This chapter introduces a variety of public/community health issues, such as health promotion and disease prevention, continuum of care, healthcare disparities and equity, chronic disease, and delivery of care in a variety of settings in the community. Nursing education programs provide clinical experiences for students in many of the settings and situations discussed in this chapter, and students also learn about this content in public/community health courses and related clinical experiences. In this chapter, public/community health is introduced as an important component of healthcare delivery and nursing. Where do patients receive care? Who are the patients? How are health and illness viewed by patients and by nurses, and what impact does this view have on healthcare delivery? Whether nurses work in public/community health settings or not, they need an understanding of these critical care issues. The COVID-19 pandemic that began in 2020 emphasized the need to develop and improve public/community health initiatives, programs, and services. These services can impact many people. Supporting the concern about the healthcare system and public health status there are current initiatives to make changes. Noting the coronavirus COVID-19 pandemic's high death toll and other negative U.S. health indicators, the Commonwealth Fund Commission on a National Public Health System issued recommendations for action to be led by the U.S. Department of Health and Human Services (HHS) and Congress. There is a critical need to develop “a robust, coordinated system that better protects lives and handles health emergencies” (CFC, 2022). The federal government should provide leadership for a national public health system, with Congress providing support and requiring clear expectations for all areas of the country. The primary care and acute care components of the healthcare system should collaborate with public health agencies routinely and during emergencies. It is important that the system earn the public's trust and improve to avoid problems that have been experienced during COVID-19, such as ineffective coordination and collaboration, which leads to ineffective services, health inequities, increased chronic illnesses, and unnecessary mortality. Health outcomes must be improved in all communities and integrate local, state, and federal participation and apply continuous improvement.
A National Initiative to Improve the Nation's Health: Healthy People 2030
The HHS, its agencies, and other government departments that have responsibilities related to health and healthcare services (federal, state, and local) are charged with developing programs that promote health and prevent disease and illness and provide data to evaluate outcomes and support the Healthy People 2030 initiative (HHS, ODPHP, 2023a), This is a major national prevention initiative that focuses on improving the health of Americans by providing a comprehensive health promotion and disease prevention plan that is evaluated over time. There are six editions of Healthy People (1979, 1990, 2000, 2010, 2020, and the current 2030) with revisions completed every 10 years. Its vision and major goals that should be reached by 2030 focus on the topics of health conditions, health behaviors, populations, settings and systems, and greater emphasis on the social determinants of health (SDOH), which are included in the initiative's framework (HHS, ODPHP, 2023b). Exhibit 7-1 describes the 2030 vision, mission, principles, goals, and plan of action, and Figure 7-1 highlights the Healthy People 2030 framework's critical concerns.
| Exhibit 7-1 Healthy People 2030 Framework |
|---|
| Vision |
| A society in which all people can achieve their full potential for health and well-being across the life span. |
| Mission |
| To promote, strengthen, and evaluate the Nation's efforts to improve the health and well-being of all people. |
| Foundational Principles |
| Foundational principles explain the thinking that guides decisions about Healthy People 2030. |
|
| Overarching Goals |
|
| Plan of Action |
|
Figure 7-1 Healthy People 2030 Framework.

An infographic illustrates five key areas of the Healthy People 2030 Framework.
The infographic outlines the five key areas of the Healthy People 2030 Framework, centered around a main icon symbolizing community or population health. Each key area is represented by a distinct icon: An icon of magnifying glass over three people. An icon of a group of three people standing on bars of different height. An icon of two hands within a heart. An icon of two people under medical cross. A colorful pie chart icon divided into six sections, each with a different symbol representing various community services. These icons are connected by lines to the central figure, emphasizing the interconnected nature of these health areas.
U.S. Department of Health and Human Services (HHS), Office of Disease Prevention and Health Promotion (ODPHP). (2020). https://health.gov/healthypeople
The Healthy People initiative provides an accessible plan developed by experts, based on evidence, and identifies achievable goals and objectives to guide the action of individuals, communities, and stakeholders to improve health (see Figure 7-2). To achieve the health and well-being of all people, it is essential to involve, as active partners, diverse stakeholders from across the public, private, and nonprofit sectors. It is important to monitor progress on Healthy People goals and objectives and share high-quality data and feedback on progress with stakeholders and the public. In addition, we have learned that significant changes (e.g., reduced rates of smoking) may be difficult but are achievable through persistent effort. Although much progress has been made, the United States is behind other developed countries (such as other members of the Organization for Economic Co-operation and Development [OECD]) on key measures of health and well-being, including life expectancy, infant mortality, and obesity, despite spending the highest percentage of its gross domestic product on health. A challenge for Healthy People 2030 is to guide the United States in achieving the population's full potential for health and well-being. As was recognized during the COVID-19 pandemic, the country was not ready for this type of public health emergency, and it is critical to learn from the experience to improve responses to future public health crises.
Figure 7-2 Healthy People stakeholders.
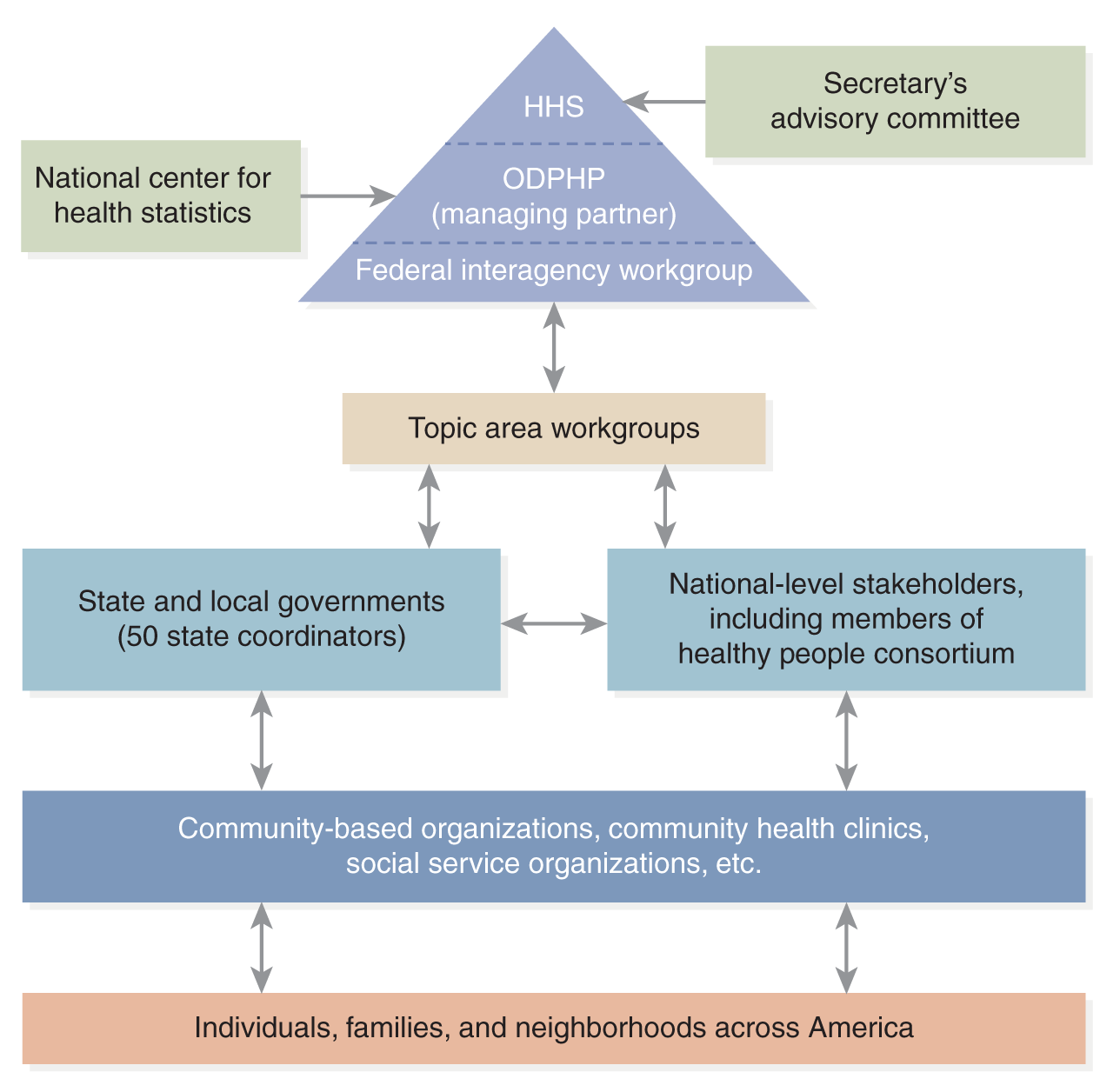
A hierarchical diagram of the organizational structure involved in the Healthy People initiative.
At the top is the U.S. Department of Health and Human Services, H H S, followed by its managing partner, the Office of Disease Prevention and Health Promotion, O D P H P, and the Federal Interagency Workgroup. Below this, there is the National Center for Health Statistics and the Secretary's Advisory Committee. The diagram further includes Topic Area Workgroups, State and Local Governments with 50 state coordinators, and National-level Stakeholders including members of the Healthy People Consortium. The base of the structure includes Community-based Organizations, Community Health Clinics, Social Service Organizations, and extends to individuals, families, and neighborhoods across America. This layout illustrates the flow of information and collaboration across different levels and sectors.
U.S. Health and Human Services (HHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). (2020) Healthy People 2030. https://www.cdc.gov/nchs/about/factsheets/factsheet-hp2030.htm
According to the Healthy People initiative, health status is determined by measuring birth and death rates, life expectancy, quality of life, morbidity from specific diseases, risk factors, use of ambulatory and inpatient care, accessibility of health providers and facilities, healthcare financing, health insurance coverage, and other factors. Healthcare accessibility is a critical and complex healthcare issue that affects the health status of individuals and communities, and it is now considered an important element related to diversity, equity, and inclusion (DEI), which is now referred to as DEIA, adding accessibility (HHS, ODPHP, 2023c). For example, when the causes of death in the United States are examined, there typically is not one single factor or behavior that determines outcomes but rather multiple factors-such as genetics, lifestyle, gender, race/ethnicity, nutrition, poverty level, education, injury, violence, and other factors in the environment, but unavailability or inaccessibility of quality health services is critical to ensure health across the life span. Data-driven national objectives are identified to meet the Healthy People framework goals. This includes multiple broad outcome measures used to assess the vision: (1) measurable core public health objectives with 10-year targets and related evidence-based interventions, (2) developmental objectives for public health issues with interventions, and (3) research objectives directed at public health issues for which there are no evidence-based interventions (HHS, ODPHP, 2023d). Review of the Healthy People website provides further understanding of these measurements and status of its data. Healthy People 2030 is interrelated with other federal initiatives, such as the annual National Healthcare Quality and Disparities Report (NHQDR) (HHS, AHRQ, 2023a), which is discussed in more detail in other chapters in this text.
A community is defined as a group of people that share a physical environment and services. Healthy People 2030 describes a healthy community as a community that maintains a high quality of life and is productive. This community is safe; provides both treatment and prevention services to all community members; maintains necessary effective infrastructure (access to food sources, water/power, roads, schools, playgrounds, transportation, fire and safety, law enforcement, and other services); and it is a healthy environment (concerned with issues, such as safe air and water, waste management, and so on). Educational and community-based programs need to focus on preventing disease and injury, promoting and improving health, and enhancing the quality of life. To meet Healthy People goals, community-focused programs and services need to provide broad access, for example, by offering programs in schools, workplaces, healthcare facilities, and community sites. These programs might offer services for health promotion and prevention, nutrition, exercise, monitoring health, and provide treatment and rehabilitation focused on a variety of needs, such as the following:
- Chronic diseases
- Injury and violence
- Bullying
- Mental health and illness
- Oral health
- Tobacco use
- Substance misuse (alcohol and drugs)
- Nutrition, physical activity, and obesity
Healthy People 2030 not only provides a plan in 10-year intervals to improve health care in the United States, but also monitors and reports on progress periodically during a 10-year cycle to determine if the goals and objectives are being met. Data on current outcomes can be found on the Healthy People website. When the 10-year period is completed, then all leading indicators are evaluated to assess the impact of the plan. The analysis of the outcome data is used to develop the goals, objectives, and leading indicators for the next 10 years. The current version for 2030 was developed at the conclusion of 2019-2020 version, so it is more than halfway through the 10-year cycle. Ongoing evaluation is very important and conducted to guide adjustments during the 10-year cycle, for example, changes made in objectives, and then, this guides healthcare policies and services. Nurses who work in a variety of settings can easily review the current data and consider how this information can be used to improve public/community health.
| Stop and Consider 1 |
|---|
| Healthy People 2030, a national health initiative, has implications for nursing care. |
Public/Community Healthcare Delivery System
The public/community healthcare delivery system is complex and varied with several levels: national, state, and local. These levels may not always be in sync though they should collaborate and coordinate to ensure positive community health outcomes. This section examines the system and its differences from the acute care system and how acute care and public/community health relate to support an overall health system for members of the community.
Structure and Function of the Public/Community Healthcare Delivery System
Public/community health has a critical role in improving and maintaining the health of individuals, families, and communities, focusing on the entire population. Public health focuses on issues related to policies, the public health workforce, financing and economics, structure of health organizations and performance within a community, information and technology, and advocating for public health needs. It is a complicated endeavor, requiring multiple services to meet population and community needs (APHA, 2023a). Public health nursing should be integrated into these services (ANA, 2023). There is a great need to address multiple complex health problems, some of which are related to social and economic problems in communities, such as violence, including domestic, child, and elder abuse; tobacco use; alcohol and drug misuse; injuries; automobile accidents; environmental factors such as air and water quality; food safety and consequent health issues; chronic diseases; and communicable/infectious diseases. Public health has recently become more important due to the increasing concern about disaster emergency management, terrorism, increasing violence, the opioid epidemic, and climate change leading to public health emergencies. The experience with COVID-19 has made it very clear that infectious/communicable diseases can have a major negative impact on all aspects of society. Communities need to develop effective plans to provide healthcare services in major crisis situations; for example, during the COVID-19 pandemic, communities had to quickly develop initiatives to implement testing and then vaccination. All these concerns require more than just care for individuals who are experiencing these problems; we need to look at populations and communities. Public health incorporates three main functions that relate to the 10 essential public health services, highlighted in Figure 7-3 (APHA, 2023a).
Figure 7-3 Public Health Core Functions and Essential Services.
