Population: Mature adolescents and adults who are obese.
Organizations
 JCEM 2015, CMAJ 2020, AGA 2022, NICE 2022
JCEM 2015, CMAJ 2020, AGA 2022, NICE 2022
Recommendations
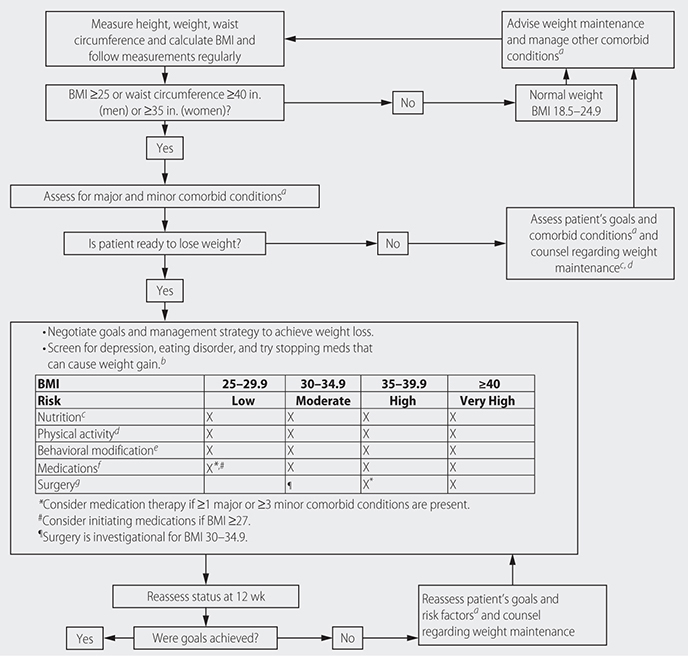
–Approach to obesity management (CMAJ) (Fig. 21–3):
• Assess and acknowledge provider bias regarding obesity.
• Ask permission to discuss obesity/weight with patient, approach conversations in a nonjudgmental way, and praise success to encourage continued positive behavior.
• Assess their story (subjective experiences as well as objective measures such as BMI, height, waist circumference, BP, lipid panel, A1c, LFT measurements).
• Discuss and agree on choice of interventions with patient and tailor weight management program to patient’s needs/preferences, initial fitness, health status, and lifestyle. Consider factors including weight-related comorbidities, ethnicity, and special education needs and disabilities. (NICE)
• Use clinical judgment to decide when to measure height and weight. Interpret BMI with caution, especially in patients age 65+, with high muscle mass, and/or of Asian or African descent. (NICE)
FIG. 21–3 APPROACH TO OBESITY INTERVENTIONS.
• Recognize that surprise, denial, disbelief, or anger about health situation may diminish patient’s ability/willingness to change. Offer patients who are not yet ready to change information on the benefits of losing weight, and a chance to return for further consults when ready to discuss again. (NICE)
• Assess possible reasons for weight gain, including patient’s view of weight/diagnosis and attitudes about eating and physical activity that may be unhelpful, previous experiences/attempts, readiness to adopt changes. (NICE)
• Exercise (30–60 min moderate-intensity activity on most days of the week), with added resistance training.
• Medical Nutrition Therapy facilitated by registered dietician when possible.
• Weight loss of 5%–7% in setting of prediabetes, 7%–15% in diagnosed T2DM.
• Ensure weight management programs include behavior change strategies to increase physical activity levels and improve eating behavior (NICE). Offer multicomponent psychological care in a longitudinal setting.
