| DRUG and COMMON INDICATIONS | MECHANISM OF ACTION | CLINICAL POINTS |
|---|
Fludarabine
- Chronic lymphocytic leukemia (CLL) (e.g., fludarabine, cyclophosphamide, rituximab [FCR])
- AML (e.g., fludarabine, cytarabine, idarubicin, filgrastim [FLAG-IDA])
- Allogeneic stem cell transplant conditioning
- Waldenstrom macroglobulinemia (in combination with rituximab)
- NHL (for relapsed or refractory)
| 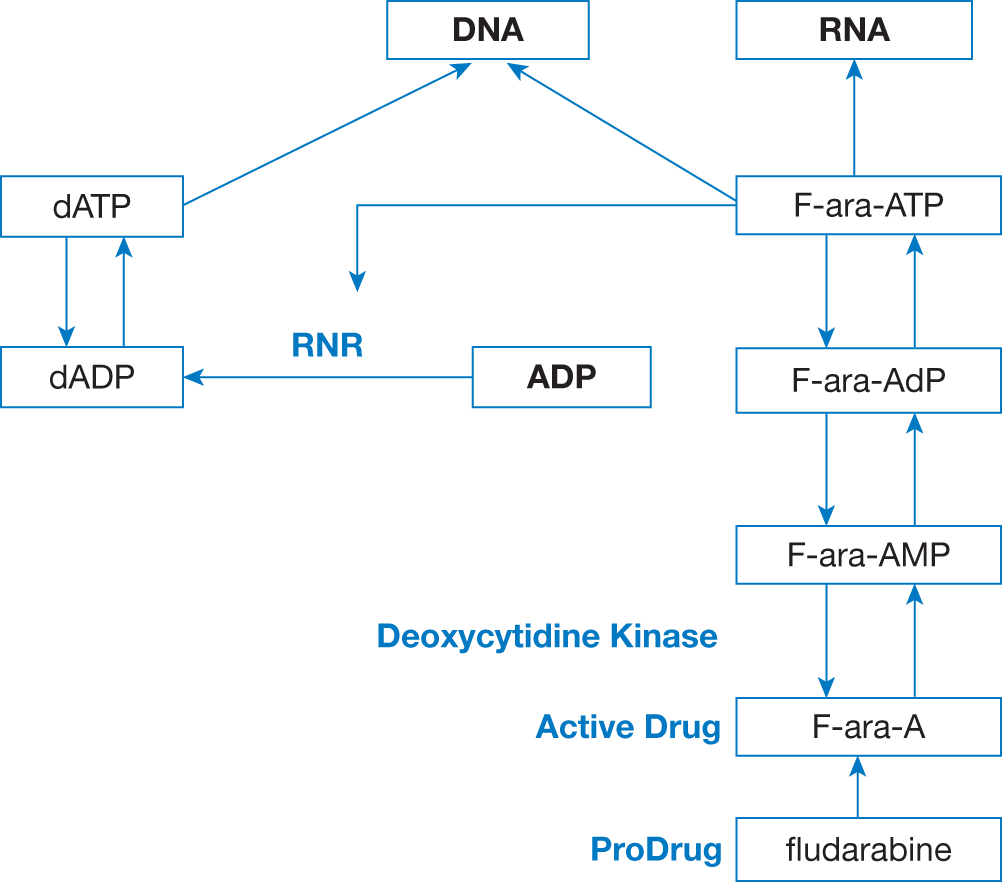 
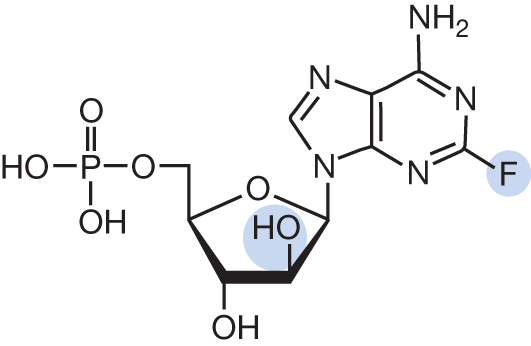
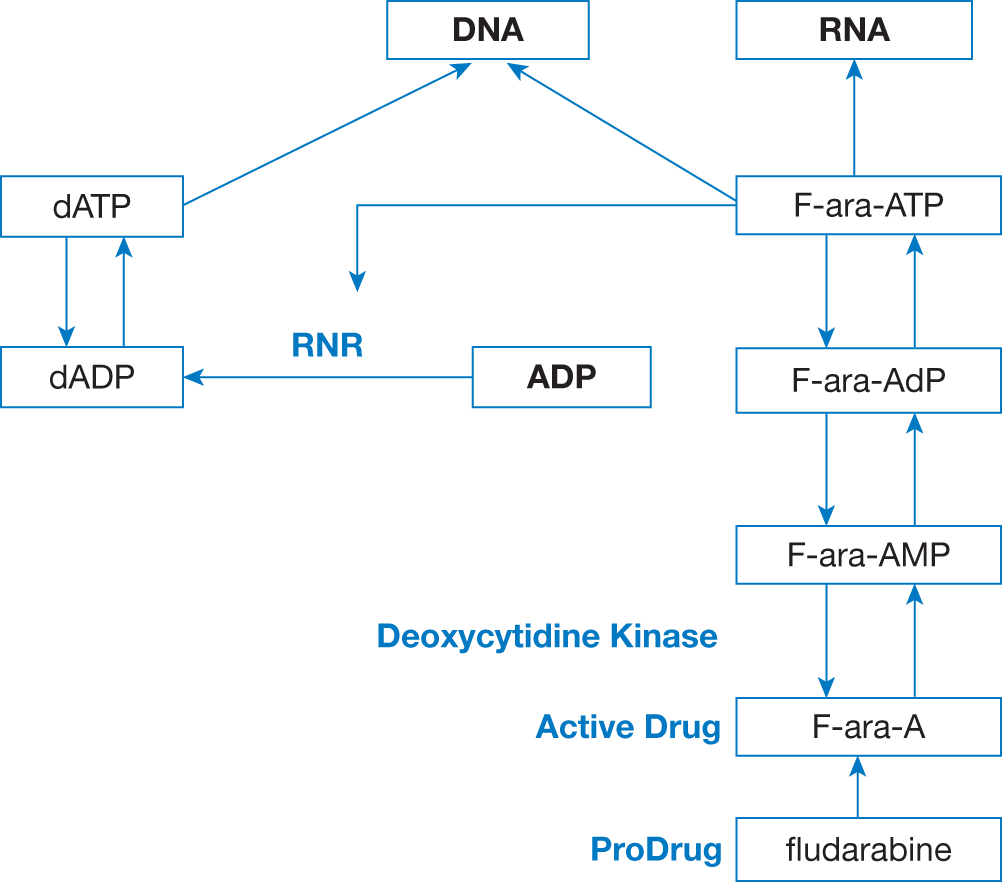
Fludarabine is rapidly dephosphorylated in plasma and enters tumor cells, where it is phosphorylated by deoxycytidine kinase to its active form. Fludarabine mimics adenosine and works in the following ways:
- incorporated into DNA to cause DNA strand breaks
- inhibits DNA polymerase
- inhibits ribonucleotide reductase (RNR targets M1 subunit)
- inhibits DNA primase and ligase I
- effective DNA chain terminator at 3’-end of DNA
| - Adverse events include:
- myelosuppression (mainly lymphopenia), PCP prophylaxis until CD4 count >200 cell/μL
- dose-dependent neurotoxicity
- hepatotoxicity (elevated transaminases)