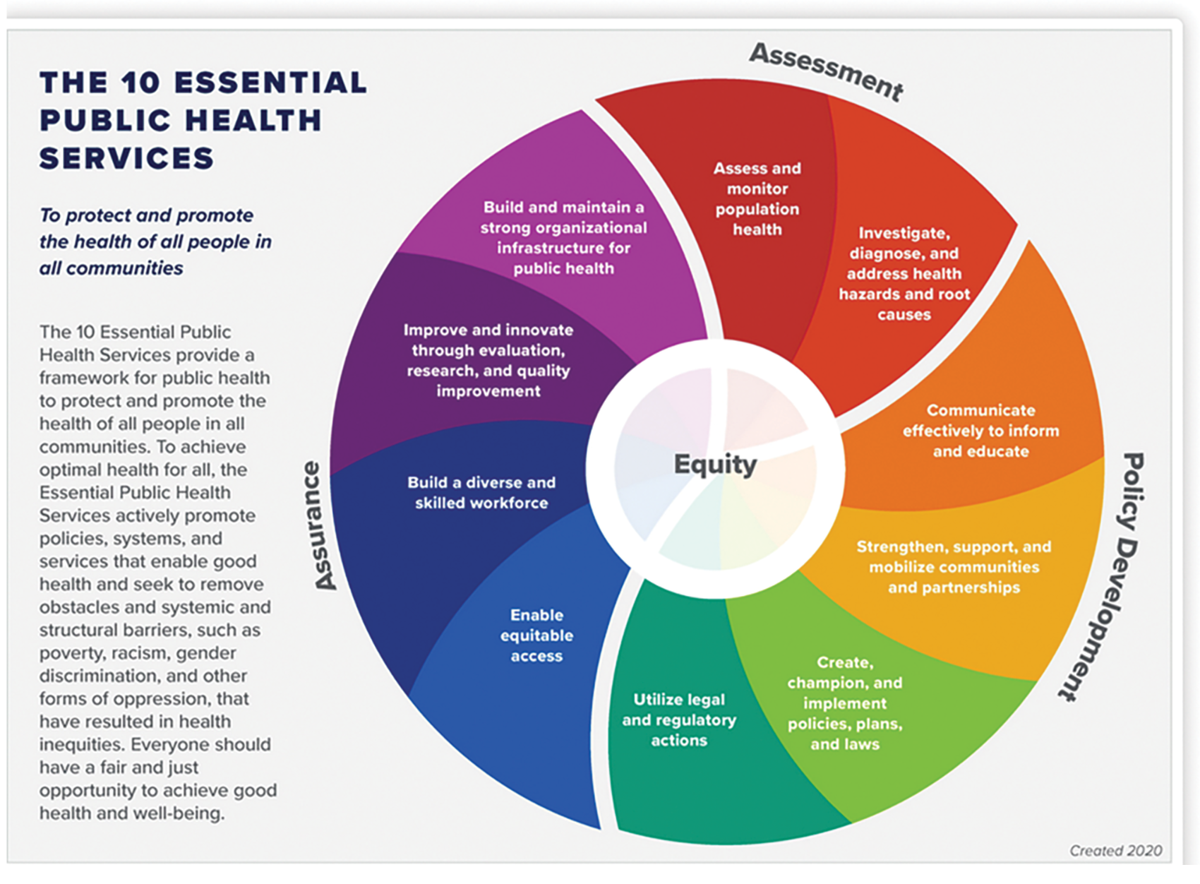
A circular diagram lists the 10 Essential Public Health Services focused on equity.
A circular diagram, segmented into ten sections, each representing a different public health service. These sections are grouped into three larger categories such as Assessment, Policy Development, and Assurance. At the center of the circle, there is a smaller circle labeled Equity, indicating the central focus of these services. It includes the following services: Assurance: Build and maintain a strong organizational infrastructure for public health. Assurance: Improve and innovate through evaluation, research, and quality improvement. Assurance: Build a diverse and skilled workforce. Assurance: Enable equitable access. Policy development: Utilize legal and regulatory actions. Policy development: Create, champion, and implement policies, plans, and laws. Policy development: Strengthen, support, and mobilize communities and partnerships. Policy development: Communicate effectively to inform and educate. Assessment: Assess and monitor population health. Assessment: Investigate, diagnose, and address health hazards and root causes. The framework aims to promote health and remove systemic barriers such as poverty, racism, and discrimination, ensuring equitable health opportunities for all. Text reads, To protect and promote the health of all people in all communities. The 10 Essential Public Health Services provide a framework for public health to protect and promote the health of all people in all communities. To achieve optimal health for all, the Essential Public Health Services actively promote policies, systems, and services that enable good health and seek to remove obstacles and systemic and structural barriers, such as poverty, racism, gender discrimination, and other forms of oppression, that have resulted in health inequities. Everyone should have a fair and just opportunity to achieve good health and well-being.
Centers for Disease Control and Prevention. (CDC). (2023). 10 essential public health services. https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html
- Assessment: Assess and diagnose the status of the community's health and identify service needs using epidemiology, surveillance, research, and evaluation.
- Policy development: Some problems require changes in laws, programs for prevention and treatment, and reimbursement for these services. Effective public health requires that the government and its agencies (local, state, and federal) and healthcare providers develop strategic plans, interventions, and appropriate evaluation of outcomes that are based on current policies.
- Assurance: Ensure universal access to care when it is needed for health promotion and prevention of disease and illness through community-wide health services.
The public/community healthcare delivery system is complex with the federal level influencing the state and local levels. At the federal level, the HHS along with its major agencies, such as the Centers for Disease Control and Prevention (CDC), the Food and Drug Administration (FDA), and the Public Health Service (PHS), have major responsibilities in ensuring the health of the nation and developing and implementing health policy based on evidence supporting best approaches to public/community health and requires collaboration with states and local health services. States and local communities (cities, towns, counties) vary as to how their public/community healthcare delivery systems are organized and the types of services they provide; however, services typically include monitoring population health and needs, health education, immunizations, environmental health issues (water, air, sanitation), transportation safety, food safety, maintenance of licensure for healthcare providers (such as physicians, nurses, hospitals, long-term care facilities, pharmacies, and others), clinic/ambulatory care services, disaster emergency planning, school health services, mental health and substance use services, social services, police and fire response, emergency response, and much more. Each state has a public health department or division, and typically counties and other local entities also have their own public/community health services. It is important that in all three levels of government public health services collaborate, coordinate, and communicate to ensure effective services and improve the public's health and safety. Local and state departments typically work closely together with the state government responsible for the public's health and safety within the state.
Nurses are very active in all types of public/community services, serving in administrative and planning roles at the federal, state, and local levels; assessing service needs; providing services in clinics and other state and local healthcare facilities; providing immunizations; providing guidance to control tuberculosis and other communicable diseases, particularly during times of epidemics or development of unexpected communicable diseases (most recently, for example, the Ebola virus and Zika virus outbreaks and the COVID-19 pandemic, and in the past human immunodeficiency virus [HIV]/acquired immunodeficiency syndrome [AIDS] prevention, assessment, and care); developing and implementing health promotion and disease prevention and education; providing home health care and hospice care; school health nursing, and occupational health nursing; conducting research in areas of public/community health; and participating in epidemiology activities. The role of the public health nurse has evolved and includes a greater focus on population-based health promotion and prevention (Kulbok et al., 2012). This role requires much more effective collaboration with a variety of organizations, healthcare professionals, and others in the community. Nurses who work in this area need to be able to collect and analyze data, develop plans and interventions, use a variety of interventions, such as typical nursing interventions (for example, health assessment and immunizations), and use different interventions (for example, implementing health education focused on population groups, involvement in planning health fairs, working with the local government to develop plans for disasters and other situations, ensuring effective and accessible school health care led by nurses, providing care in clinics and establishing nurse-managed clinics and collaborating with acute care, and so on) (Pilon et al., 2015). Nurses need to know how to motivate people in the community, such as the need for people to accept the COVID-19 vaccine or to use mitigation interventions, such as masking. The COVID-19 pandemic has emphasized an even greater need for effective public health nursing (Edmonds et al., 2020). It is clear that nurses need greater program planning skills, which require effective use of coordination, communication, and collaboration; for example, nurses may need to work with varied stakeholders, such as businesses, education, and religious organizations along with local government elected officials, to reach goals for a healthy community.
“The COVID-19 pandemic and what it has revealed about the effects of poverty, racism, and underinvestment in communities on health have illuminated the consequences of devaluing public health and underestimating the role that nurses can play in improving health and preventing disease. But if adequately valued and funded, public and community health nurses are uniquely positioned and trained to bridge health care and social needs and advance health equity. Strengths of community and public health nurses-team-based care, a holistic approach, community-centered care, advocacy, and more-are skills that will be key to ensuring everyone has what they need to be healthy and well. Investments that expand, strengthen, and diversify the community and public health nursing workforce will go a long way in advancing health equity for all” (NAM, 2021, pp. 1-2). This experience emphasizes that cultural competence is even more important in public/community health nursing than in acute care. In public/community health nursing courses students learn more about this critical area of health care and the roles of nurses and other members of the public/community health team (AACN, 2023a).
The American Association of Colleges of Nursing (AACN) also emphasizes the need for the inclusion of cultural competencies in baccalaureate and graduate nursing education and provides resources to meet this need and a faculty toolkit to integrate this content in nursing education programs (AACN, 2023a). The 2021 Essentials standards include concepts related to cultural competency: diversity, equity, and inclusion (DEI); and social determinants of health (SDOH), discussed later in this chapter, as well as in other text content (AACN, 2023b, 2023c). The National League for Nursing (NLN) also includes these critical topics in its accreditation standards (NLN, 2023). The NLN has joined with Walden University to form the Institute for Social Determinants of Health and Change recognizing the importance of nurses in addressing the SDOH and focuses on the following nursing activities (NLN & Walden University, 2021):
- Become leaders and catalysts of social change.
- Cultivate appropriate leadership competencies to integrate social change into their programs.
- Incorporate social determinants of health into their practice programs and/or curricula across undergraduate and graduate studies.
- Engage in research and other scholarly activities related to social determinants of health and social change with a view toward broad dissemination.
Continuum of Care
The continuum of care is an important concept in nursing and health care. In 2004, The Joint Commission (then called “The Joint Commission on Accreditation of Healthcare Organizations”) defined continuum of care as “matching an individual's ongoing needs with the appropriate level and type of medical, psychological, health, or social care or service within an organization or across multiple organizations” (p. 317), and this definition continues to be relevant. The continuum of care goal is to decrease fragmented care and costs and ensure care needs are met. The continuum includes health promotion; disease and illness prevention; ambulatory care, including ambulatory surgery/procedures without the need for inpatient stay; acute care; tertiary care; and public/community health needs, such as population health, home health care, long-term care, and hospice and palliative care. The continuum is a view of health care that describes a range of services in a variety of settings and different healthcare providers so that a patient receives care at different stages of health and illness based on needs and in a variety of settings.
Some hospitals have evolved into community health networks (Seegert, 2016). This is happening as hospitals are trying to determine how best to deal with a changing payment system, increasing costs, and the need to optimize patient outcomes and improve population health. Collaborating with others in the community-some who provide care and others who provide support services, funding, government structure and functions-may make the difference in meeting goals. Working in isolation, without collaboration, will not meet the goals. These hospitals are using nurses to help make greater connections with the community. “Rethinking health care requires a shift in the mindsets and skill sets of all who care for patients. It's less about episodes of care and more about an entire continuum of services” (Seegert, 2016, p. 19). Critical aspects of the continuum include the need for coordination, collaboration, communication, and the use of effective interprofessional healthcare teams to better ensure patient/person-centered care (PCC). These topics are discussed in other chapters of this text.
Continuity of Care
“Continuity of care is concerned with quality of care over time. It is the process by which the patient and his/her physician-led care team are cooperatively involved in ongoing health care management toward the shared goal of high quality, cost-effective medical care” (AAFP, 2023). This definition was developed after a multidisciplinary review of continuity of care literature to determine how different healthcare professionals viewed the concept, and healthcare providers continue to apply it today. Continuity of care is different from other views of care because it focuses on care over time and on individual patients to ensure that treatment is connected to needs as they change. Nurses are very involved in continuity of care when they transfer patients and coordinate care over time to better ensure consistency of care. Typically, this is done through discharge planning. Nurses who work in the community need to recognize the importance of continuity of care and integrate this into planning for individuals, families, and populations within the community. They need to recognize that care is based on a continuum, and acute care is often just one part of the continuum.
Individual, Family, and Community Health
Nursing students often assume that the patient is an individual, and most patients are individuals. There are, however, other views of the patient that are particularly relevant in public/community health: the family, the community, and specific populations, such as patients with specific chronic diseases.
Public health nurses often work with families in a community. “A family is a group of two or more persons related by birth, marriage, or adoption who live together; all such related persons are considered as members of one family” (HHS, HRSA, 2023a). Functional families are considered healthy families in which there is a state of bio/psycho/socio/cultural/spiritual well-being, and these families are responsive to individual family members. In contrast, dysfunctional families have poor communication and relationships with one another and do not provide adequate support to family members. Nurses work with families providing many different services needed along the continuum of care. The family itself may be the patient, or the nurse may be involved with a family because of one family member's illness. For example, a home healthcare nurse who is caring for a patient who has uncontrolled diabetes, recovering from surgery, and lives with her daughter and family must be aware of family dynamics, needs, caregiver strain, and other health issues that can impact the identified patient's care and outcomes, such as dietary changes and mobility. Family members may also be caregivers. A caregiver is someone who provides care to another person as a nonprofessional healthcare provider. Because many insurance plans provide limited or no coverage for home health care, families often need to serve as caregivers for the short-term or long-term needs of family members. From 2015-2020, caregiving increased from 16.6% to 19.2%, indicating a growing need in communities (NAC & AARP, 2020). The HHS considers caregiving by family and friends to be a public health issue (HHS, CDC, 2019). On September 21, 2022, the description of the 2022 National Strategy to Support Family Caregivers was shared with Congress (HHS, ACL, 2023). The strategy includes nearly 350 actions the federal government will take to support family caregivers in the coming year and more than 150 actions that can be adopted at other levels of government and across the private sector to begin to build a system that ensures family caregivers-who provide the overwhelming majority of long-term care in the United States and need resources to maintain their own health, well-being, and financial security while providing crucial support for others. The strategy was developed jointly by the advisory councils established by the Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act, which is a federal law signed in 2018, and the Supporting Grandparents Raising Grandchildren (SGRG) Act (2020), with extensive input from family caregivers, the people they support, and other stakeholders.
Family caregivers have long been the backbone of America's caregiving infrastructure, though informal in nature, but this has changed with its growing recognition. Each year, more than 53 million people provide a broad range of assistance to support the health, quality of life, and independence of someone close to them (AARP and National Alliance for Caregiving, 2020). Millions of older adults and people with disabilities would not be able to live in the community without this support. It is now recognized that replacing this caregiving with paid services would cost an estimated $470 billion annually (Reinhard et al., 2019).
When family members work and have other obligations, caregiving is not easy to do and there are problems that need to be considered. Serving as a caregiver for a family member on a long-term basis can lead to caregiver psychological, physical, social, and financial problems. Most caregivers are women; men are more likely to be cared for by their wives than the reverse because men have a shorter life expectancy (HHS, CDC, 2019). Caregiver strain is something nurses need to assess periodically to ensure that the caregiver(s), and typically this is the family, receive the support they need. Primary caregivers provide most of the daily aspects of care, and secondary caregivers help with intermittent activities (shopping, transportation, home repairs, getting bills paid, emergency support, and so on). Both types of caregiving can put a strain on the caregiver, but primary caregivers are at greater risk. There has been more focus on helping caregivers with information and support. In 2017, Tina Marrelli, a home healthcare nurse expert, developed an internet-based resource for caregivers (2023). Some healthcare providers and insurers offer access to this in-depth guide to caregivers for their patients and enrollees.
