A.10. What are the echocardiographic and cardiac catheterization criteria for the four valvular lesions?
Answer:
The TEE severity scales of the various valvular lesions are summarized in Table 7.1.
Table 7.1: Transesophageal Echocardiography Severity Scales of Valvular Lesions
| Measurement | Severity | |||
|---|---|---|---|---|
| Normal | Mild | Moderate | Severe | |
| Mitral stenosis | ||||
| MVA (cm2) | 4.0-6.0 | >1.5 | 1.0-1.5 | <1.0 |
| Mean pressure gradient (mm Hg) | <2.0 | <5.0 | 5.0-10.0 | >10.0 |
| Aortic stenosis | ||||
| AVA (cm2) | 2.5-3.5 | >1.5 | 1.0-1.5 | <1.0 |
| Mean pressure gradient (mm Hg) | <5 | <20 | 20-40 | >40 |
| Mitral regurgitation | ||||
| Jet area/LA area | 0 | <20% | 20%-40% | >40% |
| Jet area (cm2) | 0 | <4.0 | 4.0-10.0 | >10.0 |
| Pulmonary vein Doppler | S wave > D wave | S > D | S < D | Systolic flow reversal |
| Aortic insufficiency | ||||
| Jet width/LVOT width | 0 | <25% | 25%-60% | >60% |
Aortic Stenosis
Echocardiographic criteria for AS include 2D or 3D imaging demonstrating limited AV cusp motion, a small orifice, and left ventricular concentric hypertrophy (Figure 7.16; Video 7.1). Doppler examination reveals a turbulent, high-velocity jet across the AV, and color flow Doppler demonstrates a turbulent, mosaic-appearing color map. The gradient across the AV measured at cardiac catheterization is different from that measured by echocardiography as discussed previously. Quantification of the Doppler-derived AS pressure gradient relies on the modified Bernoulli equation.
Figure 7.16.: Transesophageal Echocardiographic Findings of Moderate Aortic Stenosis (Midesophageal Aortic Valve [av] Short-Axis View [left] and Long-Axis View [right]).
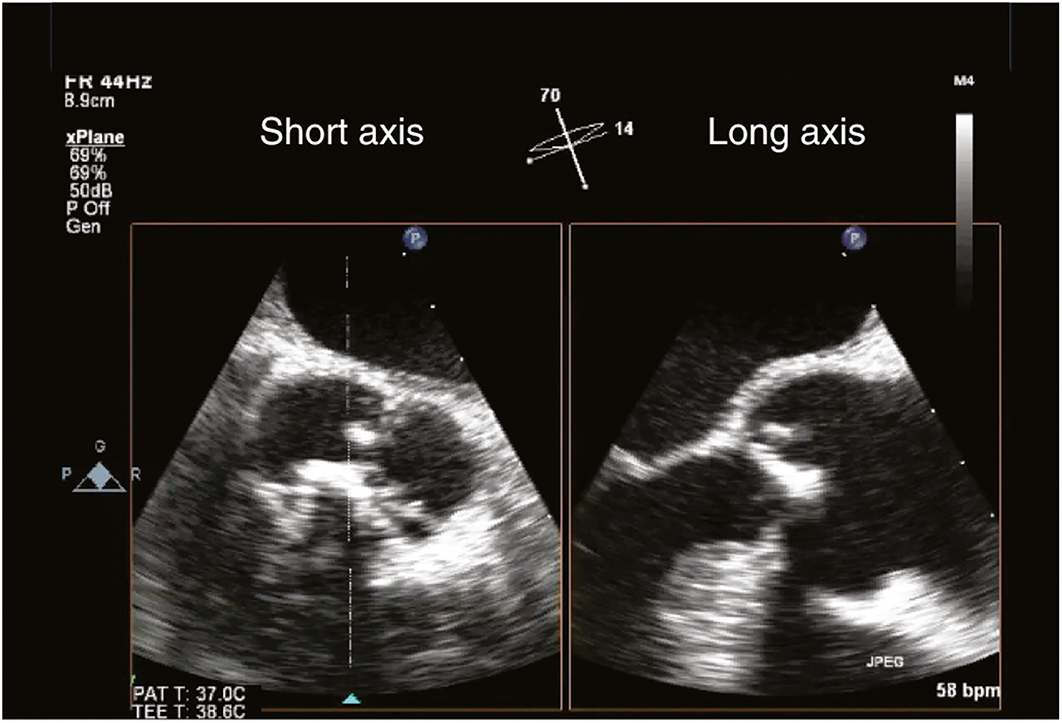
Transesophageal echocardiographic findings of moderate aortic stenosis (midesophageal aortic valve [AV] short-axis view [left] and long-axis view [right]). The AV cusps are calcified and demonstrate limited systolic excursion.
