This chapter introduces content about health policy and the political process. Both have a major impact on individual nurses, nursing care, the nursing profession, and healthcare delivery. When nurses participate in the policy process, they are acting as advocates for patients, as Abood, who served in government affairs department at the American Nurses Association, explained, and this view continues to be relevant with nurses concerned about the healthcare system and who want to advocate for change focusing on “policies, laws, or regulations that govern the larger healthcare system. This type of advocacy necessitates stepping beyond their own practice setting and into the less familiar world of policy and politics, a world in which many nurses do not feel prepared to participate effectively” (2007, p. 3).
Importance of Health Policy and Political Action
Understanding healthcare policy requires the nurse to step back and see the broader picture of healthcare needs and delivery and the impact of society (values, culture, diversity, equity, community, and so on) while understanding how such policy influences individual care. Political action is part of recognizing the need for health policy; developing policy and implementing policy, including financing policy decisions; and evaluating outcomes. Nurses offer the following resources to health policy making:
- Expertise related to health and healthcare delivery
- Understanding consumer (patient, family, community) needs
- Experience in assisting patients in making healthcare decisions
- Understanding of the healthcare system
- Understanding of interprofessional care
- Collaborating with other healthcare professionals and organizations
Nurses may assume roles in policy-making at the local, state, and federal levels of government. Within these roles, they demonstrate leadership, expertise, advocacy, and the ability to collaborate with others to meet identified outcomes. Sometimes, nurses are successful in getting the policy that they feel is needed for patients and for nursing, and sometimes, they are not. The key to policy-making is to learn from past experiences and try again.
Definitions
A policy is a course of action that affects many people and is inspired by a specific need to achieve certain outcomes. The best approach to understanding health policy is to describe the difference between public policy and private policy. “Public health, policy development includes the advancement and implementation of public health law, regulations, or voluntary practices that influence systems development, organizational change, and individual behavior to promote improvements in health. Such policies can be executed within the health section” (HHS, CDC, 2015). Developing and implementing policy is a method for finding solutions to problems, but not all solutions are policies. Many solutions have nothing to do with government. There are two main types of public policies: (1) regulatory policies (for example, registered nurse (RN) licensure that regulates practice) and (2) allocative policies, which involve money distribution. Allocative policies provide benefits for some at the expense of others to ensure that certain public objectives are met. Often, an allocative decision relates to funding certain healthcare programs but not others, thus having a major impact on services. Health policy is policy that focuses on health and health-related issues, and it may be a public or private policy. Examples of public policies that have had a national impact on health are those prohibiting smoking in public places (initiated through the legislative branch, which makes laws) and abortion rulings made by the U.S. Supreme Court (initiated through the judicial branch). Private policy is made by nongovernmental organizations, such as professional organizations, about a profession and healthcare organizations (HCOs) (for example, a hospital or clinic). The second type of private policy, which may be HCO policies, is discussed in other chapters, along with procedures that are usually associated with this type of policy.
This chapter examines public policy related to health. In summary, a general description of these policies includes the following (HHS, CDC, 2015)
- Health-related laws
- Rules and regulations used to implement legislation and laws and to guide the operation of government and its health-related programs
- Judicial decisions that have an impact on health and healthcare delivery
Policy: Relevance to the Nation's Health and to Nursing
Policies may have an impact on all aspects of health and healthcare delivery, such as care delivery, who receives care, types of services, distribution of healthcare reimbursement, and types of providers and organizations providing health care. Because nursing is a major part of healthcare delivery policy, nurses need to be involved in policy-making and aware of policy changes.
Each of the areas identified in Figure 5-1 relates to individual nurses and to the nursing profession. Roles and standards may be included in state laws and rules/regulations. State boards of nursing and state nurse practice acts set professional expectations and identify the scope of practice for nurses in a state. Federal laws and rules/regulations related to Medicare and Medicaid address issues such as reimbursement for advanced practice registered nurses (APRNs). How nursing care is provided and the type of care provided are influenced by Medicare, Medicaid, nurse practice acts, and other laws, rules, and regulations made by federal, state, and local governments. Health is influenced by federal policy decisions related to Medicare reimbursement for preventive services, the U.S. Department of Health and Human Services (HHS), and its agencies that establish rules and regulations. An agency for which rules and regulations are very important is the Food and Drug Administration (FDA), which manages the drug and medical device approval process and issues related to food and its quality and safety in the United States. State laws, such as those passed in California, New York, Massachusetts, and other states, focused on mandatory overtime and impacted staffing levels. Access to care is often influenced by policy, particularly when related to reimbursement policy and limits set on which services can be provided and by whom. This is relevant to Medicare, Medicaid, and state employee health insurance. Individual HCOs have their own policies and procedures, and often, these are influenced by public policy. Public policy laws, rules, and regulations also have an impact on nursing education-for example, funding for faculty and scholarships, development or expansion of schools of nursing and their programs, and much more. Nursing research is also influenced by policy; funding for research grants primarily comes through government sources, and legislation designates funding for government research and development (for example, funding for the National Institute of Nursing Research [NINR]).
Figure 5-1 Healthcare policy: Impact on health care and nursing.
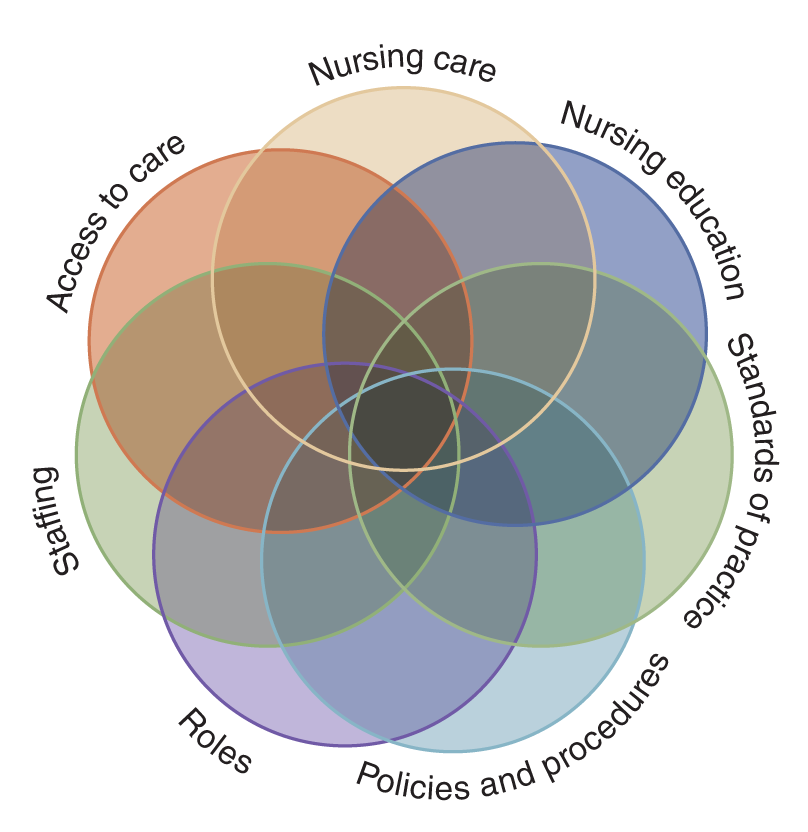
A Venn diagram with overlapping circles, each labeled with different aspects of healthcare and nursing. The circles represent Access to Care, Staffing, Roles, Policies and Procedures, Standards of Practice, Nursing Education, and Nursing Care.