Nurses offer many services in communities, and they may focus on an entire community or a specific population that lives in the community. A population is a group of people who share one or more personal or environmental characteristics and may live in the same area, but this is not required; for example, a clinical research study may focus on a population of people who have diabetes, but they may not live in the same location. Population health focuses on health outcomes for a group of people, and this is an important consideration in public and community health (Finkelman, 2023a). Examples of populations within a community include children, older adults, people with a chronic disease, such as diabetes, cardiac, or respiratory disease, and people who lack safe and appropriate housing (unsheltered, unhoused). Nurses who work in communities may provide healthcare in schools; assess the needs of older adults in their homes; develop programs to screen for diabetes for people who live in the community and might be at risk; manage a health clinic for people who are unhoused; or participate in developing and implementing a community disaster emergency preparedness plan, collaborating with multiple community stakeholders. These are some of the ways that a nurse might assist different populations within a community, and depending on community needs, there are many other programs and services that might also involve nurses.
Access to Care
Access to care (accessibility) is the first step in receiving care, and it is not a simple process for many people; for some, there are major barriers. Access to care is a critical public/community health issue at the federal, state, and local levels. Many people think access only refers to the ability to physically get to a destination, but access to care involves many factors, such as:
- Ability to pay for care, either by insurance or personally
- Lack of insurer coverage for specific treatment or medications
- Lack of provider acceptance of the patient's insurance coverage
- Challenges to access, such as transportation: type (personal car, bus, train, and so on), schedules, parking, cost
- Clinical site hours of operation
- Wait time to get an appointment
- Long waits at the time of appointment to see a physician or other healthcare provider
- Ability to get an appointment via phone, internet, etc.
- Availability of type of healthcare provider and service needed
- Ability of the patient and provider to communicate and make use of accommodations for language, hearing, and sight
- Disability provisions at the healthcare site
- Timeliness of getting laboratory tests and receiving results
- Childcare provisions so that family members can go to appointments
- Cultural barriers
- Inadequate information or lack of information
- Lack of provider time (rushed)
As this list suggests, access is a complex issue, particularly for vulnerable populations.
Accessibility has a major impact on the continuum of care. Can the patient get the care that is needed when it is needed? Where is the best location for care? When patients experience access barriers, they may neglect routine care and put off getting care when it is needed. These patients may then need more complex care and use the safety net, which are services that cover patients who cannot pay for care or who have other access barriers. Examples of safety net sites include free clinics, academic health centers, and emergency departments. This type of care may (or may not) meet the patient's immediate need, and the care does not always effectively support continuity of care. Patients who experience the safety net process may get lost in the system, and their outcomes may not be positive. Public/community health services need to routinely assess the safety net system, improve these services, and communicate with the community so that they understand the services and access and get feedback from people who use the system. Recognizing the importance of helping this population, Healthy People 2030 includes this in its goals to improve the health of all groups (HHS, ODPHP, 2023d).
Another area that is receiving more attention is access to rural health care. These areas have experienced long-term problems in attracting healthcare providers, maintaining services, such as hospitals, and meeting other health need issues. The COVID-19 pandemic increased rural health service problems leading to HCO financial problems, such as more rural hospital closures or increased danger of closings (GAO, 2021). This reduction in hospitals and other health services leads to limited care access for the residents in these communities. If care is needed, residents may need to travel long distances for routine care and more complex care needs; for example, before the closure of a hospital, the community's residents traveled 4 miles to get to the hospital, and after the closure, they had to travel 23 miles for inpatient care. These changes in distances impact many service areas, such as emergency care, substance use disorder treatment, coronary care as well as inpatient care. COVID-19 increased the need for many of these services, for routine care and for COVID care. Access was critical but not always easy to obtain. Even before the COVID-19 immunization period, there were areas that struggled to get routine immunization services to community members. This all impacts the health of rural communities. An example of the complexity of rural health and increasing efforts to improve it is the 2024 Rural Health Care Leadership Conference, which highlighted the following concerns (AHA, 2024):
- Develop strategies for a more sustainable and flexible rural healthcare workforce.
- Promote the adoption of innovative approaches to improve quality, patient safety and performance in rural health care to enhance patient satisfaction, increase efficiency and reduce costs.
- Explore disaster preparedness and response plans specific to rural communities.
- Explore new models of care and payment that align with rural health care systems' needs.
- Elevate equity and eliminate disparities in treatment, access and outcomes.
- Advance community and population health and economic development in rural areas through collaborative efforts between healthcare organizations, public health agencies and community stakeholders.
- Share inventive approaches to mergers, joint ventures and affiliations to help improve financial stability, operational efficiency, and clinical outcomes.
- Learn how advances in telehealth, information technology, and artificial intelligence are improving access in rural communities.
- Share best practices in health care delivery for American Indians and Alaskan Natives.
- Highlight best practices for achieving governance excellence in rural health care organizations, including effective leadership, stakeholder engagement, and accountability.
One approach to improving healthcare public/community service access is to offer comprehensive and wraparound services. Comprehensive services are best described as “one-stop shopping”-the patient can go to one location and receive multiple services. These services are typically offered in convenient locations, such as in neighborhoods, schools, or work sites. Health promotion and illness prevention are also integrated into these services. Recognizing that social and economic problems have a major impact on a person's health and access to needed services (social determinants of health), wraparound services can be combined with comprehensive health services within the healthcare site by also offering social and economic services (for example, when a patient comes in for a healthcare appointment, there is access to a social worker to assist with problems, such as food assistance and housing, job issues, and access to healthcare reimbursement, and the site may even offer legal aid services).
Another critical factor that has a major impact on access to care is the ability to pay for care, typically with some type of insurance. The Affordable Care Act (ACA) focuses on this issue, although its implementation does not mean all citizens have insurance (universal health insurance). The overall goal of the ACA is to reduce the number of people without health insurance in the United States. The ACA has made it easier for some people to get health insurance, especially given that the law provided some financial support to help some people cover the cost. The law initially required persons without health insurance to pay penalties. This carrot-and-stick strategy represented a complex approach to the problem, and this approach was challenged by the Trump administration. Changes were made, and the mandate for coverage and penalties were eliminated. Due to possible future changes in ACA that may occur in later presidential administrations it is important for nurses to keep up to date in healthcare policies and consider the impact changes might have on nurses, nursing care, and health care in general.
The ACA includes provisions supporting the establishment of accountable care organizations (ACOs). This type of HCO focuses on containing healthcare costs by supporting patient care sites and services that emphasize care coordination across disciplines to provide integrated care delivery (HHS, CMS, 2023a). It is unclear what effect changes in the ACA might have on provisions such as this one, but since the law was passed, the CMS has further developed the ACO model, making changes over time to improve ACO services and providing guidance for implementing these services for its beneficiaries (HHS, CMS, 2023b). Nurses provide ambulatory care nursing in ACOs, and nurse practitioners also hold important positions within ACOs.
Medicare ACOs are comprised of groups of doctors, hospitals, and other health care providers and suppliers who come together voluntarily to provide coordinated, high-quality care at lower costs to their Medicare patients. ACOs are patient/person-centered organizations where the patient and providers are true partners in care decisions. Medicare beneficiaries have better control over their health care, and providers have better information about their patients' medical history and develop better relationships with patients' other providers. Provider participation in ACOs is purely voluntary, and participating patients see no change in their Medicare benefits and have freedom to see any Medicare provider. When an ACO succeeds in both delivering high-quality care and spending healthcare dollars more wisely, it shares in the savings it achieves for the Medicare program, which acts as a financial incentive to improve services. (HHS, CMS, 2023b)
Across the Life Span
Patients may enter the healthcare system for a variety of needs and services and enter at any point in the life span from:
- Conception
- Birth
- Infancy
- Childhood
- Adolescence
- Young adulthood
- Middle adulthood
- Older adulthood
- End of life
Each of these life-span periods includes specific health concerns and needs, as well as potential disease and illness risks. In addition, social and psychological experiences during these time periods affect health and wellness. These experiences include situations such as a change in or loss of a job and other financial problems, beginning school, moving, marriage, the birth of a child, divorce, the need to care for a family member who is ill, the death of a loved one, chronic illness experience, retirement, and other stressful situations. The federal government collects data about health and illness across the life span. Exhibit 7-2 identifies the leading causes of death, and these causes have an impact on public/community health status. The data are updated periodically by the CDC on its website, though the data are typically 1 to 2 years behind the current year.
| Exhibit 7-2 Leading Causes of Death in the United States |
|---|
|
An example of a population group that has always been important but became more important during the COVID-19 pandemic, is older adults (people 65 years and older). During the pandemic, this population group was at high risk for serious health problems and experienced high mortality rates. In addition, they experienced major problems with recommended social isolation to reduce exposure, which led to limited or no contact with regular out-of-home routines, such as social events, shopping, getting prescriptions, and so on; separation from family; limited typical exercise, such as walking and use of gym; and so on (IHI, 2021). This experience has emphasized the greater need to develop age-friendly health systems (IHI, 2023a). This type of system focuses on what matters related to older adult needs, outcome goals reflecting these needs, older adult preferences, and medication that meets health needs but also considers mobility and mentation across care settings, such as daily safe mobility, nutrition, maintaining function, and meeting social needs. Developing age-friendly health systems requires changes in healthcare delivery and in healthcare provider practice. Demonstrating the increasing interest in this area the Institute for Health Improvement offers resources to healthcare providers and organizations to provide effective age-friendly care (IHI, 2024).
Health Promotion and Disease Prevention
Even though the United States spends more on health care than most countries its citizens are the less healthy, compared to other developed countries. Chronic disease is a major factor that affects this outcome; chronic illness is often connected to unhealthy lifestyle behaviors. The American Hospital Association developed an initiative describing a road map for improving America's healthcare system, focusing on wellness rather than acute care, which is important in public/community health. The initiative's goals are “Health for Life: Better Health. Better Healthcare,” which continue to be relevant and include the following issues (AHA, 2017):
- Focus on wellness
- Most efficient, affordable care
- The highest quality care
- Best information
- Health coverage for all; paid by all
Health Promotion
In 1976, the U.S. Congress created the Office of Disease Prevention and Health Promotion (ODPHP). This is part of the HHS and “plays a vital role in keeping the nation healthy. We accomplish this by setting national public health objectives and supporting programs, services, and education activities that improve the health of all Americans. Our site includes information about Healthy People 2030 and evidence-based, actionable health information for consumers from MyHealthfinder” (HHS, ODPHP, 2023e). Health promotion focuses on changing lifestyles to maximize health and is an important part of primary prevention. Healthy lifestyle choices help individuals and communities improve and maintain health-eating a nutritious diet, being physically active, making healthy choices, and getting preventive screenings-to help prevent major health threats and burdens, such as diabetes, asthma, cancer, heart disease, and stroke. Most people have difficulty making changes and maintaining them, and it is challenging for public/community health initiatives to address these responses.
Many models describe how health promotion might be effective. Pender's health promotion model is a nursing model that has been used in many health promotion studies (Pender et al., 2006). This model that can be applied across the life span does not include fear or threat as a motivator to make people change their behaviors. Pender's health promotion model includes individual characteristics and experiences, emphasizing that each person is unique. The following aspects of health promotion have an impact on health and continue to be relevant today (Pender et al., 2006):
- Prior related behavior: The frequency of the same or similar behavior in the past is the best predictor of behavior.
- Personal factors: Biological (age, weight, pubertal status, and strength), psychological (self-esteem, coping style, and self-motivation), and sociocultural (race, ethnicity, education, and socioeconomic status) factors may influence the cognitions, effects, and health behavior.
- Behavior-specific cognitions and affects: These cognitions and affects are very important because nursing interventions can change them, which can in turn move a person toward health-promoting behaviors.
- Perceived benefits of action: Whether a person will be active in participating in changing behavior is highly dependent on whether the person sees any benefit in doing so-that is, whether there are perceived benefits. It is important to determine whether perceived barriers are real. If perceived barriers to success are felt by a person, it is much more difficult for that person to change a behavior to a health-promoting behavior.
- Perceived self-efficacy: Self-efficacy relates to whether a person feels that it is possible to do what is needed. It does not mean that the person has the competency to do this but rather centers on whether the person feels that he or she could do what needs to be done.
- Activity-related affect: Emotions tied to actions are important to recognize, because they can determine whether a person repeats a behavior. Did the person feel good about what he or she did? Did it make the person anxious?
- Interpersonal influences: A person is influenced by others, family, friends, coworkers, peers, healthcare providers, and so on. This influence-what it might be and how it might be felt-may or may not be reality based, but it still can influence a person's behavior and the person's ability to change to health-promoting behavior.
- Situational influences: A situation or context can influence a person's behavior. If a person smokes and is told that all smoking must take place outside the building in a designated area regardless of the weather, this situation or context may influence a change in behavior.
- Commitment to a plan of action: Is a person committed to a specific plan to change to health-promoting behavior? Commitment is not enough; strategies must be laid out that will enable the person to reach the desired outcomes.
- Immediate competing demands and preferences: What might interfere with a person changing to health-promoting behavior? Will the family be supportive? Are there other actions that must take precedence (for example, work over exercise)? Each person has alternative behaviors that compete with what the person needs to do to change to a healthier lifestyle.
- Health-promoting behavior: This is the outcome, and from this, a person reaches positive health outcomes.
Disease Prevention
Disease prevention is concerned with interventions to stop the development of disease and treatment to prevent the disease from progressing further and leading to complications. The three major levels of prevention are primary, secondary, and tertiary. The levels continue to be relevant; for example, they are used by the CDC (Leavell & Clark, 1965):
- Primary prevention includes interventions that are used to maintain health before illness occurs. Health promotion is a critical component of primary prevention. Examples are teaching people (children and adults) about healthy diets before they become obese and encouraging adequate exercise; education about health and healthy lifestyles is an important intervention at this level.
- Secondary prevention identifies and treats disease/injury in a timely manner to prevent or slow the progress of the health problem. Examples are breast cancer screening using mammography and blood pressure screening to diagnose hypertension.
- Tertiary prevention occurs when there is a disability and the need to maintain or, if possible, improve functioning. Examples are teaching a person with diabetes how to administer insulin and manage the disease or referring a stroke patient for rehabilitation or providing long-term home care.
In 2011, the Office of the Surgeon General initiated the National Prevention Strategy, which aims to guide the United States in improving the health and well-being of its population. The strategy prioritizes prevention by integrating recommendations and actions across multiple settings to improve health and save lives (HHS, OSG, 2011). The initiative includes “actions that public and private partners can take to help Americans stay healthy and fit and improve the nation's prosperity. It identifies the following four strategic directions that, collectively, are fundamental to improving the nation's health” (HHS, NIH, 2020):
- Building healthy and safe community environments: Prevention of disease starts in communities and at home, not just in the physician's office.
