D.1. A pericardial drain is placed following mediastinal decompression. How should this drainage tube be managed?
Answer:
Following open surgical drainage, a pericardial drain is connected to a closed, underwater seal system to prevent air entry into the mediastinum during negative pressure inspiration. Low-pressure suction (-15 to -25 cm H2O) is typically applied to facilitate clearance of effusions and air, but clots can still form within the tubing leading to a recurrence of cardiac tamponade if not cleared. Although a small respiratory "swing" might be present in drain tubing fluid or the water seal, "bubbling" is not typical unless there is a concurrent pneumomediastinum or a pneumothorax in direct connection to the drain. For percutaneous drainage, a pigtail catheter is typically connected to a closed drainage system for gravity drainage with a stopcock for aspiration and flushing to maintain catheter patency. Some percutaneous drain care protocols advocate regular aspiration every 4 to 6 hours with instillation of heparinized saline after each aspiration attempt. Regardless of the type of drainage tube, all patients should be monitored closely for re-accumulation of pericardial fluid from catheter malfunction. The dwell time for the catheter should be minimized to prevent infection. Drains are typically removed when there is less than 30 to 50 mL drainage over a 24-hour period, or after 24 to 72 hours (Figure 12.11).
Figure 12.11.: Basic Three-Bottle Suction Drainage System Diagram.
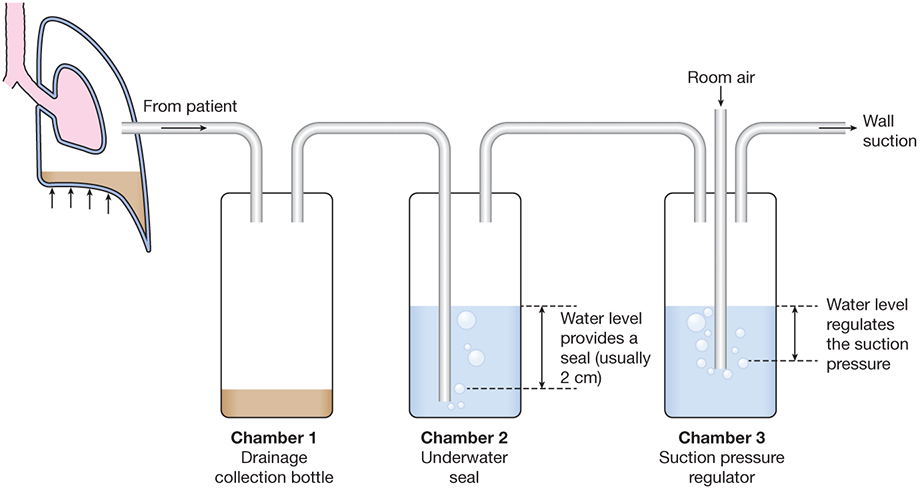
Basic three-bottle suction drainage system diagram. First bottle: drainage bottle; second bottle: water seal bottle; third bottle: negative pressure regulator bottle.
References
- De Carlini CC, Maggiolini S. Pericardiocentesis in cardiac tamponade: indications and practical aspects. e-J Cardiol Pract. 2017;15.
- Zisis C, Tsirgogianni T, Lazaridis G, et al. Chest drainage systems in use. Ann Transl Med. 2015;3:43.