Nurses are experts in health care, and in that role, they can make valuable contributions to the healthcare policy-making process. Nurse expertise and knowledge about health and healthcare delivery are important resources for policymakers. Nurses also have a long history of serving as consumer advocates for patients and their families and for public and community health. Advocacy means to speak for or be persuasive for another's needs. This does not mean that the nurse makes decisions for the patient but rather guides the patient by increasing the patient's understanding of health issues and providing support. When nurses are involved in policy development, for example, they are acting as advocates. Nurses may get involved in policy-making both as individuals and as representatives of the nursing profession, such as by representing a nursing organization. This advocacy is an example of nursing leadership.
Collaboration is very important for effective policy development and implementation. The goal of health policy should be the provision of better health care for citizens. When nurses advocate for professional issues, such as pay, work schedules, the need for more nurses, and so forth, they also influence healthcare delivery. If there are not enough nurses because pay is low, then care is compromised. If there are not enough nurses because few are entering the profession or because schools do not have the funds to increase enrollment or enough qualified faculty, this compromises care. In other cases, nurses advocate directly for healthcare delivery issues, such as by calling for reimbursement for hospice care and home care, supporting mental health parity legislation to improve access to care for people with serious mental illness, or supporting and communicating public interventions during a public health emergency, such as what was done for the COVID-19 pandemic.
General Descriptors of U.S. Health Policy
U.S. health policy can be described by the following long-standing characteristics, which have an impact on the types of policies that are enacted and the effectiveness of the policies (Shi & Singh, 2021). Most countries have national, government-run healthcare systems, but the United States does not. Instead, the private insurance sector is the dominant player in the U.S. health reimbursement system, which is primarily an employer-based insurance. The issue of a universal right to health care has been a contentious one for some time. “The Coalition of Partnerships for Universal Health Coverage and Global Health calls on all countries to urgently reinvigorate progress towards health for all” (Barron et al., 2023, p. E1335). Some people believe that universal health coverage means that countries/governments must provide all available health services free to everyone through national health insurance; however, it actually means that all people should have access to health services they need without experiencing financial hardship (Barron et al., 2023).
The government does have an important role in the U.S. healthcare system, but it does not have the only major role. This stance reflects Americans' view that the government's role should be limited. Chapter 8, The Healthcare Delivery System: Focus on Acute Care chapter, includes content on healthcare financial issues.
The second characteristic important to the United States is the approach taken to achieve healthcare policy, which has been, and continues to be, often fragmented and incremental. This approach does not look at the whole system and how its components work or do not work together effectively so that its parts are not connected to constitute an effective system. Coordination between state and federal policies and even between the branches of the government may also be limited or ineffective. An example of this is the response to COVID-19 and the current evaluation of the U.S. Department of Health and Human Services (HHS) recommending changes to improve its organization and functions (HHS, CDC, 2023; GAO, 2023). The system is further complicated by the wide array of reimbursement sources, complicating services received, by whom, when, and costs.
The third characteristic is the role of the states, which has a significant impact on policy in the United States and states are responsible for the health of their residents. Consequently, since each state makes its own policies, health policies may vary from state to state. Local governments within states are also involved in making policy and should coordinate and not conflict with state-level policy. In some cases, there is a shared role with state and federal governments-for example, with the Medicaid program and application of the Patient Protection and Affordable Care Act of 2010 (typically referred to as the Affordable Care Act or ACA) (HHS, 2023a).
The last important characteristic is the role of the U.S. president (head of the executive branch of government), which can be significant. How does the president influence healthcare policy? Consider President Clinton and his initiative to review the quality of health care in the United States. Clinton established a presidential commission to start this process. Although this commission was short term, which is the case for most commissions of this type, it set the direction for extensive reviews and recommendations that have been identified by the Institute of Medicine (IOM), now known as the National Academy of Medicine (NAM). Clinton also pushed to get the Health Insurance Portability and Accountability Act (HIPAA) and the State Children's Health Insurance Program (S-CHIP) passed. Both laws, which are examples of policies, resulted from the work of this healthcare commission. The expectation was this commission's work would be part of a major healthcare reform initiative, but it failed at the time of the Clinton administration because it did not meet its goal to make major changes in healthcare reimbursement. However, some significant policies did emerge from these efforts-such as the two previously mentioned laws and the IOM initiative to further examine the quality of U.S. healthcare delivery. The issue of healthcare reform was not seriously addressed again until the Obama administration, which developed and pushed for passage of the ACA. The Trump administration made changes to this law, and most likely, over time, other changes will be made by subsequent administrations or by the U.S. Congress. It is not uncommon for presidential administrations to make changes in policies that are different from previous administrations, and often, they are politically based decisions. Presidents also speak out about health policies and actions, such as what occurred during the COVID-19 pandemic with President Trump, and then President Biden spoke to the nation about the pandemic and health policies, such as the use of testing, vaccines, isolation, using masks, the status of schools during the pandemic, impact on workplaces and public transportation, and so on. This not only influences policies but also relates to how the public views, supports, and follows policies. Nurses need to be alert to changes in laws or policies, like ACA and others, and participate in the policy-making process by providing nursing expertise.