- rash
- Oral fludarabine has similar toxicities as IV but greater frequency of diarrhea
- Infusion of fludarabine before ara-C augments the rate of ara-CTP synthesis in circulating AML blasts during therapy
|
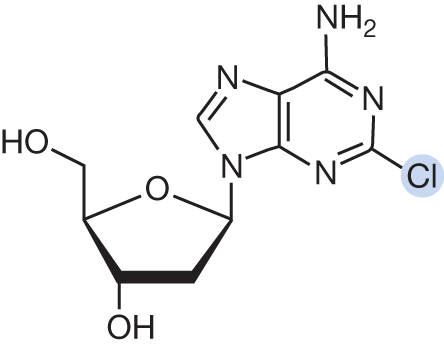
Cladribine
- AML (e.g., cladribine, cytarabine, and filgrastim with mitoxantrone [CLAG-M] or without mitoxantrone [CLAG])
- Hairy cell leukemia
- Langerhans cell histiocytosis
- Mantle cell lymphoma
- ALL (in children)
- AML
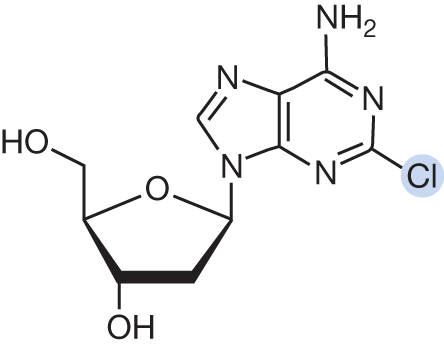
| Cladribine is a prodrug that requires intracellular phosphorylation by deoxycytidine kinase for activation. Cladribine mimics adenosine and works in the following ways:
- incorporated into DNA to cause DNA strand breaks
- inhibits DNA polymerase
- inhibits ribonucleotide reductase (RNR M1 subunit)
- triggers apoptosis in nondividing cells
- hypomethylating properties by inhibition of methyl group transfer of S-adenosyl methionine
| - Cladribine is 50% renally cleared. Requires dose reduction in renal impairment
- Adverse events include:
- myelosuppression (prolonged neutropenia), PCP prophylaxis until CD4 count >200 cell/μL
