Population: Adults without diagnosis or symptoms of colorectal cancer.
Organizations
 AAFP 2021, USPSTF 2021, ACS 2020, ACG 2021, US Multi-Society Task Force on Colorectal Cancer (USMSTF-CC) 2017, 2020, ACP 2019, Canadian Task Force (CTF) 2016, NCCN 2021, ASCO 2019
AAFP 2021, USPSTF 2021, ACS 2020, ACG 2021, US Multi-Society Task Force on Colorectal Cancer (USMSTF-CC) 2017, 2020, ACP 2019, Canadian Task Force (CTF) 2016, NCCN 2021, ASCO 2019
Recommendations
–Screen all adults, with age ranges, modalities, and frequencies varying by organization.
–Adults with elevated risk are outside the scope of these recommendations.1

Practice Pearls
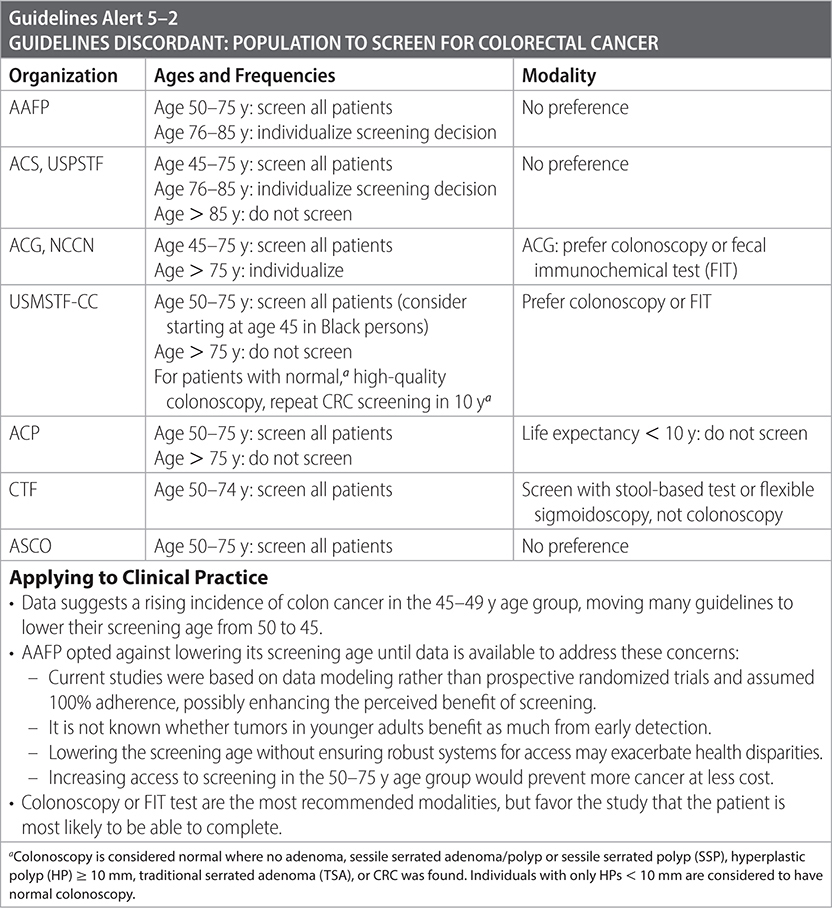
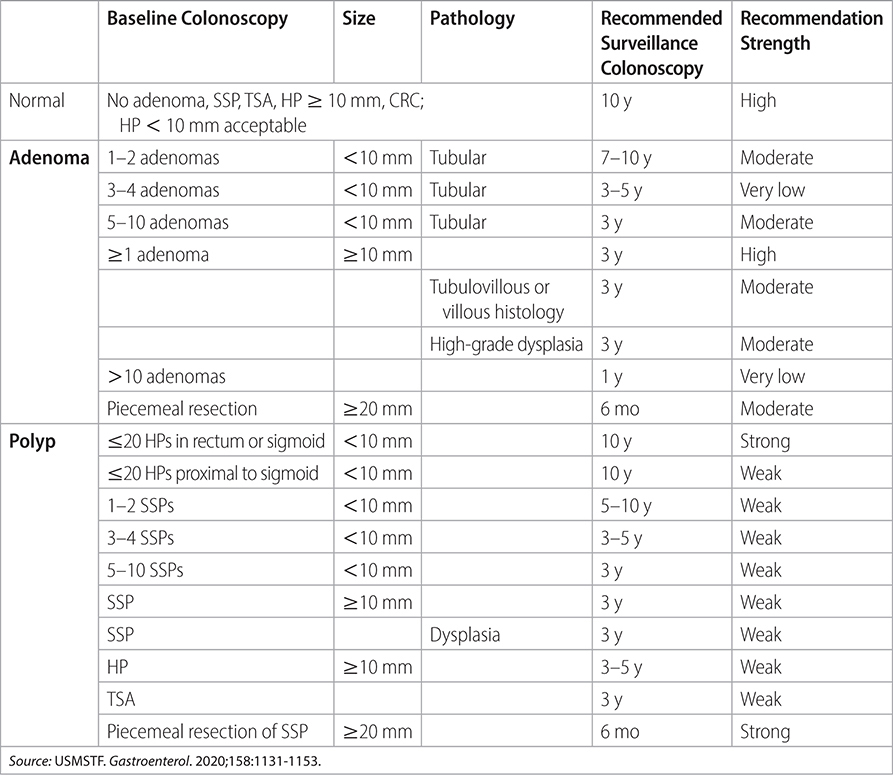
• Recommendations for follow-up testing after the initial colonoscopy are detailed in Table 5–1.
