Population: Children with acute otitis media.
Organizations
 NICE 2022, AAP 2019, CDC 2017
NICE 2022, AAP 2019, CDC 2017
Recommendations
Evaluation
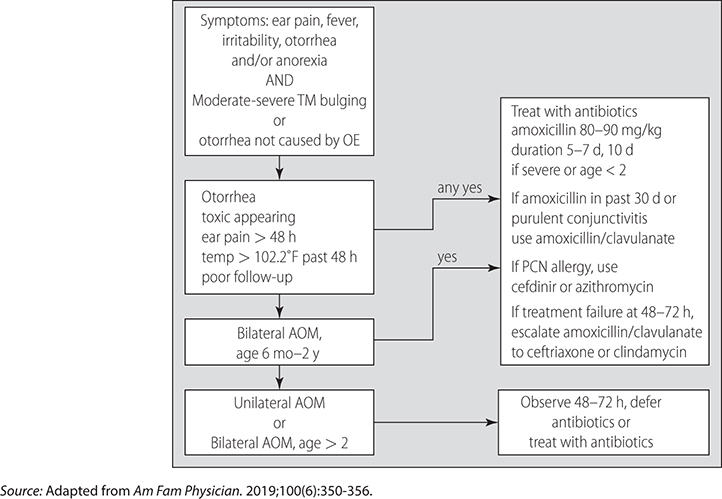
–See Fig. 26–1 for diagnostic and treatment pathway.
–Diagnose when bulging TM with effusion or otorrhea (not due to otitis externa).
–When appropriate, use non-antibiotic treatments (as most cases resolve without antibiotic treatment):
• Prescribe acetaminophen or ibuprofen, ensure correct dosing.
• Offer eardrops with anesthetic or analgesic improve pain.
• Do not prescribe decongestants, antihistamines, or oral steroids.
–Antibiotic strategy:
• Consider watchful waiting with back up antibiotic prescription if no improvement at 48 h with pain control for mild unilateral cases in children 6–23 mo or >24 mo with unilateral or bilateral illness.
• Antibiotic selection: use amoxicillin first-line 125–500 mg TID (based on age). Amoxicillin-clavulanate has more side effects.
• Clarithromycin (NICE) or cefdinir (AAP) are alternatives in allergy or intolerance.
• Use amoxicillin-clavulanate if not improved in 2–3 d on amoxicillin or had taken amoxicillin within the past 30 d (0.25 mL/kg of 125/31 mg suspension based on weight and age).
• Duration of antibiotic: 5–7 d, consider 10 d if <2 or severe.
• Do not use prophylaxic antibiotics not recommended.
Practice Pearls
• Usually self-limited, caused by viruses and bacteria (commonly: Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Streptococcus pyogenes).
• Complications: temporary hearing loss and tympanic membrane (TM) perforation (antibiotics do not affect rates of these complications).
• Antibiotics do not reduce pain at 24 h. There is a small benefit to pain at 23 d. They do reduce TM perforations, but the effect is small.
• Antibiotic benefits are greatest for children ≤2 y and children with otorrhea suggesting perforation.
• Risk factors include age <5 y, craniofacial anomalies, family history, birth weight <2.5 kg, male sex, birth <37 wk EGA, prior ear infections, recent viral URI, White ethnicity.
• Potentially modifiable risk factors include exposure to tobacco smoke and air pollution, crowded living conditions, GERD, lack of breast feeding, pacifier use after 6 mo, supine bottle feeding.
FIG. 26–1 DIAGNOSIS AND TREATMENT OF AOM IN CHILDREN.
Sources
–https://www.nice.org.uk/guidance/ng91
–https://www.cdc.gov/antibiotic-use/clinicians/pediatric-treatment-rec.html
–Pediatrics. 2013;131(3):e964-e999.
–Am Fam Physician. 2019;100(6):350-356.