Some legislative efforts are reduced over time or eliminated as their designated implementation time ends (law expires), and the laws are not renewed. A recent example is S-CHIP. In 2007, Congress tried to expand this program, but President George W. Bush vetoed the bill. S-CHIP was established to provide states with matching funds from the federal government to enable states to extend health insurance for children from families with incomes too high to meet Medicaid criteria but not high enough to purchase health insurance. Matching funds is one method used by the government to fund programs. With this method, the federal government pays for half, and the states pay for the other half (or some other configuration of sharing costs). Medicaid is funded with matching funds (state and federal funds), but Medicare is funded only with federal funds. The issue of maintaining S-CHIP came up again when the legislation was expiring, which opened it up for elimination or renewal with or without changes. S-CHIP has been an effective program by providing reimbursement for needed care for many children, improving children's access to care and preventive care, and improving their health status. During the time the bill was expiring, Congress and the administration disagreed over the expansion and funding of this program, with the dispute reaching a stalemate during the Bush administration. When President Obama took office, the first bill he signed was one that continued the expansion of this program, blocking its expiration. This is an example of how legislation can be passed by one administration, vetoed by another administration, not renewed when expiring, or taken up again by yet another administration. In 2023, 9.6 million children were enrolled in CHIP coverage, along with some in Medicaid. So even though this law has had a history of varied support, it continues to provide critical healthcare support for a vulnerable population, children (Medicaid.gov, 2023).
| Stop and Consider 1 |
|---|
| Health policy has an impact on healthcare professionals, healthcare organizations, reimbursement, and all aspects of health care from local, state, and national perspectives and thus impacts the nation's health. |
Examples of Critical Healthcare Policy Issues
Many healthcare policy issues are important to local communities, states, and the federal government. Exhibit 5-1 highlights some of these issues, which are often of particular concern to nurses, nursing, other healthcare professionals, and healthcare delivery in general. How policy is developed or whether policy related to each of these issues is developed may vary. Examining some of these issues in more depth provides a better understanding of the complexity of health policy. The examples of policy issues related to nursing covered in this section are not the only healthcare policy issues, but they illustrate some of the types and their relationship to nursing.
| Exhibit 5-1 Potential Healthcare Policy Issues |
|---|
|
The cost of health care in the United States has risen steadily. There is no doubt that better drugs, treatments, and technology are available today to improve health and meet treatment needs for many problems; unfortunately, these new preventive treatments and interventions typically have increased costs. Defensive medicine, in which physicians and other healthcare providers order tests and procedures to protect themselves from lawsuits, also increases costs. Insurance coverage has expanded, and beneficiaries or enrollees expect to get care when they feel they need it. Insurance costs money-premiums and other payments required of enrollees, cost to employers and to the government, insurer costs for both administrative activities and to provide the services, and so on. In turn, cost containment and cost-effectiveness have become increasingly important. Health policy often focuses on reimbursement, control of costs, and greater control of provider decisions to reduce costs. The last of these measures has not been popular with consumers/patients.
For a long time, a critical issue has been whether the United States should move to a universal (national) healthcare system. Early in the discussions about universal health coverage, the following reasons for this type of coverage were identified, and they also relate to nurses and nursing practice. These reasons supporting universal health coverage still apply today (Coffey, 2001):
- Insuring everyone with one national health program would spread the insurance risk over the entire population.
- The cost of prescription drugs would decrease.
- Billions of dollars in administrative costs would be saved.
- Competition could focus on quality, safety, and patient satisfaction.
- Resources would be redirected toward patients.
The ACA did not establish universal healthcare coverage in the United States, though its goal was to improve insurance coverage through Medicaid, expand access for more people who cannot afford health insurance, and provide other methods for people to enroll in healthcare insurance plans. It is, however, not clear if future changes in the ACA or new legislation will alter the approach to healthcare reimbursement, but it was significant legislation when it was passed and implemented. The COVID-19 pandemic led to more discussion about universal coverage as the United States compared its response to the virus, available services and accessibility, coverage for care, and even distribution and administration of testing and vaccines to countries that have universal coverage and were better able to respond to these needs. The World Health Organization (WHO) strongly supports universal health coverage. It supports providing universal coverage so that “all people have access to the full range of quality health services they need, when and where they need them, without financial hardship. It covers the full continuum of essential health services, from health promotion to prevention, treatment, rehabilitation, and palliative care” (WHO, 2023). This is a critical global health policy issue and has a major impact when there are critical global health issues, such as a pandemic, but the United States has not supported this policy change.
Healthcare Quality
Healthcare quality is a critical topic in health care today, recognizing we need to monitor healthcare delivery effectively and improve outcomes. Following President Clinton's establishment of the Advisory Commission on Consumer Protection and Quality in Healthcare (1996-1998), an important area of policy development expanded. What is the status of healthcare quality in the United States? How can healthcare quality be improved? What needs to be done to accomplish this? This focus led to the federal government's request for the IOM, which as of 2015 is known as the National Academy of Sciences, National Academy of Medicine (NAM), to further assess health care in the United States. This resulted in the publication of major reports, often referred to as the Quality Chasm reports, describing in-depth examinations of health care, identifying problems, and offering recommendations related to quality and patient and staff safety, which are components of quality care. Quality health care is discussed in several chapters in this text. The Centers for Medicare and Medicaid Services National Quality Strategy (NQS) was developed in recognition of the need for a national perspective of quality health care (HHS, Centers for Medicare and Medicaid Services [CMS], 2023). Also supporting the need to monitor national health quality are the National Healthcare Quality and Disparities Reports (NHQDR), discussed in more detail in quality care content (HHS, AHRQ, 2023).
Disparities in Health Care
The IOM reports on diversity in health care and disparities and the Sullivan report on healthcare workforce diversity drew attention to a critical policy concern-namely, inequality in access to and services received in the U.S. healthcare system (Sullivan, 2004; IOM, 2004, 2002). Nurses need more knowledge about culture and health needs, health literacy, the ways in which different groups respond to care, and healthcare disparities. How does this impact health policy? Does it mean that certain groups may not get the same services (disparities)? If so, what needs to change? We need regular monitoring of healthcare disparities, and we now do this annually when we monitor healthcare quality and disparities with the National Healthcare Quality and Disparities Reports (HHS, AHRQ, 2023). Stigma is related to disparities and health equity. Stigma is an important social determinant of health that can have a negative impact on physical health outcomes and social well-being and reduces educational achievements and income levels among people who experience stigma. It “causes incalculable human suffering. It intensifies harm against the most vulnerable and marginalized communities. Stigma, driven by upstream factors connected to social control, is an inherently structural phenomenon. Because laws are common and powerful mediators for structural stigma, they are critical levers for antistigma work” (Conyers-Tucker et al., 2022). Structural stigma is found in laws/policies that need to be adjusted at all levels to reduce this problem of stigma. There is additional content on this critical content in several chapters in this text, particularly content related to patient/person-centered care (PCC) and the need for greater consideration of diversity, equity, inclusion (DEI), and accessibility, which can reduce the experience of stigma (HHS, 2023b).
Consumers
There is increasing interest in the role of consumers in health care. Today, consumers are more informed about health and healthcare services than previous generations. An example of a law that focuses on health and the consumer is HIPAA. This law includes regulations related to transferring health insurance from one employer to another, but it also includes expectations regarding the privacy of patient information, which is now a critical factor considered by healthcare providers in daily practice. With the increased emphasis on PCC and then the addition of family-centered care, consumers have gained a stronger voice in their health care.
