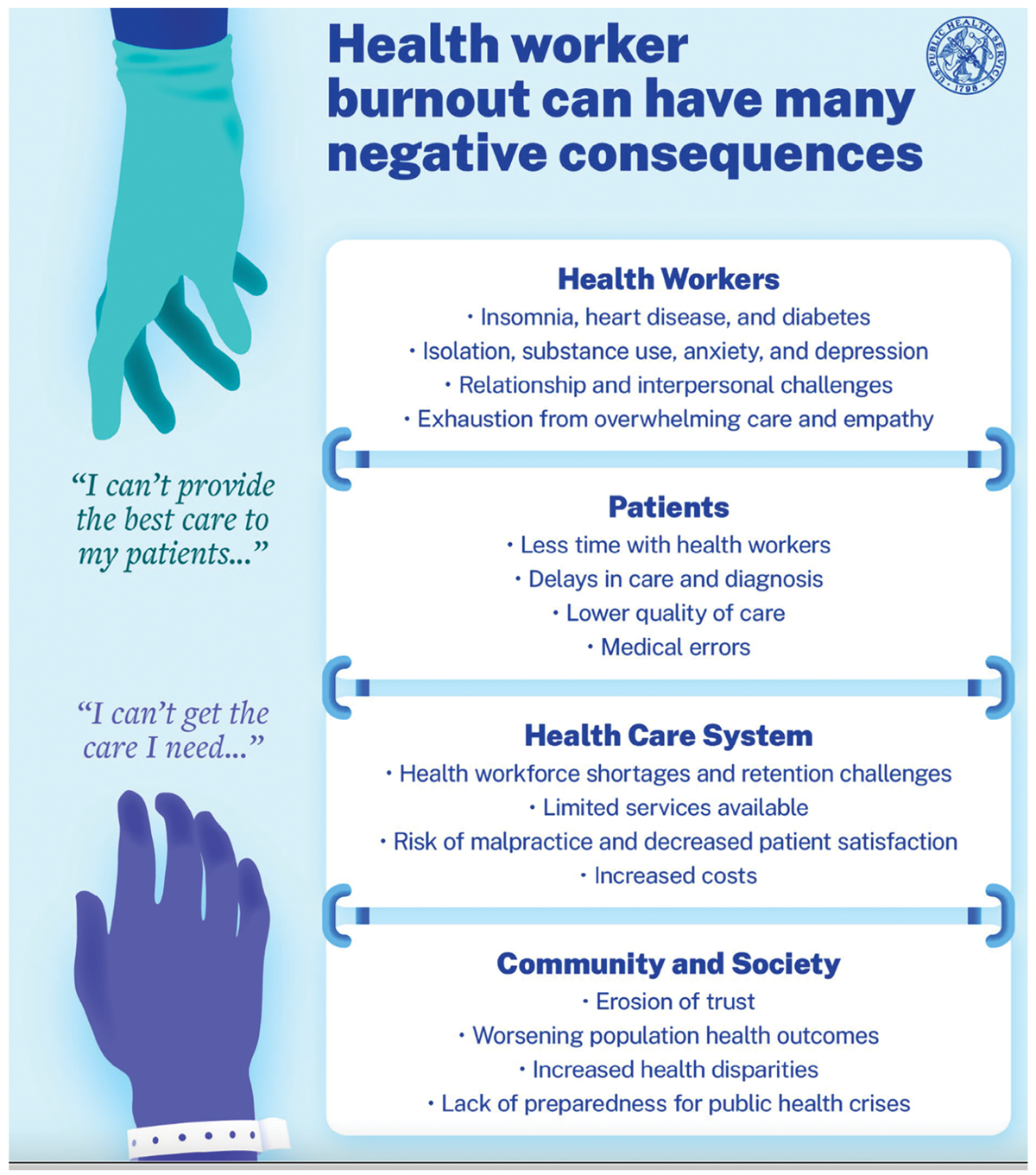
An infographic illustrates the detrimental effects of health worker burnout across various domains: health workers themselves, patient care, the healthcare system, and society at large.
The infographic begins with two quotations from a health worker and a patient: I can't provide the best care to my patients and I can't get the care I need. For health workers, the infographic lists impacts such as insomnia, heart disease, diabetes, isolation, substance use, anxiety, depression, interpersonal challenges, and exhaustion from overwhelming care and empathy. Patients are affected through less time with health workers, delays in care and diagnosis, lower quality of care, and medical errors. The health care system faces workforce shortages, retention challenges, limited services, risks of malpractice, decreased patient satisfaction, and increased costs. For community and society, consequences include erosion of trust, worsening population health outcomes, increased health disparities, and lack of preparedness for public health crises.