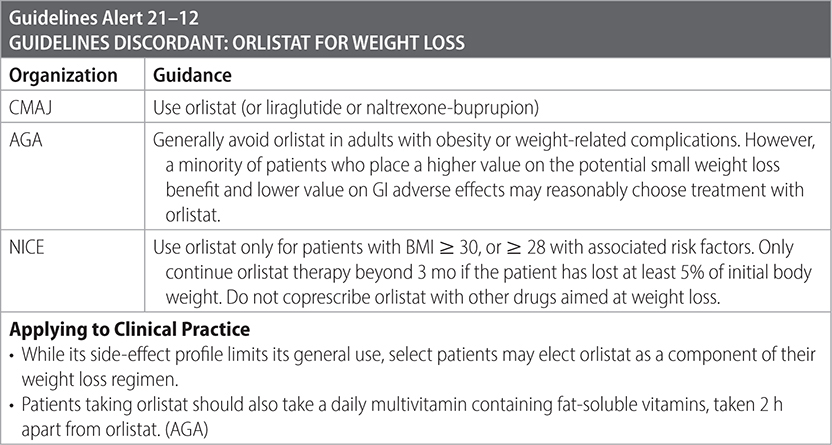
• Pharmacotherapy: used when BMI ≥ 30, or ≥ 27 with adiposity-related complications, in conjunction with intensive lifestyle changes listed above. Choices for pharmacotherapy include semaglutide, liraglutide, naltrexone-bupropion combination, phentermine-topiramate ER. Minimize exposure to pharmacotherapy with the side effect of weight gain used for other medical conditions.
• Bariatric surgery considerations: BMI ≥ 40, BMI ≥ 35 with at least 1 adiposity-related disease, BMI between 30 and 35 with presence of poorly controlled T2DM despite maximal medical therapy.
• Do not offer adjustable gastric banding procedure due to long-term treatment failure and rate of complications.

Practice Pearl
• Bariatric surgery does improve all-cause mortality and comorbidities such as diabetes, hypertension and sleep apnea. (PLoS Med. 2020;17(7):e1003206)
Sources
–CMAJ. 2020;192:E875-91. doi: 10.1503/cmaj.191707
–Adapted from the ICSI Guideline on the Prevention and Management of Obesity. https://academic.oup.com/jcem/article/100/2/342/2813109/Pharmacological-Management-of-Obesity-An-Endocrine.
Population: Children and adolescents (2–18 y) with obesity.
Organizations
 NICE 2022, AAP 2023
NICE 2022, AAP 2023
Recommendations
Evaluation
–Ask permission from patient and their families/caregivers before discussing weight, and conduct all discussions in a manner that is supportive, age-appropriate, nonjudgmental, and recognizes cultural values. Understand that these discussions may elicit strong emotional responses such as sadness/anger, and acknowledge and validate these responses, keeping focus on patient’s health.
–Approach to diagnosis (AAP):
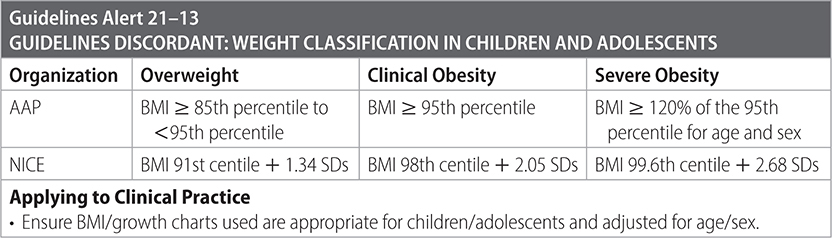
• Screening: Measure height and weight, calculate BMI, and assess BMI percentile/weight classification using age- and sex-specific CDC growth charts or growth charts for children with severe obesity at least annually for all children 21–18 y to screen for overweight/obesity.
• Evaluation: If BMI indicates overweight or obese (see Guidelines Alert 21–13), conduct full evaluation for overweight/obesity and obesity-related comorbidities by using a comprehensive patient history, mental and behavioral health screening, SDoH evaluation, physical examination, and diagnostic studies.
• Comorbidities: Evaluate for:
 Dyslipidemia.
Dyslipidemia.
 Prediabetes and/or DM, with fasting plasma glucose or HbA1c.
Prediabetes and/or DM, with fasting plasma glucose or HbA1c.
 NAFLD.
NAFLD.
 Hypertension, by measuring BP at every visit starting at age 3 y in children with overweight or obesity.
Hypertension, by measuring BP at every visit starting at age 3 y in children with overweight or obesity.
 OCA.
OCA.
 PCOS.
PCOS.
 Depression, and conduct annual evaluation for depression in adolescents 12 y+ with a formal self-report tool.