Commercialization of Health Care
The organization of the healthcare delivery system has changed into a series of multipronged systems, though not all healthcare organizations (HCOs) are of this type. These organizations generally form a corporate model. Such corporations may exist in a local community, statewide, or even nationally. Some of the large healthcare corporations also have hospitals in other countries. This change has had an impact on policies related to financing health care and quality concerns. Over time, the commercialization of health care has led to more business practices in healthcare delivery, such as marketing, control of budgets, and so on, and not all of it is positive.
Reimbursement for Nursing Care
Reimbursement for nursing care must be viewed from two perspectives. The first view considers reimbursement methods for nursing care services, particularly inpatient or hospital services. There has not been much progress in this area. Hospitals usually do not clearly identify the specific costs of nursing care in a manner that directly affects reimbursement. The second view involves reimbursement for specific individual provider services instead of reimbursement for an organization provider, such as a hospital. Physicians are reimbursed for their services. There have been major changes in how APRNs are reimbursed; thus, this situation is improving, though more needs to be done. For example, if an APRN provides care in a clinic or a private practice, the question arises: How are the APRN services reimbursed? Will the patient's health insurance pay for these services? Some services are covered by federal government plans, but there is great variation in reimbursement from nongovernment plans. The ACA and other initiatives, such as those identified in the report The Future of Nursing: Leading Change, Advancing Health (IOM, 2011), have supported greater use of APRNs. To ensure that APRNs are used, reimbursement practices need to support the use of APRNs. There has been, however, more movement to improve APRN reimbursement than there has been in the clarification of reimbursement for nursing services in hospitals and other types of HCOs.
Immigration and the Nursing Workforce
Immigration of nurses to the United States has an impact on global and U.S. healthcare delivery. This is an important international policy issue, but one that is not yet resolved. COVID-19 has had an impact on this issue (Batalova, 2020). Important considerations related to nurse immigration include regulations (visas to enter the United States and work; nursing licensure), level of language expertise, quality of education, orientation and training needs, and potential limits on the immigration of RNs. Some of the issues need to be addressed by laws, rules, and regulations and by state boards of nursing, and there is greater global academic nursing education collaboration. Other chapters discuss issues related to this policy concern.
| Stop and Consider 2 |
|---|
| Multiple healthcare policy issues are influencing nurses today. |
Nursing Agenda: Addressing Health Policy Issues
The ANA has long advocated for a variety of healthcare issues through its membership and political action activities. The organization identifies key policy issues that it will focus on during each U.S. congressional session. The issues vary depending upon need; for example, the ANA advocated for the passage of the ACA and spoke about changes that have been recommended by some experts and politicians. Examples of issues identified on the ANA website are healthcare system transformation, health informatics, and care coordination (ANA, 2023a). The ANA agreed with the IOM Quality Chasm report series recommendations supporting care that is safe, timely, effective, efficient, equitable, and patient/person-centered and continues to support these areas through its policies. The ANA agendas are examples of how a professional organization speaks for the profession, delineates issues that need to be addressed through policies, commits to collaborating with others to accomplish policy agendas, and advocates for patients/families/populations through such statements and lobbying efforts. Individual nurses and nursing students should participate in this process. The ANA is also engaged in addressing issues related to diversity, such as racism and its impact on health policy, which is currently a critical issue throughout healthcare delivery. The organization formed the National Commission to Address Racism in Nursing. The commission, which is a collaborative initiative with representatives from several organizations, “examines the issue of racism within nursing nationwide focusing on the impact on nurses, patients, communities, and health care systems to motivate all nurses to confront individual and systemic racism” (ANA, 2021). Racism impacts policy and needs to be considered at all levels: government, professional organizations, professional education, healthcare services, and individual healthcare providers. Other examples of policy issues that the ANA and other healthcare professionals are concerned about and recognize that they are connected to policies are workplace violence, staff and shortages, workplace safety, access to care, and improvement in all levels of nursing education.
Other nursing professional organizations, such as specialty organizations and the major nursing education organizations (National League for Nursing [NLN] and American Association of Colleges of Nursing [AACN]), are also engaged in policy as it pertains to their members and their organization goals. The NLN 2023-2024 policy agenda generally focuses on education, workforce, access, and diversity and inclusion and identifies the following concerns (NLN, 2023):
- Programming to attract, educate, and retain diverse candidates for nursing faculty and the nursing workforce.
- Research to advance the science of nursing education.
- Access to technological innovations in nursing education.
- Regulatory reform that facilitates the full-scope practice of nurses with advanced credentials and encourages the development of new models of care that meet high quality and safety standards.
- Increased and equitable compensation for members of the nursing workforce.
- Expanded emergency and disaster preparedness training.
- Equitable access to comprehensive health care for individuals, families, communities, and diverse populations.
- Public health campaigns, preventative care, promotion of healthy living, and initiatives on environmental policies and climate change designed to improve public health.
- Strategic, evidence-based approaches to enhance inclusivity and civility in academic and clinical work and practice environments.
- Collaboration among national nursing organizations and other essential partners as mutual stakeholders in achieving health equity and tackling challenges presented by social determinants of health.
The AACN agenda items or goals included to advance higher education, develop the workforce, pursue transformative research, and redefine models of care and their core values applied to these agenda items are to be sustainable, innovative, and inclusive (2023a).
| Stop and Consider 3 |
|---|
| Nursing organization agendas have an impact on healthcare policy. |
The Policy-Making Process
Health policy is developed at the local, state, and federal levels of government, but the two most common levels are state and federal. At the state level, the typical broad focus areas are public health and safety (for example, surveillance of disease, immunization, air quality, water safety, public safety and law enforcement, fire and rescue, and so forth); care for those who cannot afford health services, for example, use of Medicaid; purchasing care through state insurance, such as for state employees; regulation (for example, RN licensure); and resource allocation (for example, funding for care services, research grants, funding for nursing education). At the federal level, there are many different needs and policymakers. The focus areas are much the same as at the state level but apply to the nation as a whole and usually are more complex because they require more collaborative efforts to ensure national acceptance.