Pressure gradient (mm Hg) = 4 (transaortic valve velocity, m/s)2
Because flow is an important determinant of pressure gradients, both catheterization and Doppler-derived values must be interpreted along with cardiac output. Calculations permit determination of a valve area. Severe AS is present when the mean pressure gradient exceeds 40 mm Hg or the valve area is less than 1.0 cm2.
Aortic Insufficiency
Catheterization criteria for AI rely on the qualitative estimation of the regurgitation volume and estimation of left ventricular size and ejection fraction. Similar quantification can be made from Doppler color echocardiography-derived data. The width of the regurgitant jet at the level of the AV can be compared to the width of the LVOT. A ratio of more than 0.6 corresponds to severe AI (Figure 7.17; Video 7.2). Another sign of severe AI is diastolic flow reversal of the descending thoracic aorta, as observed on spectral Doppler.
Mitral Stenosis
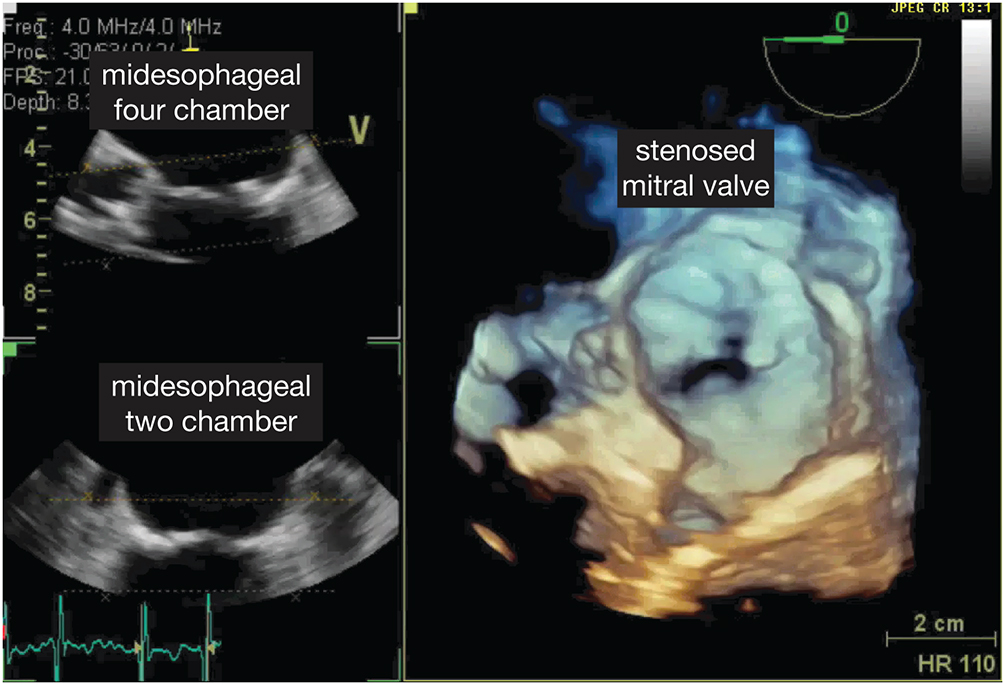
The severity of MS can be obtained by direct measurement of the diastolic gradient between the LA and ventricle at the time of cardiac catheterization. This requires a transatrial puncture, a procedure largely replaced by echocardiographic techniques. Echocardiographic diagnosis is based on gradient estimation by Doppler and by measuring the rate of decay in the pressure with the time spent in diastole (pressure halftime). The MV area (cm2) can be derived from an empirical formula wherein the MV area equals 220 divided by this pressure halftime. Severe MS is present when the mean diastolic gradient exceeds 10 mm Hg, corresponding to a valve area of less than 1.0 cm2 (Figure 7.18; Video 7.3).