- Clinical and community preventive settings: When people receive preventive care, such as immunizations and cancer screenings, they have better health and lower healthcare costs.
- Empowered people to make healthy choices: When people have access to actionable and easy-to-understand information and resources, they are empowered to make healthier choices.
- Elimination of health disparities: By eliminating disparities in achieving and maintaining health, the goal is to improve quality of life for all Americans.
Several initiatives related to health promotion and disease prevention are identified in this chapter, and they are connected. For example, Healthy People, some of the ACA provisions, and the National Prevention Strategy focus on both individuals and their communities. Another theme that runs through these initiatives is the need to provide PCC. Prevention priorities to ensure healthy communities typically include:
- Tobacco-free living
- Preventing substance use
- Healthy eating
- Active living
- Injury- and violence-free living
- Reproductive and sexual health
- Mental and emotional well-being
| Stop and Consider 2 |
|---|
| Nurses can make a positive impact on public/community health. Nurses are involved in CDC initiatives focused on prevention and addressing health problems, such as (2022a): |
|
Important Concepts
Public/community health care includes several concepts that may not be found in acute health care, may be viewed differently when considered to be part of public/community health, or may receive less emphasis in acute care. For example, the public/community healthcare team may include different members from acute care. Some may not be healthcare providers but rather government officials and staff from social service agencies. The following sections discuss some of these concepts.
Patient as Focus of Care and Member of the Healthcare Team
The patient is always the focus of care, even when the larger community is considered. Patients should be viewed as members of the healthcare team and involved in decision-making about their own care with the patient at the center of the care process, which requires greater emphasis on PCC. This point does not just apply to individual patients. As noted earlier, in public/community health the patient may be an individual, family, population, or the community and involve different types of healthcare delivery services from private and public healthcare sectors. All should be part of assessment, planning, and decision-making. If this does not happen, the public/community health efforts are at risk of failure. Public/community health initiatives are more successful when community members participate in the planning and evaluation of programs and their services. This is demonstrated regularly, for example, in local community health departments and city and county government meetings that discuss and plan to address community water and air quality, health needs, cost of school nurses, transportation safety, and so on. Community members (elected officials, and residents-taxpayers and voters) participate in this process as stakeholders concerned about issues that relate to health and services in their communities. In some cases, these issues may be on ballots as legislation/policy and part of election campaigns-the overall goal should be a healthy, safe community for all.
Social Determinants of Health
A critical concern today in health care is SDOH that affect an individual's health status. The World Health Organization (WHO) describes SDOH as “[t]he conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, and political systems” (2023a). When we consider these determinants, we are looking at social and community policies, cultural and social norms, political issues and systems, diversity and equity, and disparities. We need to use partnerships to address social determinants-they cross many community areas and concerns. It is also important to ensure that healthcare professionals are better prepared-offering more content and learning experiences about the SDOH in academic health professional programs and include this topic in healthcare staff education as part of lifelong learning (NAM, 2016). To address SDOH, staff need to collaborate and coordinate across different sectors of society, such as government, business, education, social service agencies, religious institutions, and so on, emphasizing the importance of interprofessional teams to address SDOH. Figure 7-4 highlights SDOH as viewed by the HHS and its agency the CDC.
Figure 7-4 Social determinants of health at CDC.

A diagram of social conditions and structural conditions of health emphasizing various contributing factors and their interconnections.
This diagram provides a structured view of the social determinants of health, represented by a central circle labeled social conditions, structural conditions, and S D O H. Surrounding this are several linked elements that impact these determinants: Policy and Law, Data and Surveillance, Evaluation and Evidence Building, Partnerships and Collaboration, Community Engagement, and Infrastructure and Capacity.
Centers for Disease Control and Prevention (CDC) (2022). Social Determinants of Health at the CDC. https://www.cdc.gov/about/sdoh/index.html
Diversity, Equity, Inclusion, and Accessibility
Health disparities have become even more important in the last 10 years (Finkelman, 2023b). The IOM, now known as the NAM, Quality Chasm report series includes reports that describe supporting data demonstrating the severity of the U.S. healthcare system problems associated with health/healthcare disparities (IOM, 2002). A health disparity is “an inequality or gap that exists between two or more groups” (HHS, CDC, 2023b). Health equity occurs “when everyone has the opportunity to be as healthy as possible” (HHS, CDC, 2023b). President Biden signed Executive Order 14035, Diversity, Equity, Inclusion, and Accessibility in the Federal Workplace on June 25, 2021. “This action established a government-wide initiative to advance diversity, equity, inclusion, and accessibility (DEIA) in all parts of the Federal workforce” (HHS, 2022). This action is significant for federal services but also has an impact on local and state governments as they too are now focusing on DEIA. HCOs are also integrating this approach, including diversity, health equity, inclusion, and accessibility as strategic priorities guided by leadership (Finkelman, 2023b). This requires structure, processes, and strategies to address multiple SDOH and meet patient needs across many spectrums (WHO, 2023a). Health disparities are believed to be the result of the complex interaction of personal, economic, societal, and environmental factors. HCOs need to address and reduce racism within HCOs and develop effective partnerships in communities to meet this goal (IHI, 2023b, 2016; Finkelman, 2023b). Racism must be considered in healthcare delivery and in the healthcare workforce. This term refers to “a system consisting of structures, policies, practices, and norms-that assigns value and determines opportunity based on the way people look or the color of their skin. This results in conditions that unfairly advantage some and disadvantage others throughout society” (HHS, CDC, OMHHE, 2021).
“Most agree health disparities are a moral problem. Yet there are disagreements about how to reduce them. Some believe that in health systems, equity and efficiency are incompatible, requiring stark and painful tradeoffs,” but improving efficiency can make a difference in health outcomes (Anderson, 2023). Efficiency should involve distributing resources in the best way possible, best use and time. Paying attention to this also impacts opportunity cost; for example, health disparities increase health burden, medical care, lost productivity, and premature death. These issues are now important factors as health care is planned, delivered, and evaluated to ensure DEIA is part of the healthcare delivery system and healthcare professions.
As healthcare systems address racism and related issues, health literacy is an important factor connected to DEIA, discussed in more detail later in this section. It is relevant to all segments of the population, though it disproportionately impacts racial and ethnic minorities, increasing the risk of disparities (Bau et al., 2019). The Healthy People 2030 initiative considers measures of race/ethnicity, gender, physical and mental ability, and geography. Another federal initiative, the National Healthcare Disparities Report, is now combined with the National Quality Report and called the National Healthcare Quality and Disparities Report (NHQDR). This change recognizes the connection between disparities and quality, particularly the effects of race, ethnicity, socioeconomic status, age, sex, disability status, sexual orientation, gender identity, and residential location. The NHQDR provides annual summaries of the status of health and healthcare delivery in the United States since 2003. “The NHQDR team prioritizes reporting data and measures that are broadly representative of the performance of the nation's healthcare system over time. The NHQDR content provides policymakers, health system leaders, and the public with a statistical portrait of the effectiveness of the healthcare delivery system in providing safe, high-quality, and equitable care to all Americans. It addresses the question, how successful is the nation in ensuring that people benefit from the scientific advancements and effective treatments available today? Multiple partners, including agencies throughout the Department of Health and Human Services and all states, contribute data for the report, which is submitted each year to Congress by the Secretary of HHS” (HHS, AHRQ, 2022): The 2022 NHQDR reports on more than 440 measures of quality and examines data in three sections:
- Portrait of American Healthcare provides a healthcare system overview, including descriptions of leading health concerns and the healthcare delivery system's capacity to address them.
- Special Emphasis Topics examine quality of care and disparities in four priorities: maternal health, child and adolescent mental health, substance use disorders, and oral health.
- Quality and Disparities Tables group data into one of seven topic-related chapters, systematically summarizing the nation's healthcare outcomes for each measure.
The NHQDR can be accessed online to review the above data and analysis and its chartbooks that provide detailed reviews of health status based on the NHQDR framework (HHS, AHRQ, 2023a).
In early 2021, the National Institutes of Health (NIH) initiated a critical discussion and actions related to structural racism, which impacts disparities and health equity and plans to improve. Historically, racism has led to the marginalization and oppression of Indigenous peoples, African Americans, Latinos, and other communities of color. This discrimination has extended to sexual and gender minorities. “Structural racism has resulted in persistent health disparities, poor health status, and premature mortality as demonstrated by the current disproportionate burden of morbidity and mortality from COVID-19. Within the biomedical research enterprise, structural and institutional racism has resulted in inequitable access to funding, training, and workforce opportunities. The NIH is in a position of influence to contribute to positive, visible, and sustainable change to break the cycle of institutional racism with systems, policies, social norms, and practices that remove stereotypes and mitigate the pervasive effects of racism. We must practice science in a way that ensures employing the full breadth of talent and with attention to any unintended consequences of our research that might amplify health disparities” (HHS, NIH, 2021a), This growing problem is also now discussed in nursing literature, noting the need for the profession, practice, and education standards to also address it (Jolly & Peck, 2022; AACN, 2021; Gold, 2021; Villarruel & Broome, 2020; ANA, 2018).
Vulnerable Populations
A vulnerable population is a group of persons who are at risk for developing health problems. These populations often have problems accessing care when they need it. Examples of vulnerable populations are children, older adults/elderly, people with chronic disease, people who experience disabilities, for example, limited mobility/hearing/sight and others, immigrants, illegal aliens, migrant workers, people who live in rural areas, unhoused, the serious mentally ill, victims of abuse and violence, pregnant adolescents, people who misuse alcohol and drugs, and people who are HIV positive. Children as a vulnerable population needing care within communities requires careful assessment and monitoring to identify problems early so that complications can be prevented and support positive growth and development outcomes. Typically, complex factors, such as physiological, psychological, economic, ethnic, religious, social, cultural, and communication increase risk, referred to earlier as SDOH and are connected to problems related to nutrition, housing, safety, education, and transportation, and other problems that may impact health.
Poverty is an important concern, which has a significant impact on public/community health for individuals, families, populations, and communities. Prior to 2020, there was some improvement in household income and health insurance coverage (U.S. Census Bureau, 2022). However, the short-term and long-term impact of the COVID-19 pandemic is not yet known, but many people lost their jobs temporarily or long term, experienced changes in work hours decreasing income; some businesses closed or experienced reduced income; some people experienced food access problems; health insurance coverage problems influenced healthcare services needed for non-COVID-19 health problems; debt increased from home costs or lost homes; and some postponed higher education opportunities and had an impact on career goals. All of this has a short- and long-term impact on poverty levels and on healthcare delivery. Poverty guidelines are important because financial eligibility for certain federal programs is based on poverty levels. To receive specific services from government sources, a person must not have an income higher than the poverty level. The HHS identifies the poverty guidelines, which are reviewed and usually changed annually, posted on the HHS website (HHS, ASPE, 2023).
Health and Illness
“Health” and “wellness” are terms that tend to be used interchangeably, but what does “health” mean? There is no simple response to this question. A simple definition of health is to be structurally and functionally whole. Absence of this state is illness. “Disease” and “illness” are terms that are often used interchangeably. Disease is an indication of a physiological dysfunction or pathological reaction. WHO defines health as
a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. The bibliographic citation for this definition is: Preamble to the Constitution of WHO as adopted by the International Health Conference, New York, 19 June-22 July 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of WHO, no. 2, p. 100) and entered into force on 7 April 1948. The definition has not been amended since 1948. (WHO, 2023b)
This is a common definition and one that is often quoted. The WHO focus areas are global and include universal health coverage, health emergencies, health and well-being; noncommunicable disease prevention, mental health promotion, climate change, antimicrobial resistance, and elimination and eradication of high-impact communicable diseases (WHO, 2023c).
According to the Organization for Economic Co-operation and Development (OECD), life expectancy at the time of birth in the United States in 2019 was 76.2 (OECD, 2023). COVID-19 has had a major impact on morbidity and mortality data globally, but the data are not yet fully applied in analysis of current health status globally. The following data compare the United States with OECD countries (OECD, 2023):
- The United States spends much more on health than other high-income countries-both on a per capita basis and as a share of gross domestic product (GDP).
- Prices in the health sector tend to be high in the United States, which helps to explain the high health spending, although the use of certain health goods and services may also be high. Most countries, health spending is primarily financed either by government out of its tax revenues, or by health insurance paid for through social security contributions. Taken together, these types of financing schemes fund three-quarters of all healthcare spending in OECD countries. Healthcare funding in the United States is different with more provided by private sources and private health insurance.
In terms of value for money, the United States does well on some measures of healthcare quality, while not so well in others. Some factors that indicate differences from other OECD countries related to risk for health problems: The United States has a lower rate of smoking; population aging is less than many other countries; the United States has a higher rate of overweight and obesity. Another factor is the quality of care; however, it is difficult to confirm that it is better in the United States. Does the United States get value for what it spends? The answer is not clear. The United States does better on some international measures of healthcare quality, while not so well in others. In terms of outcomes, some mortality and morbidity measures are below average in the United States, although this can be due, to an extent, to factors outside the health system's control.
Many countries have universal health coverage, but this is not the case for the United States. This factor has an impact on the data presented previously. The U.S. Census Bureau publishes data about health statistics specific to the United States (2023, 2022). This type of data is used in public/community health to assess the status of health in communities and then determine the needs for health promotion, disease prevention, and treatment services, followed by the development, implementation, and evaluation of services. It also affects other types of services, such as projecting housing, education, and employment needs; for example, a community of older adults requires different community services compared to a community composed of young families.
Stress, Coping, Adaptation, and Resilience: A Public/Community Perspective
Stress is a complex experience, which is felt internally, as discussed in other chapters pertaining to students and individual nurses in practice, and it can lead to a feeling of loss or threat of a loss. Stress is present in all parts of life, and it influences current health status and can lead to long-term health problems or make health problems worse-for example, a patient with a cardiac problem may exhibit more cardiac symptoms when experiencing high levels of stress; patients who have socioeconomic problems may not have an adequate diet because of lack of money, or they may experience sleep problems because they work two jobs-all factors that increase stress. Not all people who experience stress have negative outcomes. In this chapter, the content focuses more on communities experiencing stress-for example, stress can be caused by economic problems, such as lack of employment and high poverty level, inadequate or unsafe housing, lack of critical healthcare services, increase in violence or crime, or inadequate education for children. The COVID-19 pandemic is an example of the overwhelming impact this type of experience can have on communities of all sizes and economic levels and countries, increasing community stress. Climate can also increase stress in communities, for example, extreme temperatures, winter snowstorms, floods, water shortages, tornados, hurricanes, fires, and so on. During hot weather, some urban communities experience more violence among adolescents and young adults, and people who may be outside more due to heat experience. Heat in the summer of 2023 was a major climate and health problem globally, for all ages and many communities, impacting the economy, availability of electricity and water, availability of cool safe shelter, the number of dangerous fires, and much more. As school began in the fall, many schools that opened in August and September found that not having air conditioning led to problems, with some schools even closing, delaying start dates, or changing their hours. Many communities were not prepared for this climate emergency, and this problem of extreme temperatures is expected to continue. Nursing includes these concerns more in its community/public health education and they have become part of community/public health practice, for example, addressing problems and responses to extreme weather events, air pollution, water-borne diseases, vector-borne diseases, food insecurity, mental health/stress, allergies and respiratory diseases, displacement, and skin cancer (Morris, 2023).
