Population: Women who are pregnant.
Organizations
 AAFP, USPSTF, NICE, ACOG
AAFP, USPSTF, NICE, ACOG
Recommendation
–See Table 29–5 for routine prenatal care guidance and Table 29–6 for perinatal recommendations.
TABLE 29–5 COMPILED RECOMMENDATIONS FOR ROUTINE PRENATAL CARE |
|---|
Preconception visit |
1. Measure height, weight, and blood pressure. 2. Assess immunization status for tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap); measles–mumps–rubella; hepatitis B; rubella, and varicella. Immunize as indicated. Live vaccines should be administered at least 1 mo prior to pregnancy. 3. Assess all patients for pregnancy risk: substance abuse, domestic violence, sexual abuse, psychiatric disorders, risk factors for preterm labor, exposure to chemicals or infectious agents, hereditary disorders, gestational diabetes, or chronic medical problems. Initiate interventions to optimize maternal, fetal, and pregnancy outcomes. 4. Educate patients about proper nutrition; offer weight reduction strategies for patients with obesity. 5. With the exception of universal HIV and hepatitis C screening, screening lab tests should be considered selectively in appropriate high-risk groups. 6. Initiate folic acid 400–800 μg/d; 4 mg/d for a history of a child affected by a neural tube defect. |
Initial prenatal visit |
1. Confirm pregnancy. 2. Assess medical, surgical, obstetric, psychosocial, and family history, and perform a complete physical examination. Record baseline blood pressure, height, weight, and calculate BMI. 3. Order CBC, blood type (ABO & RhD) and antibody screen, rubella titer, varicella titer, HIV, syphilis screening, hepatitis B surface antigen, hepatitis C antibody, urine NAAT for gonorrhea and chlamydia, urinalysis (proteinuria, glucosuria), urine culture. Pap smear if not up to date. Other selective screening tests as indicated. 4. Order an obstetrical ultrasound for dating if any of the following: beyond 16-wk gestational age, unsure of last menstrual period, size/date discrepancy on examination, or for inability to hear fetal heart tones by 12 gestational weeks. 5. Discuss fetal aneuploidy screening and counseling regardless of maternal age. 6. Prenatal testing for sickle cell anemia (African descent), thalassemia (African, Mediterranean, Middle Eastern, Southeast Asians), Canavan disease and Tay-Sachs (Jewish patients), cystic fibrosis (Whites and Ashkenazi Jews), and fragile X syndrome (family history of nonspecified mental retardation) when indicated. 7. Test for tuberculosis in medium- to high-risk patients.a 8. Consider a 1-h 50-g glucose tolerance test for certain high-risk groups.b 9. Obtain an operative report in all women who have had a prior cesarean section. 10. Psychosocial risk assessment for mood disorders, substance abuse, or domestic violence. |
Frequency of visits for uncomplicated pregnancies |
1. Every 4 wk until 28 gestational weeks; q2 wk from 28 to 36 wk; weekly >36 wk. 2. Offer a single ultrasound examination at 18- to 20-wk gestation if not indicated earlier (ACOG). Consider offering routine ultrasonography between 11- and 14-wk gestation even if not medically indicated (NICE). There is no evidence to support routine ultrasonography in uncomplicated pregnancies. |
Routine checks at follow-up prenatal visits |
1. Assess weight, blood pressure, and urine for glucose and protein. 2. Exam: edema, fundal height, and fetal heart tones at all visits; fetal presentation starting at 36 wk. 3. Ask about regular uterine contractions, leakage of fluid, vaginal bleeding, or decreased fetal movement. 4. Discuss labor precautions. |
Antepartum lab testing |
1. Offer first trimester, second trimester, or combined testing to screen for fetal aneuploidy; invasive diagnostic testing for fetal aneuploidy should be available to all women regardless of maternal age. a. First trimester. b. Second trimester screening options: amniocentesis at 14 wk; a Quad Marker Screen at 16–18 wk; and/or a screening ultrasound with nuchal translucency assessment. 2. Consider serial transvaginal sonography of the cervix every 2–3 wk to assess cervical length for patients at high risk for preterm delivery starting at 16 wk. 3. No role for routine bacterial vaginosis screening. 4. 1 h 50-g glucose tolerance test in all women between 24 and 28 wk. 5. Screen for group B beta-hemolytic streptococcus (GBS) colonization between 36- and 38-wk gestation with rectovaginal swab. 6. Recommend weekly amniotic fluid assessments and twice weekly nonstress testing starting at 41 wk. |
Prenatal counseling |