Federal legislation is an important source of health policy. Prior to the healthcare reform legislation of 2010 (ACA), the two laws that had the greatest impact on U.S. health care were the Social Security Act of 1935 and the Public Health Act of 1944. The Social Security Act established the Medicare and Medicaid programs, the two major government-run healthcare reimbursement programs, managed through the U.S. Department of Health and Human Services (HHS), Agency for Healthcare Research and Quality (AHRQ). The Public Health Act consolidated all existing public health legislation into one law, and it, too, has been amended over the years. Some of the programs and issues addressed in this law are health services for migratory workers, the establishment of the National Institutes of Health (NIH), nurse training funding for students and schools of nursing, prevention and primary care services, rural health clinics, communicable disease control, and family planning services. Subsequent amendments to the law also provide funding for nursing education. An important amendment to this law established the Healthy People initiative in 1990, with subsequent 10-year interval reviews and revisions. The current version is Healthy People 2030, which is discussed throughout this text (HHS, ODPHP, 2023).
The policy-making process is described in Figure 5-2. The first step is to recognize that an issue might require a policy. The suggestion of the need for a policy can come from a variety of sources, including professional organizations, consumers/citizens, government agencies, and lawmakers.
Figure 5-2 The policy-making process.
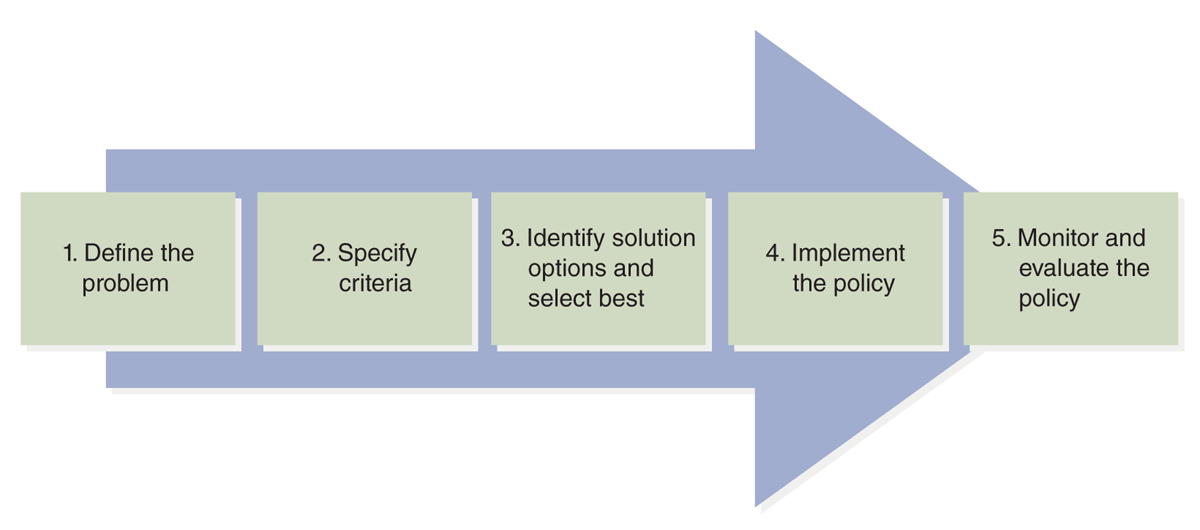
A diagram outlines the five steps in the policy-making process.
The sequence is as follows: 1. Define the problem. 2. Specify criteria. 3. Identify solution options and select best. 4. Implement the policy. 5. Monitor and evaluate the policy.
The second step is to learn more about the issue and use this information to determine if a policy is necessary and what it should include. This examination of an issue may reveal that there is no need for a policy. There may be, and often is, disagreement about a policy need, and there may also be disagreement about how to resolve it if the need exists. Information and data are collected to get a clearer perspective on the issue from different sources, such as experts, consumers, professionals, relevant literature (such as professional literature), and research.
Using this information, policymakers then identify possible solutions. They should not consider just one solution because only under rare circumstances is a single solution possible, and it is best to examine options before making a final decision. During this process, policymakers consider the costs and benefits of each potential solution. Costs are more than financial-a cost might be that some people will not receive a service when they need care, whereas others may get care. What impact will this have on both groups? After the cost-benefit analysis is done, a solution is selected, and the policy is developed. It must then go through the approval process, a process that may be influenced by politics.
It is at this time that implementation begins, although how a policy might be implemented must be considered as the solution is selected and the policy developed. Perhaps implementation is very complex, which in turn affects the policy. For example, if a policy decision states that all U.S. citizens should have healthcare insurance, the policy statement is very simple; however, when implementation is considered, this policy would be very complicated to implement. How would this be done? Who would administer it? What impact would it have on states, federal government, and employers? How would funding be designed to pay for this system? What would happen to current employer coverage? Would all health services be provided? How much decision-making power would the consumer have? How would providers be paid, and which providers would be paid? What impact would this have on the availability of services and appointments? What impact would this have on healthcare staffing and education for healthcare professionals? Many more questions could be asked, and it is important to identify as many of the potential questions as possible and then determine answers to the questions. Policy development must include an implementation plan. Social, economic, legal, and ethical forces influence policy implementation. The best policy can fail if the implementation plan is not reasonable and feasible and should include clear goals and objectives that are then used to evaluate outcomes. As the political process section in this chapter discusses, the policy is often in the form of legislation (law) and influenced by local, state, and national politics.
Coalition building is important in gaining support for a new policy and in the legislative process. As noted in the political process content, gaining support is especially important in getting laws passed. When a policy relates to a healthcare issue, some groups that might be included in coalition building are healthcare providers (for example, physicians, nurses, pharmacists); healthcare organizations, particularly hospitals; healthcare professional organizations (for example, the ANA, the American Medical Association (AMA), the American Hospital Association (AHA), The Joint Commission, the AACN, the NLN); state government and related activities, such as the state board of nursing, the Council for State Boards of Nursing, and other organizations; research initiatives and the National Institutes of Health; elected officials; business leaders; third-party payers; and pharmaceutical industry representatives. Members of a coalition that support a policy may offer funding to support the effort, act as expert witnesses, develop written information in support of the policy, provide information and evidence, and work to get others to support the policy, such as lawmakers who may vote on the legislation.
After a policy is approved and implemented, it should be monitored, and its outcomes evaluated. For a federal policy, the U.S. Congress may require routine reports to ensure Congress is informed of the implementation status of its laws and outcomes. This type of monitoring also applies to the state legislative process and state policies. This all may impact future changes or the determination that a policy is not effective or may not be needed. The process may then begin again.
| Stop and Consider 4 |
|---|
| To develop an effective healthcare policy, the policy-making process should be followed. |
The Political Process
The preceding description of the policy-making process may seem to be a clear step-by-step process, but it is not. It is greatly influenced by politics and stakeholders who are either invested in the policy or do not want the policy and thus can limit what might done. Identifying the need for a policy and what might be included in a policy may involve several different views and parties, and disagreement may result. Since not all interested parties may accept a policy, efforts may be made to defeat a policy. In addition, partisan issues-that is, Democrat versus Republican-may affect the policy development and approval process.