The most effective intervention for stress is stress management, which can be applied to individuals and to communities and should be considered as a preventive method with increased use during times of potential stress risk. Earlier content discussed student stress, but here we focus on how stress impacts others. Eliminating stress completely is not possible, but helping individuals, families, vulnerable populations, and communities cope better with stress is an important goal in improving health and developing health-promoting behaviors. Using effective coping measures routinely can reduce the negative impact of stress and, in many cases, prevent a person, family, or community from experiencing stress. This might be done by identifying stressors or stimuli that cause a community to experience stress. Stressors can be biological, sociological, psychological, spiritual, or environmental. Using self-assessment to identify stressors is critical to improve coping, and this can be done by individuals, as discussed in other chapters, but also by communities. For example, a community should collect and analyze local data about suicide, accidents, and requests for certain services, such as mental health, alcohol and drug misuse, violence and crime, unemployment, housing problems, bullying problems in schools, and so on. The goal is to understand the community's stress level, and use prevention and interventions to reduce it. Stress management interventions might include community education so that residents understand stress and the application of interventions and offer residents resources to reduce stress. Other community-oriented interventions to make people feel safe and reduce violence might include providing places for teen after-school activities; increasing collaboration with law enforcement with healthcare providers and schools; increasing access to community clinics including mental health services for all ages; assessing and responding to substance use such as drugs and alcohol; increasing job training and jobs; improving neighborhoods; improving housing and making it more available; improving transportation to areas where healthcare services and other needed services are available and access to schools, employment, and social activities; providing parenting classes; and increasing exercise classes and social activities in community centers. Resilience, or the ability to cope with stress, is an important factor. Just as individuals can develop resilience so can communities-sometimes you hear people interviewed on the news after a disaster, such as a tornado, and they describe how the community is coming together, helping one another, and they will survive. This is resilience. Adaptation to situations is also important in stress prevention and management. Listening to the community is a critical element in understanding stress but also provides guidance in preventing and responding to stress. The same principles of stress apply to everyone, including patients-individuals, families, and communities. The COVID-19 pandemic was a situation of high community stress along with stress for individuals and families. Coping was difficult, and some communities are now better prepared to handle the many needs that occur in a public health emergency and move forward by actively and routinely integrating stress management as a significant part of their future public/community health plans and ensuring it is addressed during times of public health crisis.
Acute Illness
Acute illness is typically self-limiting and occurs over a short period of time. Cure is the focus of acute care, though some acute illnesses may not be cured and then may result in a chronic illness or death. Some health care for acute illness takes place in the hospital, commonly referred to as the “acute care setting,” but today, more care is taking place in the patient's home in the community through primary care and ambulatory services, home health care, digital health (telehealth/telemedicine), and other community services and in other facilities that are not acute care; for example, a patient may go to a rehabilitation center for a short stay after complex orthopedic surgery. Examples of acute illnesses are infectious diseases, such as the flu or pneumonia, a broken leg, appendicitis, and a urinary tract infection.
Greater Emphasis on Chronic Disease
With the increase in the number of people with chronic diseases and the increasing older adult population, cure is becoming less important for some patients' daily perspective. There is more focus on functioning at the best possible level. The curative model focuses more on the biological approach, which relies on a hierarchical system of decision-making in which physicians make diagnoses and order treatment. Nursing is more involved in other functions, although the nurse certainly participates in providing nursing care that is directed at cure, such as assisting in surgery to repair a fractured hip. The hip can be repaired, but the patient typically has other needs after this surgery that are related to other functions. The patient will need help gaining functional capacity, and some patients may not regain full capacity and require support in coping with a change in long-term health status. The patient may require help with health promotion if the cause of the fracture was osteoporosis, for example, lifestyle changes related to diet, vitamins, and exercise. These factors need to be considered in follow-up care in the community.
Patients with chronic diseases need PCC. In the United States, the total number of persons with chronic diseases has increased, as has the number of people with more than one chronic disease. Many of these diseases are preventable. Six in 10 Americans have one chronic disease, and 4 in 10 have two or more, particularly, heart disease, cancer, chronic liver disease, stroke, Alzheimer's disease, diabetes, and chronic kidney disease. Ninety percent of the U.S. $4.1 trillion in annual healthcare costs is due to care for people with chronic and mental health conditions (HHS, CDC, 2023c). Some factors that impact these diseases in the community are tobacco use, poor nutrition, lack of physical activity, and excessive alcohol use, and in some cases, drug use. Over time new health problems arise, problems that on initial experience were not viewed as chronic are now chronic and require different perspectives on treatment, for example, concern about long-term effects of having had COVID-19.
The CDC is actively working to learn more about the whole range of short- and long-term health effects associated with COVID-19. As the pandemic unfolded, it was recognized that many organs besides the lungs are affected by COVID-19, and there are many ways the infection can affect someone's health. While most persons with COVID-19 recover and return to normal health, some patients can have symptoms that last for weeks or even months after recovery from acute illness, and for some it may be longer. Even people who are not hospitalized and experience only mild illness may experience persistent or late symptoms. Multi-year studies are underway to further investigate the impact of this virus. The CDC continues to work to identify how common these symptoms are, who is most likely to get them, and whether these symptoms eventually resolve. (HHS, CDC, 2022b)
Patients with these postvirus problems are referred to as “long haulers” and have developed problems related to cardiovascular disease, for example, inflammation of the heart muscle; respiratory (e.g., lung function) abnormalities; acute kidney injury; dermatologic problems, such as rash, hair loss; and neurological problems, particularly smell and taste problems, sleep issues, difficulty with concentration, memory problems; and mental health concerns, such as depression, anxiety, and changes in mood. It is not clear yet the impact these results will have on individuals, families, and communities and what communities will need to do to ensure care is provided as needed for these problems, but it is recognized that some patients are not back to full functioning. In addition, communities need to consider problems that occurred beyond health, such as problems related to unemployment, failed businesses, access to housing, limited or lack of health insurance, increase in crime, increase in alcohol and drug misuse, and other social concerns, which impact stress levels and health. Due to this increasing concern, WHO is working on a clinical description for these “long-hauler” problems that are not resolved after the initial COVID-19 illness (Carbajal, 2021). In February 2021, the NIH issued a call for research focused on these problems, recognizing that this is a significant problem, and it will be a long-term problem for the healthcare system and the social system (HHS, NIH, 2021b).
One reason the United States has problems with increasing chronic disease is that there is better treatment today, so people with chronic diseases live longer; consequently, there are more people with chronic diseases. A second reason is that the United States still needs more care improvement for chronic diseases and coping with a greater number of patients, and there are special needs for patients with multiple chronic illnesses. Chronic disease is a serious problem not only in the United States but worldwide.
We have much to learn about how to structure and furnish healthcare services for individuals with multiple chronic conditions. We also need to recognize that countries that perform better in coordinating care invest a higher proportion of their resources than we do in primary care. However, clinical guidelines focused on treating the whole patient, combined with improving the capacity of our primary care providers to better coordinate care, might help us to improve our performance. More importantly, this may result in better outcomes for a vulnerable group of patients. (Bindman, 2016)
Healthcare providers also need to understand that care for patients with chronic diseases is different from acute care. To ensure that these complex care needs are met, integration of new knowledge and treatment is required. If a nurse typically cares for patients with sudden-onset illnesses or patients with injuries for which the cure model is the focus, it may be difficult for the nurse to appreciate the differences in care for chronic diseases and needs of these patients.
As discussed in this text, many Americans have multiple serious chronic illnesses, and more and more are getting services in community settings (NAM, 2018a). These community-based services, however, are not consistent across the country and quality varies. Examples of these services are community-based palliative care, home- and community-based services, and hospice. We need better quality measures to evaluate accountability in community-based serious illness care. There has been greater emphasis on quality improvement, but this has been mostly focused on acute care. We need more quality improvement in public/community health. This effort needs to engage the patient, family, and caregivers along with the clinical care team, HCOs, payers, and communities. Policymakers at the local, state, and national levels also need to engage in these efforts to improve public/community health. The overall goal is to ensure that this population has timely and effective access to services based on their continuum of care needs (NAM, 2019a).
Because of the increased recognition of chronic disease, innovations in interventions and services for patients with chronic diseases have increased including factors related to healthcare reimbursement related to care services. Examples from the government payment perspective are important to consider, such as the CMS innovative models of care to promote care coordination: medical homes (a primary care model that provides core primary care functions and patient identifies as a major source of health care) and accountable care organizations, supporting transitional care, care coordination, and comprehensive care management services. Self-management and health literacy are also important elements to include in planning these services for patients with chronic illness to ensure a comprehensive public/community health program. Another method used is disease management, which is a systematic approach to managing a chronic disease, such as diabetes, cardiac disease, and so on. Typically, disease management interventions have been tested with large populations, and thus, they may be more effective than interventions tested in studies with smaller samples. Disease management emphasizes the use of interprofessional teams with expertise in the specific disease, use of evidence-based clinical guidelines, clear descriptions of interventions and procedures and application of recommended timelines, patient support and education, and measurement of outcomes. Nurses assume important roles in disease management; they may be on the team or lead the team. Insurers, hospitals, and other healthcare providers develop and sponsor disease management programs with the goal of assisting patients in maintaining the best quality of life possible and preventing complications that might lead to deterioration and increased costs of care.
Disease management programs also emphasize prevention, although, as discussed earlier, it is important to emphasize prevention throughout the healthcare system and particularly in community care-not just in special-focused programs. Examples of community prevention services include tobacco cessation counseling, screening (breast cancer, colorectal cancer, prostate cancer, diabetes, hypertension, hearing, vision, cholesterol, and so on), and immunizations. Prevention is not always successful and may be limited by lack of reimbursement, access to services, and providers who provide these services. In general, better patient outcomes are achieved using evidence-based techniques that emphasize patient activation or empowerment, collaborative goal setting, and problem-solving skills. Provider teams may use standardized assessments of patient self-management needs and activities to enhance their ability to support patients. Such assessments include questions about self-management knowledge, skills, confidence, support, and barriers (IHI, 2023c).
The report Living Well with Chronic Illness: A Call for Public Action described chronic illness in the United States as a major public health problem: “Chronic disease is a public health as well as a clinical problem. Therefore, a population health perspective for developing strategies, interventions, and policies to combat it is critical. A population perspective considers how individuals' genes, biology, and behaviors interact with the social, cultural, and physical environment around them to influence health outcomes for the entire population” (IOM, 2012, p. 3). Communities use a variety of options to enhance prevention particularly focused on chronic diseases and may be associated with less typical healthcare sites, such as health fairs, immunizations in locations that are easy to access (retail pharmacies, community centers, schools, work sites), offering walking groups in malls, enforcing smoking bans, offering educational opportunities about health, smoking cessation groups, and exercise, as well as screening for diseases, alcohol and drug misuse, stress, and so on. Establishing places for exercise in parks, such as walking/jogging paths and exercise equipment, identifying street bike lanes, ensuring healthy diets in school lunches, and so on-communities need to be creative in addressing their health needs and increasing access. Working closely with the community's acute care system is critical for the success of these community efforts-collaboration, coordination, and communication are elements that make for a healthier community.
Medical Home Model
The medical home model is a multidimensional solution for planned, clinically integrated care to meet the complex care needs of people with chronic disease by organizing care around patients, working in interprofessional primary teams, focusing on PCC, and coordinating and tracking care over time (NCQA, 2023). When the CMS and the Joint Commission identified APRNs as medical home providers, the profession supported this significant change (PCC, 2018). Other nurses also have roles in these newer models of ambulatory care that should not be ignored (Ortiz, 2018).
Self-Management
Self-management is a concept of care that focuses on the patient and the patient's role in managing personal care with resources provided and requires that the patient have access to health information. Electronic personal health records are now more common and support self-management. For example, this type of record can be used to help patients manage their health through individualized care plans, graphing and recording of symptoms, passive biofeedback, individualized instructive or motivational feedback, assisting in health care decisions, and providing a reminder system. Security, privacy, and confidentiality are all critical factors in effective use of electronic personal health records. It is important that when these systems are used, the system can adjust to meet the health literacy needs of the patient. Public/community health can utilize self-management to support members of the community, particularly patients with chronic diseases.
Health Literacy
Health literacy is a factor that has implications in all healthcare settings and for all patients (IOM, 2004). As mentioned elsewhere in this text, diversity is a key element of PCC, but it is important to recognize its relevance to public/community health as well. Patient education-whether from the perspective of individual patients, families, populations, or communities-is influenced by the patient's health literacy. The definition of health literacy was recently updated: “Personal health literacy is the degree to which individuals can find, understand, and use information and services to inform health-related decisions and actions for themselves and others. Organizational health literacy is the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.” These new definitions (HHS, CDC, 2023d):
- Emphasize people's ability to use health information rather than just understand the information
- Focus on the ability to make well-informed decisions
- Incorporate a public health perspective
- Acknowledge that organizations have a responsibility to address health literacy
Effective health literacy improves self-management and engages the patient (individuals, families, populations, communities) in the process (Brega, 2019). Three key supporting interventions to ensure health literacy, which continue to be important, are as follows (Sand-Jecklin et al., 2010):
- Identify patients at risk for lack of understanding and not acting on health information.
- Communicate health information and instructions in a way that promotes patient understanding.
- Check for patient understanding.
The report Health Literacy and Older Adults is a resource that examines health literacy issues for a specific population, older adults, and represents an example of the importance of health literacy that is also directed to specific populations. In addition to older adult health literacy needs, the content also includes information about health literacy needs of families, caregivers, and communities (NAM, 2018b).
| Stop and Consider 3 |
|---|
| Nurses who practice in public/community health need to view the patient as an individual who is part of a family, population, or community, and all may require nursing services. |
Multiple Perspectives of Public/Community Health Services
The following sections discuss examples of public/community health services that need to be considered and provided to ensure the health of communities and their populations. Many of these services are interrelated and are also needed for effective collaboration and coordination in acute care services.
Community Health Workers
Community health workers are not sufficiently recognized by many in communities including healthcare professionals. “There are tens of thousands of CHWs across the United States. Together, they form a safety net that protects the most vulnerable in our communities by helping remove barriers to health care-whether it be information, translation services, or trust building. Their work is as diverse as the communities they serve” (Levine, 2023). The HHS has designated a National Community Health Worker Awareness Week to emphasize the importance of the work done by CHWs-recognizing that they have a major impact on improving health equity in many communities. “A community health worker is a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served. This trusting relationship enables the worker to serve as a liaison/link/intermediary between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery. A community health worker also builds individual and community capacity by increasing health knowledge and self-sufficiency through a range of activities such as outreach, community education, informal counseling, social support, and advocacy” (APHA, 2023b). States are also recognizing the need to support and development services provided by CHWs; for example, California has increased integration of CHWs who provide frontline care to many populations through health education and connection to services and resources (Buller, 2024). Other states are also active in supporting these services. Nurses also need to collaborate with community health workers and include them as part of the team and as part of nursing practice.