- crosses the blood–brain barrier, dose-dependent neurotoxicity
- nephrotoxicity
- fever and rash
- Start ara-C 2 hours after cladribine completion
|
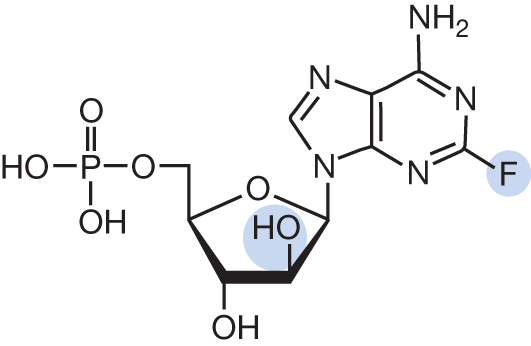
Clofarabine
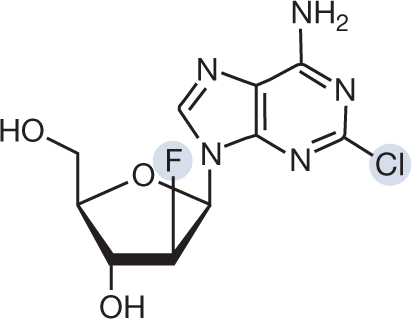
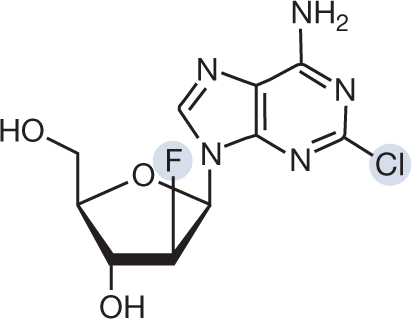
| Clofarabine is intracellularly phosphorylated by deoxycytidine kinase for activation. It is a second-generation purine analog that is designed to be resistant to adenosine deaminase. Clofarabine mimics adenosine and works in the following ways:
- incorporated into DNA to cause DNA strand breaks
- inhibits DNA polymerase
- inhibits ribonucleotide reductase (RNR M1 subunit)
- induces cellular apoptosis via induction of mitochondrial damage
- at low doses, it has hypomethylating activity
| - Adverse events include:
- myelosuppression, PCP prophylaxis until CD4 count >200 cell/μL
- hepatotoxicity (elevated transaminases)
- rash
- hypotension
- capillary leak syndrome/cytokine release (presents with tachypnea, tachycardia, pulmonary edema, hypotension). Consider prophylactic steroids for prevention.