Public policy should meet the needs of the public, but in reality, it is more complex than this. Politics influences policy development and implementation, and sometimes politics interfere with the effectiveness of policy development and implementation. Political feasibility must be considered because this aspect can mean the difference between a successful policy and an unsuccessful policy. Political support, usually from multiple groups, is critical, and healthcare providers need to understand political positions and, in some cases, use politics to benefit health care.
As discussed, most major healthcare policy changes or new policies are made through the legislative process, though some may be made or influenced by executive or judicial components of government. Steps 1 through 4 of the policy-making process depicted in Figure 5-2 are similar to the legislative process steps. Once the policy is developed in the form of a proposed law, the legislative process merges with the policy-making process. The legislative process varies from state to state, but all states have a legislative process that is similar to the federal process. When a federal bill is written and then introduced in Congress, in addition to its title, it is given an identifier that includes either H.R. (House of Representatives) or S. (Senate), based on which congressional chamber initiates the bill, plus a number-for example, H.R. 102. The bill is then assigned to a committee or subcommittee by the leadership of the Senate or House, depending on where the bill begins its long process to determine approval and a final vote. In the committee, the bill may figuratively die, meaning that nothing is done with it. Conversely, if there is some support for the bill, the assigned committee or the subcommittee will assess the content. This might include holding hearings on the bill for extensive discussion and sharing of information, often with witnesses (experts and others). Amendments may be added. If the bill began in a subcommittee, it may be sent on to a full committee and then progress to the full House or Senate for a vote. If the bill began in a committee, it may be sent directly to the full House or Senate.
When the bill gets to the full House, it first goes to the rules committee. There, decisions are made about the debate on the bill, such as the length of the debate. These decisions can have an impact on the successful passage of the bill. The Senate does not have a rules committee, and senators can add amendments and filibuster or delay a vote on the bill. There is more flexibility in the Senate than in the House. The leader in the Senate (majority leader) and the House leader have a great deal of power over the legislative process. A bill cannot be passed only in the House or only in the Senate and become law; rather, both the House and the Senate must pass the bill for the bill to progress to the president for signature. Sometimes a bill is introduced at the same time in both the House and the Senate, allowing the approval process to proceed in both simultaneously. Decisions may then need to be made to reconcile any differences in the two bills that are passed by each, requiring a conference committee composed of both representatives and senators to collaborate to make one version of the bill. The altered bill must then go back for votes in both the House and the Senate. Allocation of funding is a critical aspect of legislation and associated regulations. If both houses of Congress pass the bill, then the bill moves from the legislative branch of government to the executive branch for presidential signature. Figure 5-3 identifies the branches of government.
Figure 5-3 The branches of the U.S. federal government.
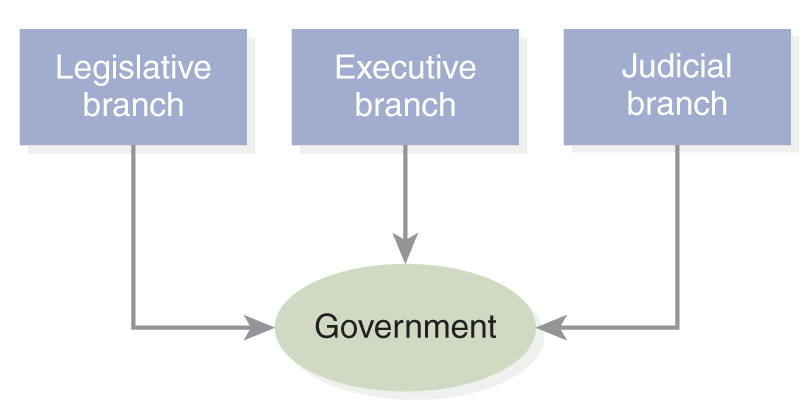
A diagram of the three branches of the Government: Legislative, Executive, and Judicial.
The president has 10 days to decide whether to sign the bill into law. If the president waits longer than 10 days or Congress is no longer in session, the bill automatically becomes law just as if the president had signed it. In some cases, it is made public, either before the president receives the bill or soon after, that the president plans on vetoing a bill, not signing the bill. In this case, Congress may decide not to pursue the bill any further or Congress may decide to bring the bill back to Congress for another vote to try to override the president's veto. This effort may or may not be successful, but it often is a highly politicized situation. Depending on the number of votes, at this point, the bill could either become law or die with no further action taken. During this process there is often a great deal of communication and negotiation about the content and approaches to take to get a bill passed or rejected.
If the president signs the bill or Congress overrides a presidential veto, the bill goes to the regulatory agency that would have jurisdiction over the law. For example, a health law would typically go to HHS. If the law relates to Medicare, it would go to the Centers for Medicare and Medicaid Services, the agency within the HHS responsible for these programs. It is at this point that a very important step in the process occurs. Rules or regulations are written for the law describing how the law will be implemented, and the law's content and implementation make a significant difference in the effectiveness of the law. At specific steps in the regulatory development process, the public, including healthcare professionals, such as nurses, can participate by providing input, and this is important input. Once the final rules are approved, the law is implemented. There may be a date that the law ends, or “sunsets.” If so, the law may expire, or it may be reintroduced into the legislative process, and in some cases, the president can extend the law.
Nurses' Role in the Political Process: Impact on Healthcare Policy
As healthcare professionals, nurses bring a unique perspective to healthcare policy development because of their education, clinical expertise, professional values and ethics, advocacy skills, experience with interprofessional healthcare teams, and understanding of health and healthcare delivery. Significant progress has occurred over the years toward advancing nursing's presence, role, and influence in the development of healthcare policy. However, more nurses need to learn how to identify issues strategically; work with decision makers; understand who holds the power in the workplace, communities, and state- and federal-level organizations and government; and understand who controls the resources for healthcare services (Ferguson, 2014). Many schools of nursing offer courses on health policy, particularly graduate courses, or health policy content is integrated into courses, such as a course that uses this text. These courses or content help to prepare all nurses to better understand policy and how they might be involved in health policy at multiple levels. Nursing publications, textbooks, and journals also focus on health policy or include this topic when it relates to other nursing topics. It is also important that nurses collaborate with other healthcare professionals in advocating for health policy. To better ensure that this occurs, more needs to be done to provide opportunities for interprofessional healthcare education on health policy to help students from a variety of professions (such as medicine, nursing, pharmacy, and so on) develop competency to work together early, before practice begins (Eaton et al., 2017). This will help to develop better understanding of roles and communication and appreciation of what different professions have to offer and how they improve advocacy.