U.S. Department of Health and Human Services (HHS). (2022). Health worker burnout. U.S. Surgeon General's advisory on building a thriving health workforce. https://www.hhs.gov/sites/default/files/health-worker-wellbeing-advisory.pdf
Individual providers, healthcare professionals, and HCOs need to support staff well-being and reduce burnout. This will improve staff retention and patient care. The pandemic has made it very clear that when staff practice in intense situations with few breaks or real rest and care for critical patients, they then experience many emotional responses, and some of these may be long-term. Nurse leaders should routinely offer cumulative stress debriefing and support to provide care for their staff-a supportive leader helps staff cope (Griner et al., 2017). To guide leaders as they address this problem, a recent report, National Plan for Health Workforce Well-Being, examined the critical and growing concern of healthcare profession burnout and stress, which was present before the COVID-19 pandemic but increased these problems (NAM, 2022). The report emphasizes the need to take collective action for the future of the nation's health system. Its vision is “patients are cared for by a health workforce that is thriving in an environment that fosters their well-being as they improve population health, enhance the care experience, reduce costs, and advance health equity, therefore achieving the quintuple aim” (NAM, 2022, p. 4). This plan identifies the following priorities (p. 6):
- Create and sustain positive work and learning environments.
- Invest in measurement, assessment, strategies, and research.
- Support mental health and reduce stigma (associated with seeking help).
- Address compliance, regulatory, and policy barriers for daily work.
- Engage effective technology tools.
- Institutionalize well-being as a long-term value.
- Recruit and retain a diverse and inclusive health workforce.
Staff may also experience compassion fatigue, which is the feeling of emotion that ensues when a staff member is moved by the distress or suffering of another and can be associated with burnout, but it is different (Peters, 2018; Mazzotta, 2015; Hooper et al., 2010). Compared to burnout, compassion fatigue is relational, associated with caring for others, and has a sudden onset. Compassion is necessary for effective caring, but long-term coping with exposure to distress (both physical and emotional) of others can lead to compassion fatigue or a state of psychic exhaustion. It is in the interpersonal connection with patients and families that nursing provides its best care, but this context carries risks for the nurse over time. Compassion fatigue is not uncommon in nursing; for example, it may be experienced by nurses working in emergency care and intensive care. Colleagues and supervisors, however, do not always recognize the signs and symptoms in fellow workers indicating the need for support. Many nurses are concerned about sharing feelings they are having because they think it may be viewed as a sign of weakness or poor professional performance, so they do not ask for help. Compassion fatigue is a reason some nurses give for leaving a position or even the profession (Mazzotta, 2015).
Burnout and compassion fatigue are included here because they relate to stress management, requiring a set of skills that students need to develop while in school and continue to use throughout their careers. Prevention and interventions for burnout and compassion fatigue should address work issues and physical and psychological factors (ANA, 2023b). Staff need to understand the importance of having a healthy work-life balance, and managers need to work with staff when they need guidance to achieve this balance. All need to understand the causes of burnout and compassion fatigue. Communication is related to both problems. Effective communication with staff, management, patients, and families under stress can reduce stress. HCOs and management need to consider work interventions to prevent and, if necessary, respond to stress, such as using debriefing, providing resources for counseling, support groups, exercise and yoga, space to take a break, learning stress management techniques, providing nutritious food and snacks for breaks, and so on. Stress management and resilience training are used to assist staff to reduce stress and recover quickly from stressful situations (Magtibay et al., 2017). Using mindfulness to manage stress (to be more fully aware of your situation) also has an impact on staff satisfaction, productivity, and patient care (Ponte & Koppel, 2015).
Indicating the growing concerns in healthcare delivery about stress and burnout, the following two examples demonstrate strategies to address these concerns. The report Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being is a follow-up to the critical IOM Quality Chasm reports that were first published in 1999, but this report turns the focus to the need for immediate actions to address clinician burnout-for the safety, health, and well-being of healthcare professionals, which also needs to be considered for healthcare professions students (NAM, 2019). Healthcare organizations, professional organizations, healthcare education, healthcare technology, healthcare regulation, and government at all levels must be involved in this effort.
The second example is the Action Collaborative on Clinician Well-Being and Resilience, which was formed in 2017 and includes 200 organizations concerned about increasing clinician burnout. The goals of the collaborative are to increase awareness of clinician anxiety, burnout, depression, stress, and suicide; gain better understanding of clinician well-being; and develop evidence-based, multidisciplinary solutions (NAM, 2020a). This collaboration is even more important now due to the strain of the COVID-19 pandemic on healthcare providers, individuals, and organizations. It is also important because it uses an interprofessional approach and recognizes that strategies to resolve these concerns need collaborative efforts-the problems are not isolated and cross all healthcare professionals and services. The link to the collaborative provides many resources for nurses and others in health care. The factors that impact clinician well-being, the clinician-patient relationship, and patient well-being are society and culture, personal factors, skills and abilities, healthcare responsibilities, learning/practice environment, organizational factors, and rules and regulations (NAM, 2020b).
| Stop and Consider 9 |
|---|
| Self-care is important to every nurse. |