Depression, and conduct annual evaluation for depression in adolescents 12 y+ with a formal self-report tool.
• Perform a musculoskeletal review of systems and physical examination (eg, internal hip rotation in growing child, gait) as part of their evaluation for obesity.
• Maintain a high degree of suspicion for idiopathic intracranial hypertension with new-onset or progressive headaches in the context of significant weight gain, especially for females.
–Approach to diagnosis (NICE):
• Consider assessment of comorbidity for children w/BMI at or above 98th centile.
• In addition to BMI, also consider using waist-to-height ratio in children and adolescents age 5 y+ to assess and predict health risks associated with central adiposity (such as type 2 diabetes, hypertension, or cardiovascular disease).
–Treat overweight and obesity concurrently with related comorbidities.

Management
–Involve children/adolescents and their families/caregivers in decision-making.
–Provide or refer children with overweight or obesity to intensive health behavior and lifestyle treatment (IHBLT). When an IHBLT program is not available, provide the most intensive program possible, given available community resources and other specialty programs. (AAP)
–Aim to create a supportive environment that helps the child and their family make changes to lifestyle, behavioral, and environmental factors. Ensure that interventions address lifestyle within the family and in social settings, and encourage parents/caregivers to take main responsibility for lifestyle changes in children, especially those under 12 y. Involve behavioral health specialists when possible.
–Encourage increasing physical activity (60+ min/d) and reducing inactive behaviors. Choose an activity with the child, appropriate to ability and confidence. (NICE). Exercise specialists can provide counseling and training to engage children and families in noncompetitive, cooperative, and fun activities. (AAP)
–Offer nutritional advice or refer to a dietician. Dietary recommendations should be part of multicomponent intervention, as a dietary approach alone is not recommended for children and adolescents (NICE). Total energy intake should be below energy expenditure, and changes should be sustainable. Focus on increasing healthful food consumption. (AAP)
–Consider offering patients 12 y+ with obesity weight loss pharmacotherapy, according to medication indications, risks, and benefits, as an adjunct to health behavior and lifestyle treatment. Pharmacotherapy is generally appropriate for children with more severe degrees of obesity and/or comorbidities.
–Consider offering referral for adolescents 13 y+ with severe obesity for evaluation for metabolic and bariatric surgery to local or regional comprehensive multidisciplinary pediatric metabolic and bariatric surgery centers. (AAP)
–Treat using a family-centered approach that acknowledges obesity’s biological, social, and structural drivers. Assess individual and contextual risk factors for obesity, and tailor interventions to the needs and preferences of the child and family, taking into account the child’s physical and mental/emotional health status, as well as SDoHs such as ethnicity, socioeconomic status, household and familial influences/complexities, and access to resources. Recognize and address systemic racial and socioeconomic inequities that often result in disparities in obesity risk and outcomes, including systemic disparities in access to resources and quality health care services. (AAP)
–The aim of weight management programs for children/adolescents can vary; focus on weight management or loss depending on age/stage of growth. (NICE)
–Consider whether patient has experienced weight-based stigma or bullying, which may contribute to binge eating, social isolation, avoiding health care services, and decreased physical activity. (NICE)
–Use long-term care strategies, and provide ongoing medical monitoring and access to treatment for obesity and associated comorbidities, appropriate reassessments of medical and psychological risks and comorbidities, and appropriate modifications to treatment plans throughout childhood and adolescence into young adulthood. (AAP)
Practice Pearl
• Drug treatment is currently not recommended for children under 12 y for the sole indication of obesity. (AAP, NICE). However, it may be appropriate in exceptional circumstances, when severe comorbidities are present. Prescribing should be started and monitored only in specialist pediatric settings. (NICE). AAP notes that the use of pharmacotherapy to aid BMI reduction in children is a rapidly evolving field; new evidence may lead to additional options for children under 12 y in the future.
Sources
–NICE. Obesity: Identification, Assessment and Management. 2022. www.nice.org.uk/guidance/cg189.
–AAP. Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents with Obesity. 2023;151(2):e2022060640.