Although the nursing profession has gained political power, it is still weaker than it should be. “Nurses are sorely underrepresented in elected office-from local school boards to the halls of the U.S. Congress. Currently, only three nurses serve in the House of Representatives and a nurse has never served in the Senate. The National Conference of State Legislatures tracks state legislators' occupations. Because so few nurses serve in state legislatures, they don't even merit an occupational category; they're included among “other” (Sommers & Gordon, 2022). Put simply, given the large number of nurses in the United States and nursing's significant contributions to healthcare delivery, the profession should have more influential power. Each nurse is a potential voter and, therefore, has potential influence over who will be elected and legislative decisions. However, nursing as a profession has struggled with organizing, and this weakness has diluted the political power of nurses in the United States. At the most basic level, nurses have experienced serious problems defining the profession. The use of multiple entry levels, licensure issues, and multiple titles confuse the public and other healthcare professionals. Policymakers may not understand the various nursing roles and titles, which in turn makes it difficult for nurses to speak with one voice for nursing.
Nurses need to develop political competence. This requires the ability to use opportunities, including networking, highlighting nursing expertise, using powerful persuasion, demonstrating a commitment to working with others, thinking strategically, and persevering. It means being aware of the rules of the game and recognizing that the other side needs something. Sometimes giving up or modifying one viewpoint or action may lead to more effective results, recognizing that compromise may be an important strategy to apply. Collective strength can be powerful, so finding partners and developing effective teamwork makes a difference. Nurses can network to find those partners. Sometimes partners may be found in the least likely groups, so nurses need to be alert as to who might have an interest in the same concerns nurses have about health and healthcare access and delivery.
It is important to view policy as a tool for change, and nurses are very adept at working with change-something they do in practice daily. This capability should help nurses develop political competence. “Successful advocacy depends on having the power, the will, the time, and the energy, along with the political skills needed to ‘play the game' in the legislative area” (Abood, 2007, p. 3). How can nurses have an impact on healthcare policy? The following content emphasizes what needs to be done to increase nursing influence.
Getting Into the Political System and Making It Work for Nursing
Lobbying is a critical part of the U.S. political process, and nurses are involved in lobbying. A lobbyist is a person who represents a specific interest or interest group that tries to influence policy-making. The First Amendment to the U.S. Constitution gives citizens the right to lobby-to assemble and to petition the government for redress of grievances. Lobbyists want to influence legislators-the decision-makers-as well as public opinion. They often collaborate via coalitions and work with other interest groups to gain more support for a specific interest. Lobbyists particularly focus their efforts on contacting legislative staff who have a major role in getting data about an issue, formulating solutions that may become bills and developing bills to be submitted for passage-all of this is done for elected representatives. Nurses who visit state and federal representatives typically meet with legislative staff, which is a form of lobbying.
Professional organizations hire staff to be lobbyists at both state and federal levels. The ANA, the NLN, the AACN, and other nursing organizations have formal lobbyists who work in Washington, DC. Lobbyists may be nurses or persons who are informed about nursing and work with nurses to provide the best information to move an issue forward that supports nursing. This is typically a paid position. Exhibit 5-2 identifies examples of federal government agencies monitored by the ANA so that the organization is aware of legislative and regulatory activities and can impact policy.
| Exhibit 5-2 Important Federal Government Departments and Agencies |
|---|
|
At both the state and federal levels of government, the legislative branches are highly dependent on committees. Legislative work occurs mainly within committees. If legislation (a bill) gets “stuck” in a committee, this can be the critical barrier to passage of the bill. An example is a recent bill that addressed registered nurse staffing (H.R. 2581), Nurse Staffing Standards for Hospital Patient Safety and Quality Act of 2019. This bill was sent to the Subcommittee on Health Finance (Committee on Energy and Commerce) and did not move forward (Congress.gov, 2019). The bill focused on requiring hospital-wide staffing plans to meet the needs of patients and delivery of quality care. This type of time lag often indicates an inability to gain support for a bill; reasons may vary, such as the bill's policy issue, content of the bill, other bills that may conflict or be more important, disagreement among stakeholders, funding, and more. There are committees on both sides of the federal legislative body/chamber, the House and the Senate. Some of the healthcare-related committees in the U.S. Congress are identified in Exhibit 5-3.
| Exhibit 5-3 U.S. Congressional Committees with Jurisdiction Over Health Matters |
|---|
| U.S. House of Representatives |
|
| U.S. Senate |
|
Within the House and the Senate, committees include representatives from both major parties, Democrat and Republican. The party with the majority in the House and in the Senate decides who will chair committees and who will serve on each committee. To effectively influence legislation, it is important to understand which committee will be involved in the legislation and who is on the committee. What are the chair's and the committee members' views on the issue? How can they be persuaded? Knowing this information can help develop a more effective strategy to influence the policy content and chance of success, and may identify approaches to gain more support from stakeholders. Since this is a complex process involving many people, there may need to be some negotiating and compromises.
Political action committees (PACs) are very important in the political process. A PAC is a private group, whose size can vary, that works to get someone elected or defeated. PACs represent a specific issue or group. The Federal Election Campaign Act of 1971 covers PACs and how organizations may use them. The law defines a PAC as an organization that meets specific limits related to the number of contributions or expenditures for the purpose of influencing an election. Other rules about PAC operations are also identified. PACs do not force organization members to vote on certain candidates-this is always an individual choice, even if a PAC supports a candidate.
Why would nurses need to know about PACs? The nursing profession has its own PACs, such as the ANA PAC. The ANA considers political action to be a core mission activity, and its PAC is critical to its success on Capitol Hill (ANA, 2023b). The PAC is a form of political advocacy that focuses on supporting candidates, and if it is connected to nursing, it is concerned with the candidate's views of identified nursing issues. The PAC endorses and campaigns for candidates, but it makes minimal campaign donations based on legal requirements. The decision to support a candidate is not based on the candidate's party but rather on whether the candidate supports issues important to nursing. In the end, this empowers the PAC members-in this case, nurses. The ANA PAC's overall goal is to improve the healthcare system in the United States. Any nurse can join this PAC by contributing to support the PAC's candidate choice and participating in determining who will be supported.
Nurses need to work to get their message across using grassroots advocacy. Many nurses communicate directly with legislators about specific issues of concern. One method of doing this is through written communication. In the past, this was primarily done through letter writing, but now it is easier, and preferred by legislators, to use email for this purpose. Email and other electronic methods are more efficient. They allow nurses to respond quickly to requests to communicate their views. The request to contact candidates or elected officials may come from a nursing organization because of a recognition that something (an action or potential action, such as legislation) affects health care and nursing, from a colleague, or maybe something an individual nurse considers important.