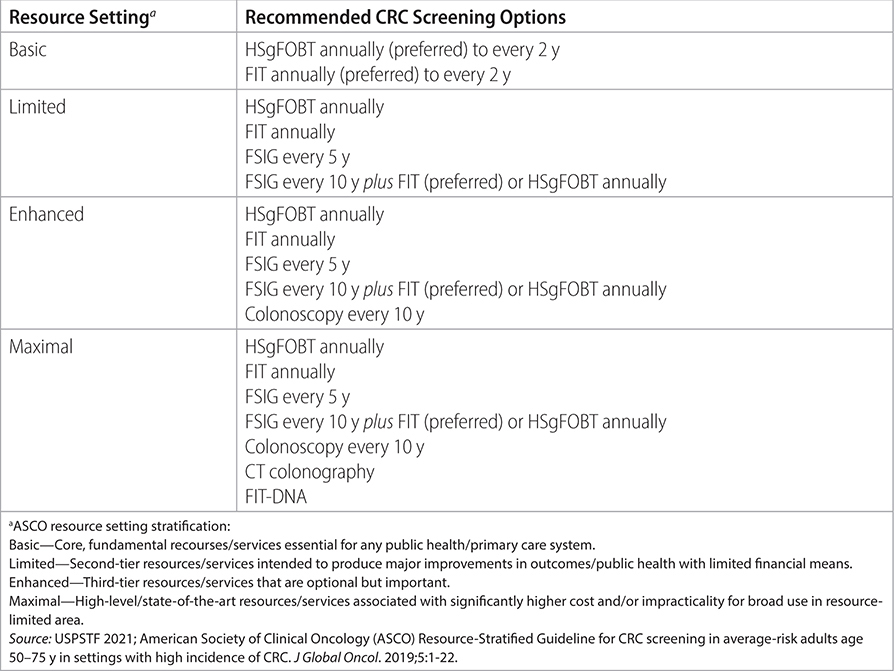
• Recommendations for screening in resource-limited settings are detailed in Table 5–2.
• USPSTF, ACG, ACS, and NCCN all recognize that evidence for initiating screening at age 45 is not as strong. USPSTF gives starting at age 45 a “B” recommendation while starting at age 50 is an “A” recommendation. ACG “recommends” starting at age 50 and “suggests” starting at age 45. Incidence of colorectal adenocarcinoma in adults 40- to 49-y-old has increased by almost 15% from 2000–2002 to 2014–2016. (Ann Intern Med. 2021;174)
• Acceptable screening methods1,2,3:
- Guaiac fecal occult blood test (gFOBT-guaiac based or FIT 4
- Flexible sigmoidoscopy every 5 y with reflex colonoscopy if abnormal.
- FIT5 annually plus flexible sigmoidoscopy every 10 y.
- Colonoscopy every 10 y.
- CT colonoscopy every 5 y.