1. Cessation of smoking, drinking alcohol, or use of any illicit drugs. 2. Avoid cat litter boxes, hot tubs, certain foods (ie, raw fish or unpasteurized cheese). 3. Proper nutrition and expected weight gain: National Academy of Sciences advises weight gain 28–40 lb (prepregnancy BMI < 20), 25–35 lb (BMI 20–26), 15–25 lb (BMI 26–29), and 15–20 lb (BMI ≥ 30). 4. Inquire about domestic violence and depression at initial visit, at 28 wk, and at postpartum visit. 5. Recommend regular mild-to-moderate exercise 3 or more times a week. 6. Avoid high-altitude activities, scuba diving, and contact sports during pregnancy. 7. Benefits of breastfeeding vs. bottle-feeding. 8. Discuss postpartum contraceptive options (including tubal sterilization) during third trimester. 9. Discuss analgesia and anesthesia options and offer prenatal classes at 24 wk. 10. Discuss repeat C-section vs. vaginal birth after cesarean (if applicable). 11. Discuss the option of circumcision if a boy is delivered. 12. Avoid air travel and long train or car trips beyond 36 wk. 13. Discuss the uncertain benefit of kick counting in the prevention of stillbirth. Kick counting may be associated with increased risk of iatrogenic preterm birth, induction of labor, and cesarean birth. |
Prenatal interventions |
1. Suppressive antiviral medications starting at 36 wk for women with a history of genital herpes. 2. Cesarean delivery is indicated for women who are HIV positive or have active genital herpes and are in labor. 3. For patients who report a history of abuse, offer interventions and resources to increase their safety during and after pregnancy. |
4. For patients with severe depression, consider treatment with an SSRI (avoid paroxetine if possible). 5. Rh immune globulin 300 μg IM for all Rh-negative women with negative antibody screens between 26 and 28 wk. 6. Refer for nutrition counseling at 10–12 wk for BMI <20 or at any time during pregnancy for inadequate weight gain. 7. Start prenatal vitamins with iron and folic acid 400–800 μg/d and 1200 mg elemental calcium/d starting at 4-wk preconception (or as early as possible during pregnancy) and continued until 6-wk postpartum. 8. Give inactivated influenza vaccine IM to all pregnant women during influenza season. 9. Give Tdap vaccine during each pregnancy between 27- and 36-wk gestation. 10. Consider progesterone therapy IM weekly or intravaginally daily to women at high risk for preterm birth. 11. Recommend an external cephalic version at 37 wk for all noncephalic presentations. 12. Offer labor induction to women at 41 wk by good dates. 13. Treat all women with confirmed syphilis with penicillin G during pregnancy. 14. Treat all women with gonorrhea with ceftriaxone; follow treatment with a test of cure. 15. Treat all women with chlamydia with azithromycin; follow treatment with a test of cure. Doxycycline is contraindicated during the second and third trimesters of pregnancy. 16. Treat all GBS-positive women with penicillin G when in labor or with spontaneous rupture of membranes. 17. Offer group prenatal care as an alternative to traditional prenatal care if available and involve partners. 18. Discuss and document preferences about mode of birth early on and confirm toward the end of pregnancy, as preferences may have changed. |
Postpartum interventions |
1. Treat all infants born to HBV-positive women with hepatitis B immunoglobulin (HBIG) and initiate HBV vaccine series within 12 h of life. 2. All women with a positive tuberculosis skin test and no evidence of active disease should receive a postpartum chest x-ray; treat with isoniazid 300 mg PO daily for 9 mo if chest x-ray is negative. 3. Administer a Tdap booster if tetanus status is unknown or the last Td (tetanus-diphtheria) vaccine was >10 y ago. 4. Administer an MMR vaccine to all rubella nonimmune women. 5. Offer HPV vaccine to all women ≤26 y who have not been immunized. 6. Initiate contraception. 7. Repeat Pap smear at 6-wk postpartum check. |
aPost gastrectomy, gastric bypass, immunosuppressed (HIV-positive, diabetes, renal failure, chronic steroid/immunosuppressive therapy, head/neck or hematologic malignancies), silicosis, organ transplant recipients, malabsorptive syndromes, alcoholics, intravenous drug users, close contacts of persons with active pulmonary tuberculosis, medically underserved, low socioeconomic class, residents/employees of long-term care facilities and jails, health care workers, and immigrants from endemic areas. bOverweight (BMI ≥ 25) and an additional risk factor: physical inactivity; first-degree relative with DM; high-risk ethnicity (eg, Black, Latina, American Indian, Asian American, Pacific Islander persons); history of gestational diabetes mellitus (GDM); prior baby with birthweight >9 lb; unexplained stillbirth or malformed infant; HTN on therapy or with BP ≥140/90 mmHg; HDL cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L); polycystic ovary syndrome; history of impaired glucose tolerance or HgbA1c ≥5.7%; acanthosis nigricans; cardiovascular disease; or ≥2+ glucosuria. Sources: Adapted from http://www.icsi.org/prenatal_care_4/prenatal_care_routine_full_version_2.html; Am Fam Physician. 2014;89(3):199-208. USPSTF. Hepatitis C Virus Infection in Adolescents and Adults: Screening. 2020. NICE. Antenatal Care (NG201). 2021. NICE. Inducing Labour (NG207). 2021. NICE. Postnatal Care (NG194). 2021. ACOG. Practice Bulletin No 229. Antepartum Fetal Surveillance. 2021. |
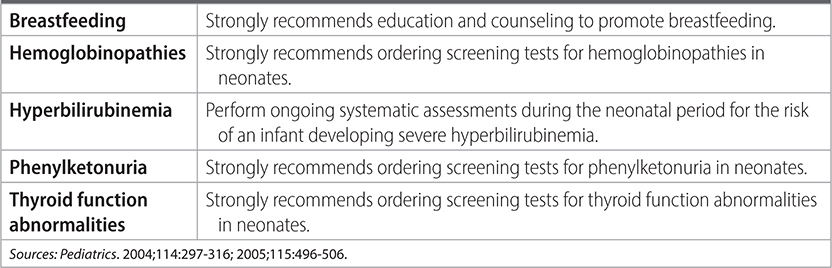
TABLE 29–6 AAP AND AFP PERINATAL AND POSTNATAL GUIDELINES