In written communication to legislators, even if through electronic means, it is important to identify the issue, provide the bill number (if the correspondence is related to a pending bill), succinctly state one's position, and provide a brief rationale for the position. The communication should include the nurse's full name, credentials, employment location, contact information, and voting district. To be more effective, the best contact is the nurse's elected representatives. Another method of communication is to call elected representatives' offices. Before making the call, the nurse should prepare a brief statement that addresses the specific issue and use this during the phone conversation. A third method of communication is to arrange an appointment to visit elected representatives' local offices, offices in the state capital, or in Washington, DC. The nurse probably will meet with the legislative staff, preferably staff responsible for health issues. Staff members have a major role in the process and can be very helpful. It is important to confirm the appointment and to be on time. The meeting may be short or long, and this is guided by the person with whom the nurse is meeting. Be engaging and let the staff or representative/senator know what you do as a nurse, where you work, and relevant nursing and healthcare concerns. Be prepared to discuss both the topic and the activities of the representative-legislation and other interests. Provide specific useful information and examples that support facts and avoid generalities, presenting your information concisely-staff and legislators are busy. Students who visit legislators or their staff, for example, might discuss the need for scholarships and financial aid, providing examples of how this support helps students meet career goals and provides more nurses. Follow-up is important; send a thank-you note with a reminder of the discussion.
All these examples related to policy demonstrate leadership by nurses who participate in these efforts to advocate for health care. Exhibit 5-4 summarizes some tips to make grassroots efforts more effective.
| Exhibit 5-4 Grassroots Tips |
|---|
| Letter or Email Communication With Legislators or Staff |
|
| Contact With Legislators or Staff |
|
| Visiting Members of Congress or State Legislature |
|
Nursing organizations are involved in policy development through lobbying, members and officers serving as expert witnesses to government groups and agencies, and publishing information about issues in both professional and nonprofessional literature. Radio and television journalists and also internet sites may interview nurses. These activities place nurses directly in the policy-making process and improve nurses' public image as experts and consumer advocates.
The AACN holds student policy summits to inform students, such as graduate students, about involvement in Capitol Hill visits and policy work (AACN, 2023b). Student participants then make visits to Capitol Hill with school of nursing deans and directors. Information is provided for all who make these visits so that they are prepared with the facts. AACN conferences for faculty and deans are held in Washington, D.C. and typically include visits to Congress and/or offer sessions in which representatives and senators are invited to speak with attendees about nursing education, the profession in general, and implications for healthcare delivery.
There are numerous opportunities for nurses to gain experience in government practice. For example, fellowships-many of which are short term-at the federal and state levels provide opportunities for nurses to learn more about politics and the legislative process, interact with people who work in government, and, if interested, learn more about potential government job opportunities. Graduate programs focused on health policy provide formal academic experiences that can lead to a career in the health policy field.
Some nurses seek election to government positions at local, state, and federal levels. Others serve as staff in health-related government agencies. Nurses who serve in government positions use their nursing expertise, and this provides opportunities for nurses to be more visible at all government levels-legislative, administrative, and judicial. However, there needs to be greater representation of nurses in these positions. Running for office at any level requires political support, finances, and guidance from those experienced in the world of politics and campaigning. If you choose to pursue this path, be aware that it takes time to build up support for a campaign.
Nurses may have staff positions in many levels of government. These positions provide great opportunities for nurses to use their expertise and participate in health policy development and implementation. Nurses have served in high-level government positions. For example, in 2013, Marilyn Tavenner, MHA, BSN, RN, was confirmed as the administrator of the CMS. This is a very important position providing oversight for the federal government's (and the nation's) largest entitlement program and having a nurse in the position provided greater recognition of nurses. In 2015, Tavenner left this government position and assumed a high-level position at the American Health Insurance Plans (Matthews, 2015). This is one example of many, but we need more nurses in government leadership and policy-making.
| Stop and Consider 5 |
|---|
| You can participate in the political process to advocate for health care and for the nursing profession. |
Critical Healthcare Legislation
Over the years, there have been many attempts to reform the U.S. healthcare delivery system. Most of these efforts have failed. Political issues have typically limited progress in this area-healthcare delivery is a critical political issue because it affects taxes and is a very expensive business. The 2008 presidential election brought healthcare reform to the forefront again. As was true with other efforts, nursing organizations got involved and spoke out about proposed changes. It was very important that nursing was involved because healthcare reform would have an impact on nursing, and it has proven to have an impact during its implementation.
In 2010, Congress passed significant legislation, the ACA, signed into law by President Obama. The purpose of the law was to reform some aspects of healthcare insurance coverage in the United States. Although universal healthcare coverage was not included in the final bill owing to a lack of political support, more people in the United States obtained health insurance coverage under this law. This law, however, did not change the traditional employer-based approach to U.S. health insurance.
The healthcare delivery system has experienced changes because of the various reform efforts. Nurses are assuming new roles and changing old ones-for example, APRNs, nurse managers, clinical nurse leaders, and clinical nurse specialists. Their roles may vary, and more opportunities are opening up. In some cases, nurses with these advanced degrees are eligible for admitting privileges, meaning that they can admit their patients to the hospital from private practice or clinics. Healthcare reform and other critical sources, such as the report The Future of Nursing, emphasized the need to expand the use of APRNs in primary care (IOM, 2011), and this continues to be recommended in a current follow-up report (NAM, 2021). The United States is experiencing a shortage of primary care providers, and with the changes in healthcare reform increasing the number of people who have health insurance coverage, there is even greater demand for these providers.
The large number of patients who cannot pay for services and have no insurance coverage causes major financial problems for hospitals. In some situations, this may lead to the closing of units and fewer beds (decreasing the size of the hospital and its services); termination of staff; and, in extreme cases, the closing of hospitals. Patient access to care has become a major problem in some communities. Accessibility is more than just getting an appointment; it involves the availability of services at times convenient for the patient (time of day and day of week); transportation to and from the care facility; reimbursement for care; and receipt of the right type of care, such as from a specialist. An increase in U.S. citizens with insurance coverage, such as what occurred with the ACA, has an impact on these services and the ability to cover costs. This law has undergone some changes from one presidential administration to another, and more changes are expected.
Healthcare reform continues to have an impact on nursing education, nursing practice, regulation of nursing, and professional roles. There are provisions in the ACA that relate to issues other than reimbursement, such as quality care, funding for healthcare provider education, workforce issues, and more. The provisions did not all go into effect at one time. It is not known what impact changes to this law may have on these important issues.
| Stop and Consider 6 |
|---|
| The ACA is a law that continues to change. |