• Follow-up/surveillance colonoscopy according to findings: refer to this chapter for updated USMSTF 2020 recommendations.
• FOBT alone decreased colorectal cancer (CRC) mortality by 33% compared with those who were not screened. (Gastroenterology. 2004;126:1674)
• Accuracy of colonoscopy is operator dependent—rapid withdrawal time, poor prep, and lack of experience will increase false-negatives. (N Engl J Med. 2006;355:2533) (Ann Intern Med. 2012;156:692) (Gastroenterology. 2015;110:72)
• Multitargeted DNA stool testing vs. iFOBT with more cancers detected (92.3% vs. 73.8%) but more false-positives with DNA test. (N Engl J Med. 2014;370:1287-1306)
• Percentage of US adults receiving some form of CRC screening increased from 44% in 1999 to 63% in 2008. The goal was 80% by 2018. (CA Cancer J Clin. 2015;65:30) (Arch Intern Med. 2011;171:647; 2012;172:575). However, the percentage increased from 58.7% in 2010 to 65.5% in 2018 (www.cdc.gov/mmwr/volumes/69/wr/mm6929a6.htm). In 2016, an estimated 134,000 new cases of CRC were diagnosed and 49,000 Americans died of CRC. Median age at diagnosis is 68. (CA Cancer J Clin. 2016;66:7)
• Colonoscopy vs. iFOBT testing in CRC with similar detection of cancer, but more adenomas identified in the colonoscopy group. (N Engl J Med. 2012;366:687,697)
• A normal screening colonoscopy may provide reassurance for up to 17 y. (Ann Intern Med. 2020;173(2):81-91)
TABLE 5–1 US MULTI-SOCIETY TASK FORCE RECOMMENDATIONS FOR FOLLOW-UP AFTER BASELINE SCREENING COLONOSCOPY IN AVERAGE-RISK ADULTS
Sources
–ACS. 2020. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html
–USPSTF. JAMA. 2016;315(23):2564-2575.
–ACG. Am J Gastroenterol. March 2021;116(3):458-479.
–ACP. Ann Int Med. 2019;171(9):643-654.
–USMSTF. Gastroenterol. 2020;158:1131-1153.
TABLE 5–2 SCREENING IN HIGH-INCIDENCE SETTINGS STRATIFIED BY RESOURCE AVAILABILITY
–USMSTF. Am J Gastroenterol. 2017;112(7):1016-1030.
–CTF. CMAJ. 2016;188(5):340-348.
–NCCN. 2021. https://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf
–ASCO. J Global Oncol. 2019;5:1-22.
Organizations
 AAFP 2018, NCCN 2020
AAFP 2018, NCCN 2020
Prevention Recommendations
–Modifiable risk factors:
• Diet:
 Advise patients to increase consumption of fruits, nonstarchy vegetables, and whole grains. Preferentially optimize nutrition from natural food sources rather than dietary supplements.
Advise patients to increase consumption of fruits, nonstarchy vegetables, and whole grains. Preferentially optimize nutrition from natural food sources rather than dietary supplements.
 Cholesterol: 2-fold increased risk of CRC with increased intake.
Cholesterol: 2-fold increased risk of CRC with increased intake.
 Fat: 25% increased risk of serrated polyps with increased fat intake.
Fat: 25% increased risk of serrated polyps with increased fat intake.
 Dairy: 15% reduced risk of CRC with >8 oz of cow’s milk daily.
Dairy: 15% reduced risk of CRC with >8 oz of cow’s milk daily.
 Fiber: no reduced risk of CRC or adenomatous polyps with increased fiber intake.
Fiber: no reduced risk of CRC or adenomatous polyps with increased fiber intake.
 Red and processed meat: 22% increased risk of CRC with increased red and processed meat intake.
Red and processed meat: 22% increased risk of CRC with increased red and processed meat intake.
• Lifestyle:
 Alcohol: 8% increased risk of CRC and 24% increased risk of serrated polyps. Reducing alcohol intake does not clearly lower risk for CRC or polyps.
Alcohol: 8% increased risk of CRC and 24% increased risk of serrated polyps. Reducing alcohol intake does not clearly lower risk for CRC or polyps.
 Cigarettes: 114% increased risk of high-risk adenomatous polyps and CRC in current smokers.