- Increases intracellular concentrations of cytarabine to potentiate cytarabine cytotoxicity
|
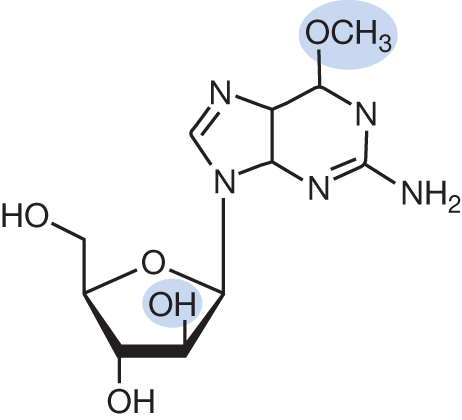
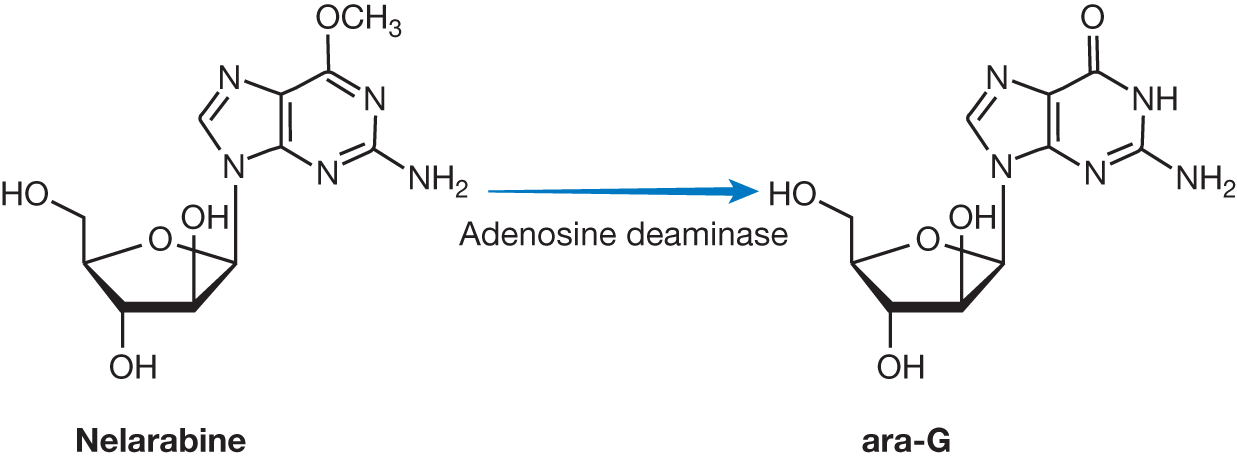
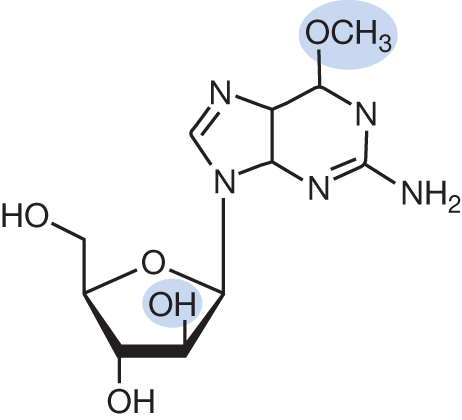
Nelarabine
| 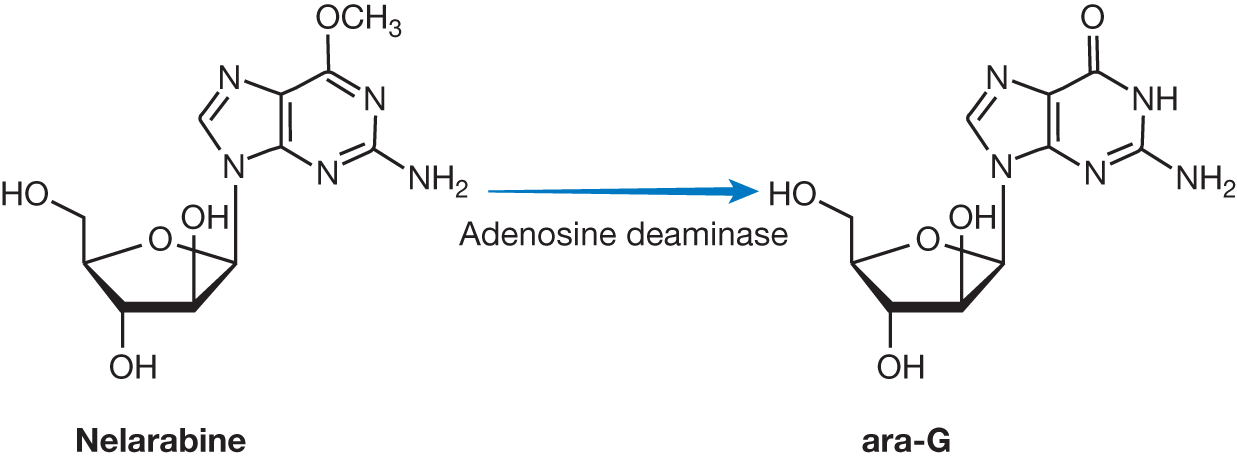
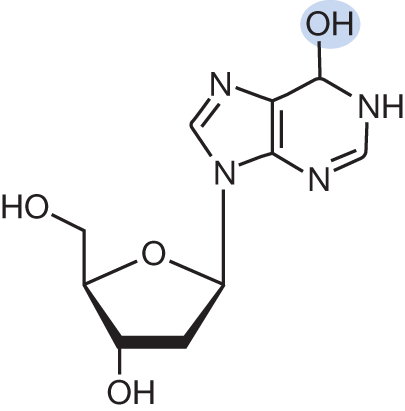
Nelarabine is a prodrug that is demethylated by adenosine deaminase (ADA) to guanine arabinoside (ara-G), which accumulates in higher concentrations in T-cells compared to B-cells. Intracellularly, similar to other purine and pyrimidine antimetabolites, ara-G is phosphorylated ultimately to ara-GTP. Nelarabine mimics guanosine and works in the following ways:
- incorporated into DNA to inhibit DNA primer extension
- inhibits RNR
| - Adverse events include:
- myelosuppression
- hepatotoxicity (elevated transaminases)
- fever
- Dose-limiting toxicity: CNS toxicities. Must monitor for neurologic toxicities such as altered mental status, somnolence, convulsions, peripheral neuropathy (numbness, paresthesias, motor weakness)