Community Emergency Preparedness
Communities may be confronted with numerous challenges-natural disasters (for example, climate related), infectious diseases, excessive and/or sudden violence and substance use disorders, and potential attacks, such as bioterrorism or other types of terrorism-that could lead to major community health needs and safety concerns. The AHRQ has developed resources for public health emergency preparedness, and more on this topic can be found on the agency's website (HHS, AHRQ, 2023b). Community planning for such events is critical to better ensure community health and safety. We have seen what happens when communities are not prepared, such as the recent experience of COVID-19. In this case, communities learned “on the run” during the crisis, and as it extended over time, so did the stress and need for even more effective planning, resources (workforce, equipment, supplies, funding), and interventions. Healthcare providers should be engaged in planning and responding to emergencies. This includes all providers and some that may not be thought of as important. For example, pharmacists can be important community resources: From early 2021 to May 2023, community pharmacies provided more than 300 million doses of COVID-19 vaccines-representing more than 2 of every 5 doses administered in the United States (Layson-Wolf & Shartstein, 2023). This was a critical service provided by community pharmacies located where people live and work, increasing accessibility and community members are familiar with their local pharmacy. In some communities this resource made it easier to initiate administration of vaccine and even testing as these pharmacies are often active in providing immunizations routinely, such as for the flu.
Other examples in the last few years have been major climate-related disasters in the United States, as well as tragic violence and terrorism that have harmed many children and adults both physically and emotionally, for example, shootings in schools, faith-based organizations, and in other public places. Communities are now more alert to the need to plan for these situations. Nurses are involved both in the planning and providing care during public crises to help others, either in their regular positions or on specific disaster teams that respond to immediate and long-term disaster needs. For example, school nurses and representatives from faith-based organizations should participate in planning as part of emergency preparation as they have regular contact with community members. The Federal Emergency Management Agency (FEMA) has critical responsibilities related to disaster planning and response. Its mission is described in Exhibit 7-3. Nurses are involved in working with FEMA staff when there are disasters and guiding community members to receive needed support services.
| Exhibit 7-3 FEMA Five Mission Areas |
|---|
|
Exhibit 7-4 identifies some critical links that provide more information on this important topic.
| Exhibit 7-4 Sources for Information About Emergency Preparedness |
|---|
|
Some community situations that can lead to disasters require extensive healthcare services as well as prevention, for example, of environmental problems. An example of this type of problem occurred in Flint, Michigan, when the community found lead in the water system. This is a complex problem for the community, particularly the children who were affected, and in some cases will have a lifetime impact. It required multiple responses, including the provision of immediate water needs, short- and long-term assessment of potential victims, improvement of the water system, health education, short- and long-term treatment for victims, collaboration with education experts to help children who might have disabilities, family support and guidance, mental health services for those suffering from the stress of the experience, and much more. All of this is costly and requires expert healthcare services and guidance. In this type of situation, nurses should be involved at all levels-assessment, prevention, treatment, and follow-up-and in multiple settings, such as public/community health services, clinics, schools, and other services.
Managing Population Health
There is greater emphasis today on learning how to effectively manage population health to reduce costs and improve outcomes (Finkelman, 2023b). The first step is to identify the target population. The second step is to assess the health status and needs of the population and then apply prevention and interventions to improve the population's health. This approach can have an impact on overall health care in the community.
With the increase in number of persons with chronic diseases, focusing on a population with a specific chronic disease, such as arthritis or diabetes, can be useful. Coordinating services across a continuum of care and tracking data about outcomes are important aspects of managing population health within a community. The ACA includes provisions that emphasize community and population health. For example, the law calls for increased funding for community health centers, development of medical homes and community-based transition grant programs, incentives to reduce readmission rates, outcome measures for chronic diseases and wellness and prevention programs, development of employer wellness programs, and requirement for nonprofit hospitals to conduct comprehensive needs assessments every three years and report to the Internal Revenue Service the activities they pursue to address the identified needs. These provisions have been enacted, though if there are changes in ACA funding or in the law, some of the provisions may be changed or eliminated.
To support communities in improving population health, the National Quality Forum (NQF) published a guide emphasizing 10 elements (NQF, 2016):
- Collaborative self-assessment
- Leadership across the region and within organizations
- Audience-specific strategic communication
- A community health needs assessment and asset mapping process
- An organizational planning and priority-setting process
- An agreed-upon, prioritized set of health improvement activities
- Selection and use of measures and performance targets
- Joint reporting on progress toward achieving intended results
- Indications of scalability
- A plan for sustainability
Communities need to use this type of information in their planning and initiatives to improve overall health and services.
With increasing recognition of the need for public/community health, nurses should provide leadership in this area of the healthcare delivery system, particularly in population health. Examples of comments about this opportunity for nurses are (Wilson et al., 2023):
- An urgent need exists for nurses to engage in and lead population health activities and services.
- Many familiar with the nurse's role in acute care view the nurses engaged in population health activities as novel, but nursing has a long history of involvement in this aspect of health care.
- Nurses with the competency to engage in and lead population health programs can help design and implement activities to improve a community's overall health.
A national report on global quality healthcare noted the following about universal health coverage (NAM, 2018c). Although evidence is scattered and incomplete, the conclusion is noted in the WHO Sustainable Development Goal 3 (SDGs) focusing on universal health coverage and “measures the ability of countries to ensure that everyone receives the health care they need, when and where they need it, without facing financial hardship. It covers the full continuum of key services from health promotion to prevention, protection, treatment, rehabilitation, and palliative care. Progress on UHC is tracked using two indicators: coverage of essential health services (SDG 3.8.1); and catastrophic health spending (and related indicators) (SDG 3.8.2)” (WHO, 2023f). As discussed later in this text, the report also emphasized the need to support the six dimensions of quality: safety, effectiveness, patient/person-centeredness, timeliness, efficiency, and equity, which is referred to as STEEEP®. The transformation of health care must be guided by leaders-government, healthcare professions, and other organizations using systems thinking and measurement.
Ambulatory Care
Ambulatory care is found in all communities, offering a variety of services, such as primary care, outpatient procedures and surgery, health promotion and prevention, and other services. This care should be easily accessible to the community. Nurses work in these services, as mentioned earlier in this chapter. The AHRQ emphasizes that staff in ambulatory care need to ensure quality care and effectively support care transition as patients move in and out of ambulatory care and other settings. The AHRQ offers resources and tools for healthcare professionals to effectively care in varied settings and services to (HHS, AHRQ, 2017):
- Reduce errors related to transitions of care.
- Increase patients' engagement in their own plan of care.
- Improve communications among patients, care partners, and other facilities.
- Address requirements related to coordination of care.
- Enhance overall patient and clinician experience.
Migrant and Immigrant Issues
In 2011, the ANA recognized the importance of immigrant health care and the need for the ANA to get involved in this issue. This led to the development of an ANA policy brief on the topic entitled, Nursing Beyond Borders: Access to Health Care for Documented and Undocumented Immigrants Living in the United States (Trossman, 2011). Access to healthcare services for this population continues to be a problem (KFF, 2022). Even though this is a complex political issue, it is still important for nurses to understand the needs of this population and provide care when it is needed. This is a diverse population-representing multiple cultures and languages, and this impacts health and healthcare services. This population may or may not increase healthcare expenditures. Since they visit the emergency department less often than U.S. citizens these expenditures are often lower than care for most adult citizens. Some of this is due to this population's concerns about interacting with potential government officials, particularly if there are problems with legal status. However, they often work in hazardous jobs, such as agriculture and construction, increasing their risk for injuries and illness, which can be costly if they need care.
The process of immigration and the integration of immigrants into American society intersect with many of the social and economic factors that impact health, including economic stability (and factors related to food, housing, and so on), access to health care services, education, the impact of the built environment (buildings, infrastructure, parks, public spaces, and so on), and social and community context (SDOH). On average, immigrants are healthier than native-born Americans. Yet, immigrants are subject to the systematic marginalization and discrimination that often lead to the creation of health disparities. These complex interactions between immigration and health have not been well explored, but they are a significant determinant of differences in health and well-being between population groups in the United States. (NAM, 2018d, p. 1)
Potential changes that may be made at the federal level in immigration legislation may increase the importance and complexity of these issues and hopefully may provide more support for this vulnerable population. States that are also coping with immigration issues, they too are involved in this type of legislation at the state level and also concerned about federal legislation. Nurses need to be aware of the current issues and provide consultation to ensure that health needs are met, ensuring effective health equity within their communities.
Home Health Care
The amount of health care provided in the home has increased in the United States. As part of efforts to control costs, patients are discharged earlier from the hospital. Often at the time of discharge, many patients are not fully recovered or ready to care for themselves. Home health care provides healthcare services in the home. These services vary as to the type, the amount of time that the care provider is in the home, the number of visits per week, and the length of services (for example, may be provided for a week, three months, and so on). In addition, there is variation in the type of healthcare provider needed: home health aides who provide assistance with activities of daily living services (bathing, ambulation, simple care, light housekeeping, food preparation); registered nurses who assess the patient, develop the care plan, monitor progress, assess the home environment for safety, and provide more complex care collaborating with the physician(s); physical therapists who help the patient with exercises to gain strength and mobility; or social workers who assist with obtaining other services that patients may need, such as Meals on Wheels, payment for healthcare services, and so on. Digital health is now used in some home healthcare situations, using technology to communicate with the patient, assess status, and so on. There is greater use of technology to share and document home health information. (Additional information on digital care is provided in later content.) Given the growing number of persons with chronic diseases and the aging population, home health care is expected to increase as a community health service.
School Health
School health has changed and expanded in many communities over the years. A critical concern that is not uncommon is limited school health services due to budget cuts for schools and public/community health services. Typical methods used to reduce costs for school health are decreasing the number of RNs in schools or having school nurses cover several schools. A review of school nurse staffing indicated 65.7% of schools have access to a fulltime (>35 hours a week) school nurse (RN, LPN, LVN), and this represents 70.3% urban schools with fulltime nurses and 56.2% rural schools (NASN, 2021). The National Association of School Nurses describe the school nurse role as supporting individual and population-based student health, providing care coordination, advocating for quality student-centered care, and advancing academic success-providing a healthy and safe place to learn.
In some communities, school health services have expanded into full clinics in the schools, often covered by pediatric APRNs. This can be particularly important in urban communities that may have limited access to services for children with inadequate health insurance coverage and limited family financial resources or in rural areas that may have insufficient pediatric services. School nurses can make a major difference in children's health and, consequently, their long-term health as adolescents and adults, through active use of prevention and appropriate timely treatment. As experienced with COVID-19, school health is a critical part of the community health system during a time of public health crisis, requiring the establishment of guidelines for students, faculty, and staff, maintaining a safe environment, and monitoring students, faculty, and staff for infection. Demonstrating the need to improve school health services, “[t]he HHS, through the Health Resources and Services Administration (HRSA), in the spring of 2023 announced the availability of approximately $25 million to expand primary health care, including mental health services, in schools. For the first time, applicants will be required to add or expand mental health services to receive school-based funding. HRSA-funded health centers currently operate more than 3,400 school-based service sites in schools across the country” (HHS, HRSA, 2023b). This type of initiative is very important in improving and expanding services to children, a vulnerable population in any community.
Rehabilitation
Rehabilitation is part of tertiary prevention. The goal of rehabilitation interventions is to attain and retain the best level of functioning for a person who has an illness or disability that may be temporary or permanent. Rehabilitation can take place in the hospital, an extended care or long-term care facility, an ambulatory care facility, or the patient's home. Rehabilitation therapists assist the patient by providing specialized therapies, such as a physical therapist, occupational therapist, speech-language pathologist, or vocational services. The nurse may be the healthcare provider who identifies the need for rehabilitation, or the nurse may be involved in assisting with the implementation of the rehabilitation plan. Patients may need to learn how to complete activities of daily living, such as taking care of personal hygiene and dressing; ambulating safely with or without assistive devices, such as a walker, cane, or wheelchair; learning basic life skills, such as cooking or driving with a disability; and learning new job skills. Some patients recover more fully than others, making assessment, treatment planning, and ongoing evaluation important care activities. Examples of patients who may require rehabilitation are those who have suffered a stroke, severe burns, or major injuries from an automobile accident or a work-related accident, such as a serious fall or experiencing a major injury due to work equipment.
Extended Care, Long-Term Care, and Elder Care
With increased aging in the U.S. population, the need for services to meet this population's needs is growing. Gerontological nursing is an important specialty that focuses on the care of the older adult population in all settings; however, the most important extended care settings involve care in the home, particularly with greater interest in “aging in place” or staying in your own home as you get older. Other services are offered in skilled nursing or intermediate-care and long-term care, in which patients receive a range of services from housing, meals, and activities to routine personal care, rehabilitation, and specialized treatment. There is a greater need within communities for more eldercare services, such as adult day care (a facility where older adults may go during the day for socializing and activities), home health care, senior centers, and retirement and assisted-living facilities (these can vary from single rooms to independent living situations with support services as needed).
Older adults experience health problems in all body systems and psychologically. They may also experience social problems, such as loss of spouse and friends, decreased mobility, and isolation. Financial problems are not uncommon, and these problems affect nutrition, housing, social activities, transportation, and access to medical care. Community health services for this population must consider multiple factors that impact quality of life. During the COVID-19 pandemic, many older adults self-isolated or were forced to isolate/quarantine, and this led to both physical and psychological problems-cut off from family and friends and services they needed. At the conclusion of the pandemic, long-term problems need to be addressed. Communities need to use this experience to consider how they might respond to future public health emergencies; some may be the same type of emergency, and others may have similar characteristics, but planning for more effective responses and support for this population is important. For example, in the summer 2023, many states experienced excessive heat. This weather led to people staying at home, particularly those at greater risk, such as older adults. They again experienced isolation and needed to get health services and supplies (water, food, medications, and so on), in addition to needing checks to ensure that they were not in unhealthy heat situations at home.
Another important problem experienced by older adults is elder abuse. The CDC's Office of Disease Prevention and Health Promotion, as part of HHS, has hosted three national symposiums on healthy aging and the SDOH and collaborated with the Elder Justice Initiative to bring awareness to important issues facing older adults (Mao, 2022). Elder abuse is a type of interpersonal violence that is an SDOH. It is “defined as an intentional act or failure to act by a caregiver or another person in a relationship involving an expectation of trust that causes or creates a risk of harm to an older adult (typically defined as age 60 years and older). Elder abuse comprises 5 subtypes: physical abuse, sexual abuse, psychological abuse, caregiver neglect, and financial exploitation and fraud” (HHS, CDC, 2016). This problem needs to be addressed to improve health outcomes and provide more effective opportunities for aging in place. Healthcare providers who interact with older adults need to be alert to indicators of elder abuse-listening and talking with older adults; assessing needs, including social and psychological; and finding assistance to meet a variety of needs, including meeting needs associated with SDOH.