Cigarettes: 114% increased risk of high-risk adenomatous polyps and CRC in current smokers.
 Obesity: bariatric surgery associated with 27% reduced risk of CRC in obese individuals. Increased BMI is associated with increased mortality from CRC.
Obesity: bariatric surgery associated with 27% reduced risk of CRC in obese individuals. Increased BMI is associated with increased mortality from CRC.
 Occupational physical activity: 25% decreased risk of colon cancer and 12% decreased risk of rectal cancer.
Occupational physical activity: 25% decreased risk of colon cancer and 12% decreased risk of rectal cancer.
 Recreational physical activity: 20% decreased risk of colon cancer and 13% decreased risk of rectal cancer.
Recreational physical activity: 20% decreased risk of colon cancer and 13% decreased risk of rectal cancer.
• Medications:
 Statins: weak evidence that statin use ≥5 y is associated with decreased risk of advanced adenomatous polyps.
Statins: weak evidence that statin use ≥5 y is associated with decreased risk of advanced adenomatous polyps.
 Calcium: 26% reduced risk of adenomatous polyps; 22% reduced risk of CRC in individuals taking 1400 mg daily calcium compared to 600 mg.
Calcium: 26% reduced risk of adenomatous polyps; 22% reduced risk of CRC in individuals taking 1400 mg daily calcium compared to 600 mg.
–Polyp removal:
• Based on fair evidence, removal of adenomatous polyps reduces the risk of CRC, especially polyps >1 cm. (Ann Intern Med. 2011;154:22) (Gastrointest Endosc. 2014;80:471)
• Based on fair evidence, complications of polyp removal include perforation of the colon and bleeding estimated at 7–9 events per 1000 procedures.
–Interventions without benefit:
• Vitamin D.
• Folic acid.
• Antioxidants.
Sources
–Am Fam Physician. 2018;97(10):658-665.
–NCCN. Colorectal Cancer Screening. 2020:1-61.
Population: Adults at high risk of colon cancer.
Organizations
 USMSTF on CRC 2017, NCCN 2021, ACG 2021
USMSTF on CRC 2017, NCCN 2021, ACG 2021
Screening Recommendations
–Screen adults with family history of early CRC1 or advanced adenoma (AA) with colonoscopy every 5 y starting at age 40 y or 10 y prior to earliest age of diagnosis of first-degree relative.
–Use Amsterdam I and II criteria to diagnose hereditary nonpolyposis CRC (HNPCC), with subsequent genetic screen for Lynch syndrome (LS).
• Amsterdam I criteria:
 ≥3 relatives with histologically verified CRC, one of which is a first-degree relative of the other two. Diagnosis of familial adenomatous polyposis (FAP) excluded.
≥3 relatives with histologically verified CRC, one of which is a first-degree relative of the other two. Diagnosis of familial adenomatous polyposis (FAP) excluded.
 ≥2 generations with CRC.
≥2 generations with CRC.
 ≥1 CRC diagnosis before age 50 y.
≥1 CRC diagnosis before age 50 y.
• Amsterdam II criteria:
 ≥3 relatives with histologically verified HNPCC-associated cancer (colorectal, endometrial, small bowel, ureter, renal pelvis), one of which is a first-degree relative of the other two. Diagnosis of FAP excluded.
≥3 relatives with histologically verified HNPCC-associated cancer (colorectal, endometrial, small bowel, ureter, renal pelvis), one of which is a first-degree relative of the other two. Diagnosis of FAP excluded.
 ≥2 generations with CRC.
≥2 generations with CRC.
 ≥1 CRC diagnosis before age 50 y.
≥1 CRC diagnosis before age 50 y.
–Lynch syndrome (LS): screening colonoscopy every 1–2 y for persons with LS or at-risk (first-degree relatives of those affected), starting at age 20–25 y, or 2–5 y before youngest age of family CRC diagnosis if diagnosed before age 25 y.
–Family CRC Type X syndrome: screening colonoscopy every 3–5 y beginning 10 y before the age at diagnosis of the youngest affected relative.
Sources
–USMSTF. Am J Gastroenterol. 2017;112(7):1016-1030.
–NCCN. 2021. https://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf
–ACG. Am J Gastroenterol. March 2021;116(3):458-479.