|
Pentostatin
- CLL
- Hairy cell leukemia
- Primary cutaneous lymphoma
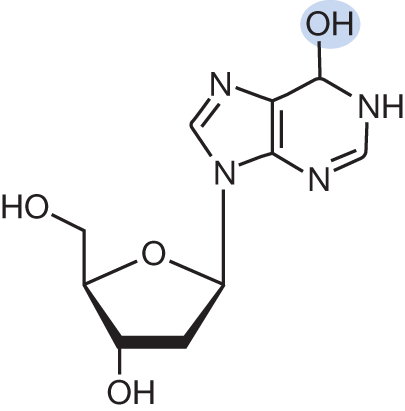
| Pentostatin mimics adenosine and is a potent inhibitor of ADA with subsequent accumulation of dATP, which causes:
inhibition of RNR resulting in decreased formation of other deoxyribonucleotides such as dCTP and dGTP to slow DNA synthesis and alter DNA replication and repair inhibition of adenosyl homocysteine hydrolase, resulting in decreased fall in cellular S-adenosyl methionine preventing cellular methylation reactions needed for cell proliferation
| - In general is well-tolerated
- Crosses cerebrospinal fluid (CSF) and may cause CNS toxicity
- Adverse events include:
- myelosuppression
- hepatotoxicity (elevated transaminases)
- nausea
- renal toxicity; primarily renally eliminated (40%–80%) and requires dose reduction in renal impairment
- cumulative pulmonary toxicity for patients exposed to fludarabine
|