End-of-Life Care and Palliative Care
Hospice care is a philosophy of care for the terminally ill that involves supporting the quality of one's life as long as possible (end-of-life care). Hospice care does not need to be provided in one type of physical place, though it can be-for example, a freestanding building for hospice services, typically focused on care for up to six months. This care can also be provided in the patient's home or in a special unit in an acute care hospital or a long-term care facility. Hospice care includes active patient and family participation in all care decisions. Specially trained staff-including physicians, nurses, social workers, spiritual professionals, as well as other healthcare providers as needed-support the patient and family during the critical last stages of life. Palliative care focuses on alleviating symptoms, meeting the special needs of patients with serious, complex problems, and supporting the family. Both palliative care and hospice care emphasize interprofessional team care. There is strong support for more nursing leadership and the provision of palliative care by nurses. The Future of Nursing report (IOM, 2011a) identified nurses as the ideal providers of palliative care. The National Institute for Nursing Research (NINR) provides resources about palliative care and notes that “offering interventions and translating our science related to hospice and palliative care can enhance the quality of life for those most in need of symptom management and emotional support” (HHS, NIH, NINR, 2023). The NIH collaborates with the NINR to expand research and develop resources for these critical needs, supporting a partnership among the various research institutes and other federal government agencies (HHS, NIH, NINR, 2021).
Recognizing the growing need to ensure that nurses are prepared to care for patients with palliative care and end-of-life needs, the AACN developed Palliative Competencies and Recommendations for Educating Undergraduate Nursing Students (CARES) to support nursing education in preparing nurses to ensure this care is culturally sensitive and uses an interprofessional team approach focused on assessment and management of complicated illnesses (AACN, 2023c, 2021; Zolot, 2016). The competencies for this care focus on the following: the need to identify palliative care as an important part of assessment and planning; recognition of multiple factors that impact care, such as demographics, economics, health delivery issues, complexity of caregiving and impact on families, and so on; impact of nurse's ethnic, cultural, and spiritual values and beliefs related to illness and death, and the need to be aware of the same in patients and families; use of effective communication and compassion with patients, families, team members, and the community supporting palliative care; use of effective team collaboration and coordination; recognition of respect and ethical principles; application of local and national legal guidelines relevant to serious illness including privacy and confidentiality; implementation of comprehensive assessment to plan care; ensuring effective pain management; incorporating psychological, social, and spiritual needs in care to improve quality of life; evaluating outcomes; supporting self-care and resilience when appropriate by assisting with grief and bereavement, when possible; and consulting with others when needed (AACN, 2023c).
Case Management
Case management is a system of care delivery that aims to get the right services to the patient at the right time and avoid fragmented and unnecessary care that can be costly (Finkelman, 2011). It facilitates effective care delivery and outcomes for patients. Case management requires collaboration or cooperative effort among healthcare providers and other sources of resources that the patient may require. Coordination is required to organize care so that it is available when needed. Communication is also critical because the case manager must work with many people to ensure patients get the required care. Case managers may do all their work on the telephone and may never actually see the patient or family. They are typically employees of an insurance company, a government agency, or a healthcare organization (particularly acute care settings [hospitals]), but they may also work for agencies within the public/community health system. Because cost-effective care delivery is a concern, case managers need to have extensive knowledge about reimbursement and understand how to manage care services in a manner that controls costs. Case managers-who may be nurses, social workers, and other staff who work with patients and their families-direct the patient to care when needed and monitor progress. Typically, care protocols or pathways guide the case manager in making decisions about the best care for specific health needs, which are adapted to meet individual patient needs. Hospitals may also use case managers to assist with complex patient needs and plan the best care posthospitalization. Case management is an area of care delivery that is effective in better ensuring patients receive the care they need in an often complex and confusing healthcare system.
Occupational Health Care
Occupational health care may be viewed as a strange nursing topic, but nurses are very active in this setting, providing health promotion, disease and illness prevention, and treatment services, including assessment of risks of illness and injury associated with the work environment, for example, during the COVID-19 pandemic the need to follow regulations to protect workers from the infection and monitor exposure to the virus (AAOHN, 2023). “COVID-19 is an occupational disease that sickened and killed countless workers in health care and long-term care, and in meat processing, agriculture, warehousing, transportation, corrections, and other ‘essential' industries. Nonetheless, COVID-19 has rarely been treated or tracked as an occupational disease by public health agencies, particularly in non-healthcare workplaces. The lessons from the failure to protect workers during the COVID-19 pandemic can be helpful as the nation anticipates and prepares for the next public health emergency” (Michaels et al., 2023, p. 24).
Occupational health is considered part of public/community health. Providing these services at the work site makes it easier for employees to obtain services with less concern about getting to appointments during work hours. Many employers have found it is beneficial to provide these services on site for employees, often reducing their potential health risks and providing prompt treatment. All of this can reduce employer health insurance costs and increase work productivity; however, employee privacy continues to be an issue and must be maintained even if services are provided at the work site.
Employers may provide a variety of health promotion and prevention services, such as exercise classes or even gym access; stress management resources and onsite classes, such as yoga, nutrition, and weight-management classes and services; smoking cessation information and programs; immunizations; and other types of opportunities for employees to maintain a healthy lifestyle. Employers may also consider factors, such as food and related nutritional factors served in the cafeteria; environmental health issues within the worksite such as air quality and noise levels; walking areas for employees during breaks; equipment to prevent back injuries while moving patients or moving equipment or products; use of ergonomic chairs and desks and other equipment, such as protective devices related to lifting; and so on.
Complementary and Alternative Therapies or Integrative Medicine
The National Center for Complementary and Alternative Medicine (NCCAM), which is part of the NIH, describes complementary and alternative medicine (CAM) as a group of diverse medical and healthcare systems, practices, and products that are not presently considered part of conventional medicine (HHS, NIH, NCCAM, 2023). Conventional medicine is medicine typically practiced by holders of medical doctor or doctor of osteopathy degrees and by other health professionals, such as RNs, physical therapists, and psychologists. Some healthcare providers practice both CAM and conventional medicine. Although there is some scientific evidence supporting the use of CAM therapies, for most, there are still key questions that have yet to be answered through well-designed scientific studies-questions such as whether these therapies are safe and their outcomes. The list of the types of interventions that are part of CAM changes continually as therapies that are proven to be safe and effective are adopted by conventional health care and new approaches to health care emerge. Countries in Europe, Asia, and the Middle East, actively use CAM, and these interventions are covered by their universal healthcare plans. These interventions may be offered in communities, for example, senior citizen groups to participate in tai chi in community parks or acupuncture offered in clinics.
Many of these interventions are not new, but their use in modern healthcare delivery has increased in recent years. However, many of the CAM interventions still need to be assessed before they become part of conventional medicine. Examples of CAM interventions are acupuncture, acupressure, massage, light energy, Reiki, tai chi, and the use of a variety of herbs and other supplements, such as garlic, shark cartilage, and ginseng. With the creation of NCCAM, there is now an organized system for clinical trials to collect and analyze data about the use of CAM and related outcomes. Nurses may provide some CAM interventions in their practice, and some insurers cover these services, but this is not yet typical in the United States. As more data are obtained to support their efficacy, there will probably be more inclusion of these interventions in care, and they will gain greater reimbursement coverage.
Genetics
Genetics has become more of a focus in health care, and it will have a long-term effect on public/community services. The U.S. Department of Energy and the NIH have funded and led the National Human Genome Project, which began in 1990 and was completed in 2003. This project focused on mapping all the loci of the 20,000-25,000 genes that make up the human body and has many implications for health. We have learned that the interaction of the genetic makeup of an individual and the environment (genomics) often determines whether the person will be healthy or ill for the majority of his or her life. “The project also supports exploration of the complex ethical, legal, and social implications of genomics, and is committed to ensuring that the knowledge and benefits generated from genomics research are disseminated widely, both to fuel current and future researchers and to benefit the public and promote genomic literacy. The benefits of this research help us deal with health problems including the following.” (HHS, NIH, NHGRI, 2023)
- Improved diagnosis of disease
- Earlier detection of genetic predispositions to disease
- Rational drug design
- Gene therapy and control systems for drugs
- Pharmacogenomics/custom drugs
When this information is used in combination with a family history tool to gather information about diseases in the family, a very thorough risk assessment can be completed (HHS, CDC, 2023e). If this risk assessment is used as part of health promotion, the health professional can explain to patients and families not only their risk for getting a disease because of their genetic profile but also the interactions between the environment and the person's genomic risk. With the knowledge of how a person's genes interact with drugs, pain medications may be designed to address individual health status and needs. This knowledge makes it possible to consider precision or personalized medicine as an option for some patients now and in the future-to offer the right treatment, to the right patients, at the right time, targeted to their genetic makeup (HHS, FDA, 2018). We also now have the ability in some cases to fix a bad gene because we know its location and its actions. The technology to diagnose diseases and conditions even prenatally is expanding, giving us the tools to allow a fetus to continue to grow normally instead of having major anomalies at birth. The possibilities are endless for disease prevention and management. We are at the beginning of a new frontier of health care and related nursing care, individual and population health.
| Stop and Consider 4 |
|---|
| Public/community health services are expanding, and this affects the roles of nurses. |
The Changing Nature of Public/Community Health Problems
Public/community health changes more than acute care, even with all the advancements in medical treatment. It is affected by many factors that are broader-socioeconomic, cultural, travel, global issues, climate, communicable diseases, community safety, law enforcement and other similar services, education, religion, immigration, and much more. The following sections provide a few examples of problems that are primarily focused on the community and for which much of the response must come from the community. This, however, does not mean that acute care is not relevant. The ideal is to have a system of care that incorporates both acute care and public/community care supporting effective coordination, communication, and collaboration.
Violence in Communities
An example of the changing nature of public/community health is increasing violence in some communities, and it is now viewed as a public health crisis. This type of violence is not new, but we have times of greater and lesser violence, and some communities experience major crises with violence involving families, adults, and children. Some of the violence may be associated with crime and drugs or crowds protesting and getting out of control. NAM published a report on a professional discussion it held to examine violence focused on a comprehensive analysis of community violence as a population health concern-background, causes, and community interventions (NAM, 2017). Violence is a social determinant of health and important to consider in public/community health systems and is viewed as a chronic, recurrent disease. Some refer to violence as a contagious disease. This report describes serious problems that result from community violence, even describing a community with violence as a “war zone.”
Violence is an action but also a reaction to situations in which people, often young people, feel they are trapped, and so they respond with violence and risky behaviors, such as using drugs. Many of the same factors and the environment in which people live have an impact on domestic violence. This is a topic that nurses need to understand not only in communities with high levels of violence but also community planning should include assessment of violence risk, prevention and safety interventions, and responses to violent events. Because violence is a highly complex issue, it requires understanding multiple variables and the use of a broad range of interventions to ensure safety for individuals, families, and neighborhoods, such as eliminate empty houses and buildings where gangs can hang out, collaborate with health services and law enforcement in planning and implementing interventions, ensure better gun control enforcement, provide programs for substance use disorders (drugs and alcohol), provide support for students in schools, implement community safety education, and so on; monitor areas where children might be at risk, such as playgrounds or walking home from school; ensure older adults get their needs met when they are afraid to leave their homes; ensure safety in public places, such as lighting; and so on. When violence increases, community members experience high levels of stress, anxiety, depression, and anger. All of this affects short- and long-term mental health, and services are needed for these problems, both for prevention and treatment.
With the increase in violence, the increase in the availability of guns/firearms has become a growing, critical concern in many communities and also a political issue. “Firearm-related injuries and deaths in the United States are a public health crisis. High-profile mass shootings, localized episodes of violence, suicides, and gun-related accidents all too frequently stimulate our personal and collective grief and outrage. But-contrary to response and recovery patterns after other crises-effective follow-up adaptations to mitigate further harm are often thwarted by cultural, legal, and political barriers. As with other public health challenges, that means openly acknowledging the scope of the problem, updating the public on what is done to reduce firearm-related injuries and deaths, and providing the most up-to-date available guidance to help the broader public navigate the crisis” (Reed, 2022). The data demonstrate this is a serious public health challenge with 45,222 firearm-related deaths in 2020; 124 people dying each day from this cause, and the United States has higher rates than many other countries, such the EU countries and Australia. There are higher rates of firearm deaths in men, young adults ages 15 to 34 years, and Black or African American, American Indian or Alaska Native, and Hispanic or Latino populations (Reed, 2022). Local, state, and federal discussions about this public health crisis continue. Nurses should engage in this policy discussion as it impacts their practice and health care.
Violence also affects a variety of stakeholders, including acute health care, particularly emergency services and critical care, and it also impacts community services, such as the police, emergency responders, and the fire department. Many community organizations and groups, such as schools, transportation, businesses, housing, and community centers and other gathering places such as playgrounds are also concerned about violence. This requires that communities assess and prevent this problem and are prepared to respond if violence occurs. Violence occurs in many settings and may lead to the need for healthcare services, but it also happens in HCOs and social service locations, increasing risk and stress for healthcare providers. Even home healthcare is not immune to a risk of violence-for example, how safe do nurses feel going into a neighborhood or a home? What should they do to protect themselves? Safety must be assessed routinely, and healthcare staff need to be prepared to respond in a manner that maintains their safety and the safety of those around them.
Opioid Epidemic
The opioid epidemic is not an uncommon story in the news. Stories such as this one: In 32 hours, a city experienced two calls for assistance per hour for overdose patients. Demonstrating an increase, the number of overdose calls in 2015 was 4,642, and in 2016, it was 6,879 (Hauser, 2017). Many communities across the United States are dealing with this epidemic that is hitting all sectors of society. Narcan is recommended for response to an overdose and can save lives. Emergency services now carry this drug, but getting enough Narcan is sometimes a problem, as is its cost. In 1991, the pharmaceutical industry told healthcare providers that opioid drugs were not addictive, and this led to expanding prescriptions for this drug. The tragic result is they are addictive. The HHS declared the opioid epidemic as a public health crisis. The CDC as part of the HHS monitors and provides current data on this public health problem. See Figure 7-5 describing the growing problem of opioid overdoses related to opioid use disorder (OUD) (HHS, CDC, 2023f). The American Medical Association (AMA) also recognizes that this is a critical public health problem (2023). Nurses encounter patients and families dealing with this problem in all types of healthcare settings and in schools and workplaces.
Figure 7-5 Rise in Overdose Rates in America.
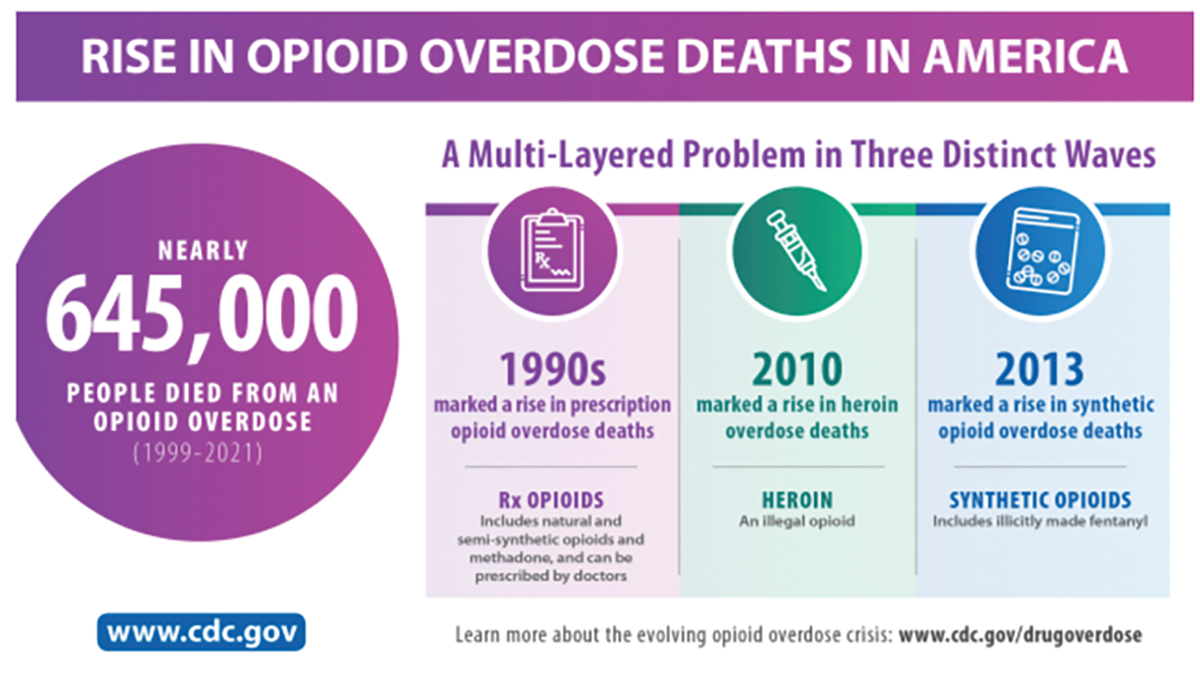
An infographic depicts the rise in opioid overdose deaths in America.
The infographic provides a detailed overview of the rise in opioid overdose deaths in America from 1999 to 2021, totaling nearly 645,000 fatalities. It breaks down the crisis into three distinct waves: the 1990s with a rise in prescription opioid overdose deaths including drugs like natural and semi-synthetic opioids and methadone, the 2010 onset of heroin, an illegal opioid, and the 2013 increase in deaths due to synthetic opioids, specifically mentioning illicitly made fentanyl. The source and additional resources can be found at the C D C's website w w w dot c d c dot gov. Text at the bottom reads, Learn more about the evolving opioid overdose crisis: w w w dot c d c dot g o v forward slash drug overdose.
Centers for Disease Control and Prevention (CDC). (2023). Opioid data analysis and resources. https://www.cdc.gov/opioids/data/analysis-resources.html
As concern has increased about opioid use, several major reports addressed pain management and opioid use. Relieving Pain in America noted that an estimated 100,000 people experienced chronic pain, resulting in an annual healthcare cost of $630 billion (IOM, 2011b). Since this report was published, opioid use increased, but this report served as an alert to a growing problem and provided evidence that the United States needed to respond quickly. The message is not that treatment should not be provided for pain, but rather, we need to do this carefully, with an understanding of benefits and consequences, and use effective interventions for pain with the least risk of harm.
Overlooked amid the intense focus on efforts to end the opioid use disorder epidemic is the perspective of clinicians who are experiencing a significant amount of daily tension as opioid regulations and restrictions have limited their ability to treat the pain of their patients facing serious illness. Increased public and clinician scrutiny of opioid use has resulted in patients with serious illness facing stigma and other challenges when filling prescriptions for their pain medications or obtaining the prescription in the first place. Thus, clinicians, patients, and their families are caught between the responses to the opioid use disorder epidemic and the need to manage pain related to serious illness. (NAM, 2019b, p. 1)
The impact of addiction on families is also a major concern-for example, the following may occur in these families: Older family members may need to care for grandchildren to help adult children who misuse opioids, divorce, and domestic abuse. Another problem is disparities in who receives access to pain assessment and treatment, such as prescribed pain medications. There are also problems with physicians and other healthcare professionals lacking sufficient understanding of pain-often underestimating pain. Patients and healthcare providers may have different perceptions of pain. There is a stigma associated with opioid use and substance use disorders, and it is very difficult to address. This stigma has existed for a long time and has an impact on the treatment and attitudes of those who provide treatment.
This public health epidemic has led to multiple approaches directed at prevention, treatment, and rehabilitation. Prevention focuses on communication with members of the community about the dangers of drug misuse and treatment options. Opioid use not only affects the person addicted to the drug and their families, as noted above, but also close associates, employers who must deal with employees who are not productive or may be unsafe in meeting job demands, and there may be increased criminal activity in a community. There is also a heavy burden on the healthcare delivery system with more services required. Education must be provided to children and adults about the dangers of using this drug as well as other risky substances. Healthcare providers must be educated about the risks of prescribing this type of medication and the importance of monitoring patient use when it is prescribed. The CDC and the Office of the Surgeon General developed information and materials to assist in communicating this message and provide approaches to avoid abuse-this initiative is called “Turn the Tide,” which is now led by the organization Turn the Tide (TTTrx, 2020). This information is directed at prescribers; however, nurses should also review this material. The key message is: Do not prescribe opioids as first-line treatment for chronic pain-excluding active cancer, palliative, or end-of-life care. The Surgeon General's information was sent in a letter with a pocket card for easy use to 2.3 million doctors, nurses, dentists, and other clinicians, asking for their help (Murthy, 2016). This is an example of a broad community education effort recognizing the importance of the public health problem. In addition, editorials and articles were published in the fall of 2016 in multiple medical journals, supporting the need for greater attention to this problem, and it continues to be a problem. Popular media, such as films, television series, and even documentaries, have focused on this problem.
Many communities with opioid use problems are working on providing more treatment and rehabilitation options. What is complex about this problem is once someone is addicted the person has a chronic health problem that can also lead to other health problems. Treatment is costly, and if a person does not have insurance, the situation is even more complex. This may also lead to many other problems, such as unemployment, financial problems and loss of one's home due to insufficient income, difficulty with school, problems during pregnancies and for newborns, mental health issues, domestic and child abuse, divorce, crime, overdoses (accidental or suicide), and much more. These are all major concerns for a community, particularly if they involve many members of the community. The COVID pandemic has not helped this problem because attention turned to the virus, and yet the opioid epidemic continued (Baumgartner, Aboulavia, & Collins, 2020). In addition, the virus and its impact, such as illness, isolation, death, loss of jobs, loss of housing, stress, and so on, are factors that make it more difficult for people to cope when they also have a substance use disorder and may be limited if family members can respond effectively.
Nurses need to be involved in community planning to respond to the SUD problem, including the opioid epidemic, along with an interprofessional team that should include other community leaders, such as government officials, law enforcement, religious leaders, education leaders, business owners, and so on. It will take a multipronged approach to improve the health of the community and its residents who are experiencing OUD. An example of recognition of SUD as a major public health problem is the American Association of Colleges of Nursing offering a special course online for nursing faculty: Implementing a Substance Use Course in RN-BSN Curriculum with the goal of integrating this content for nurses in practice who are pursuing a baccalaureate degree. The AACN notes: “Substance use in the United States increased dramatically during the COVID-19 pandemic and is already alarmingly high, 13% of Americans reported beginning or increasing use of substances during this time to cope with pandemic associated stressors. Additionally, opioid deaths increased by 30% during this same period. Nurses care for patients experiencing substance use disorder (SUD) in every healthcare setting and historically nursing curriculum has not well-prepared students for caring for this vulnerable population. With the increase in substance use, nurses must be equipped with the knowledge to provide care for this vulnerable population” (AACN, 2023d)
Epidemics and Pandemics
The United States has experienced epidemics, which are the spread of an infectious disease, and pandemics, which are infections that have a global impact. The experience of the COVID-19 pandemic has been a global crisis of epic proportions. We have seen the COVID-19 pandemic hit the healthcare delivery system from multiple perspectives. For example, routine public/community health services: “In some communities, non-essential public health services unrelated to the prevention and mitigation of COVID-19 are currently suspended, including monitoring of tobacco and electronic nicotine sales and regular inspections of food establishments. Moreover, the skeleton crew our country assigns to primary and secondary preventive services is being diverted” (Edmonds et al., 2020, p. 323). Other changes that occurred in communities as they tried to manage their response to the growing problem of the virus, for example, hospitals limited or canceled elective procedures and appointments, greater use of digital health methods, coping with medical equipment, supplies, and drug shortages, need to access and manage new testing procedures (for the virus), transferring patients in a manner that ensured safety and reduced exposure to the virus-sometimes far from their homes, patients waiting long hours in ambulances, caring for patients who are not able to be with family members, staffing difficulties and providing support to staff leading to high levels of stress and burnout, staff illness and death, staff burden in dealing with high mortality rate both emotionally and management of the experience, developing new treatment procedures to deal with complex medical problems, and the impact on emergency department and intensive care experiences due to patient overload. For example, there was a shortage of personal protective equipment (PPE) even for ambulance staff and other responders, staff involved in testing, and others, impacting exposure, safety, and services. Communities had to adjust to meet public health requirements, such as testing, tracking illness, communication with the public so that the public was prepared and encouraged to follow all requirements needed to protect the public, economic issues to meet new health needs and the impact of job losses or reduced house and limiting income for basic current needs and even long-term needs, impact on the school system and school health nursing, and reimbursement for healthcare services-impact on people without coverage and on HCOs when they did not receive payment for services and yet still had expenses to cover. Vaccination for the virus has been a major challenge-getting the vaccine to each state and distributing, storing, and administering it and working with the public to accept vaccination. Dealing with public health interventions, such as wearing masks, social distancing, decreasing group activities, and use of quarantine and lockdowns all have had an impact on individuals, families, and communities as well as staff. Addressing COVID-19 was a public health crisis that required a community-based response, but in many situations, this was difficult to communicate and achieve public compliance.
There has been a lot of focus on acute care issues and the pandemic, but there are other areas in the healthcare delivery system that were impacted, for example, home health care (HHS, CMS, 2023c). Changes had to be made to ensure that patients received these services for health needs that may or may not be related to COVID-19. The CMS identified goals for these temporary changes in home healthcare requirements to:
(1) expand the healthcare system workforce by removing barriers for physicians, nurses, and other clinicians to be readily hired from the community or from other states; (2) ensure that local hospitals and health systems have the capacity to handle a potential surge of COVID-19 patients through temporary expansion sites (also known as CMS Hospital Without Walls); (3) increase access to telehealth in Medicare to ensure patients have access to physicians and other clinicians while keeping patients safe at home; (4) expand in-place testing to allow for more testing at home or in community-based settings; and (5) put patients over paperwork to give temporary relief from many paperwork, reporting, and audit requirements so providers, healthcare facilities, Medicare Advantage and Part D plans, and states can focus on providing needed care to Medicare and Medicaid beneficiaries affected by COVID-19. (HHS, CMS, 2023c)
This is an example of how during a public health crisis policies need to be adapted quickly to ensure that care is received in all types of services. Public/community health services also experienced budget and staff shortages to meet the demands of routine public health services. Communities tried to attract new nurses and retired nurses to provide services, or, in some cases, states asked for help from other states that were not experiencing high levels of the virus and a staffing shortage. These issues demonstrate the complexity of trying to respond to a public health emergency-one that impacts the entire healthcare system.
And we have not yet experienced or fully understand the long-term impact COVID-19 might have on the health of those who have been exposed to the virus and/or experienced illness from the virus and the emotional impact on many people due to stress-for example, will there be a need for care coordination, rehabilitation, and so on? This will have an impact on the type and level of future healthcare services and staffing. Quality care issues are not something that should be forgotten during this stressful time. Errors continue to be made in healthcare prevention and treatment processes. There was a greater need for staff safety, training on the spot, adjustment to changes that impacted effective communication due to confusion, and lack of time to meet all the usual quality improvement needs and additional ones required for the virus. “Upcoming public health changes will include conducting contact tracing, primary prevention and its impact on frontline providers will continue to evolve and will necessitate continued agility by the healthcare system. What may transpire as a result of the last several months will be an increased need for interdisciplinary healthcare teamwork, collaboration with scientists, economists, and politicians” (Hoffman et al., 2020, p. 180). The critical question is: What will healthcare organizations, healthcare professionals, healthcare professional education, communities, and the government (local, state, federal) learn from this experience to prepare for possible, future crises?
| Stop and Consider 5 |
|---|
| The problems of violence and opioid use affect all nurses in their practice. |
Global Healthcare Concerns and International Nursing
The WHO is the major international health organization that focuses on “building a better, healthier future for people all over the world” (2021). The organization focuses on global health, providing guidance about many global health risks and problems (2023d). Member States of WHO globally and in its European Region (including the United States) are committed to implementing three interconnected strategic priorities that constitute the pillars of WHO's Thirteenth General Program of Work, 2019-2023 (GPW 13) (WHO, 2023e):
- moving towards universal health coverage (UHC)
- protecting people better against health emergencies
- ensuring healthy lives and well-being for all at all ages.
These core priorities are related to the WHO 2030 Sustainable Development Goals (SDGs) agenda. These goals focus on a comprehensive vision for sustainable development that (WHO, 2023f):
- is global, rather than limited to “developing” countries as was the case with the Millennium Development Goals (MDGs)
- based on values, such as equity and respect for human rights
- relies on approaches, such as sustainable financing, scientific research and innovation, and monitoring and evaluation
- requires a new way of working, involving intersectoral action by multiple stakeholders
- aims to strengthen health systems toward UHC
The United States, through the work done by the HHS, also applies these goals as part of its collaboration with WHO.
Global healthcare concerns change, and some changes are significant both in their impact and their costs-such as during the COVID-19 pandemic. Emerging infections have long been a concern and represent a major global health concern, for example, bacteria that are antibiotic-resistant (Cleeson, 2016). Other recent examples of infectious diseases are the Ebola virus and the Zika virus and the long-term impact on infants born when mothers are infected. War and refugees/displaced persons who need medical care and support services, such as housing, food, education, and so on, continue to be global health problems-increasing the problem of displaced persons, which can be caused by wars, violence, climate crises, food insecurity, and other challenges. These situations are typically complex political situations and involve problems related to coordination and speed in meeting the needs. The refugee situation is much more complex and will last a long time-affecting multiple countries and many people of all ages. The WHO provided critical global leadership assisting with the global response to COVID-19. The organization's leaders spoke out about the need to ensure that all countries have access to the vaccine to better ensure equity and reduce risk globally, which is a very troublesome problem (WHO, 2021). This experience will influence future global health concerns and how countries cooperate and collaborate, such as the United States. Nurses should be aware of WHO and its relationship to national health. For example, the International Council of Nursing (ICN) is also involved in global health by providing a voice for nursing throughout the world. Its stated mission is “to represent nursing worldwide, advance the profession, promote the well-being of nurses, and advocate for health in all policies” (ICN, 2023). The ICN and WHO focus on the health of individuals, families, and communities and work collaboratively with the ICN supporting the WHO Vaccine Equity Declaration (ICN, 2021).