Mitral Regurgitation
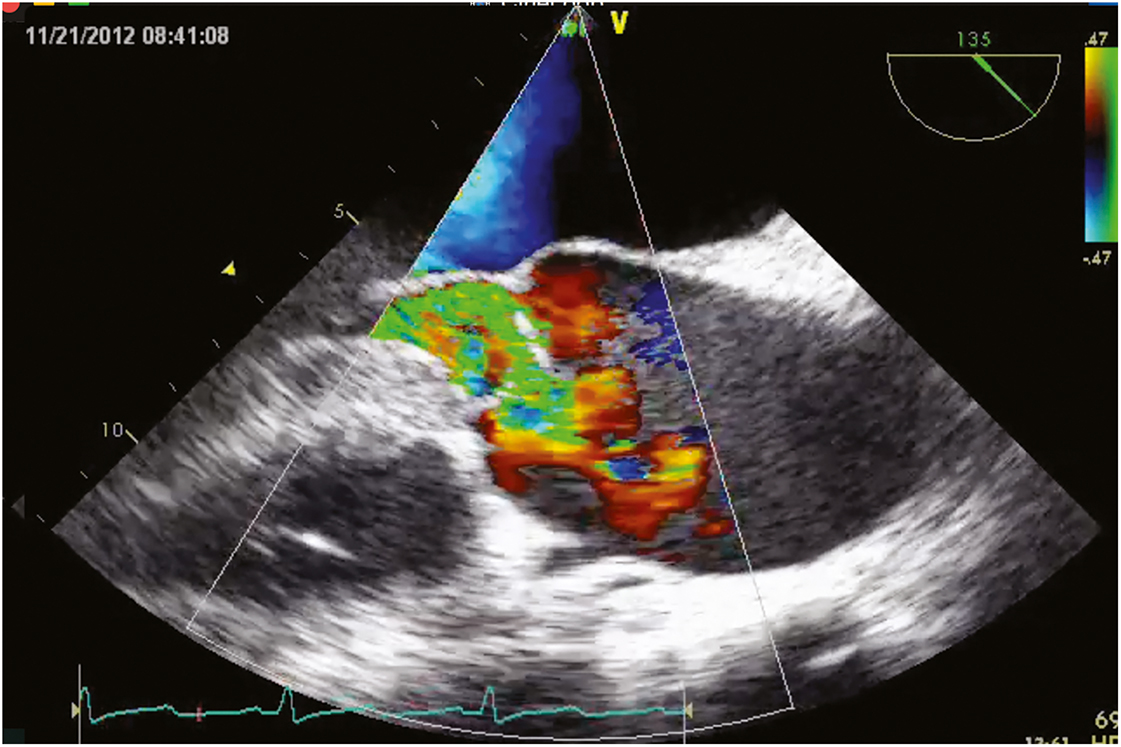
In the presence of MR, ventriculography demonstrates reflux of dye from the LV into the LA. Severe MR is diagnosed according to the relative volume of regurgitant flow and flow reversal in the pulmonary veins. Color Doppler echocardiography permits similar quantification, as does spectral Doppler waveforms of pulmonary venous flow (Figure 7.19; Video 7.4).
Figure 7.19.: Transesophageal Echocardiographic Findings of Moderate Mitral Stenosis (Color Flow Doppler) with 3D View (Top) and 2d View (Bottom).
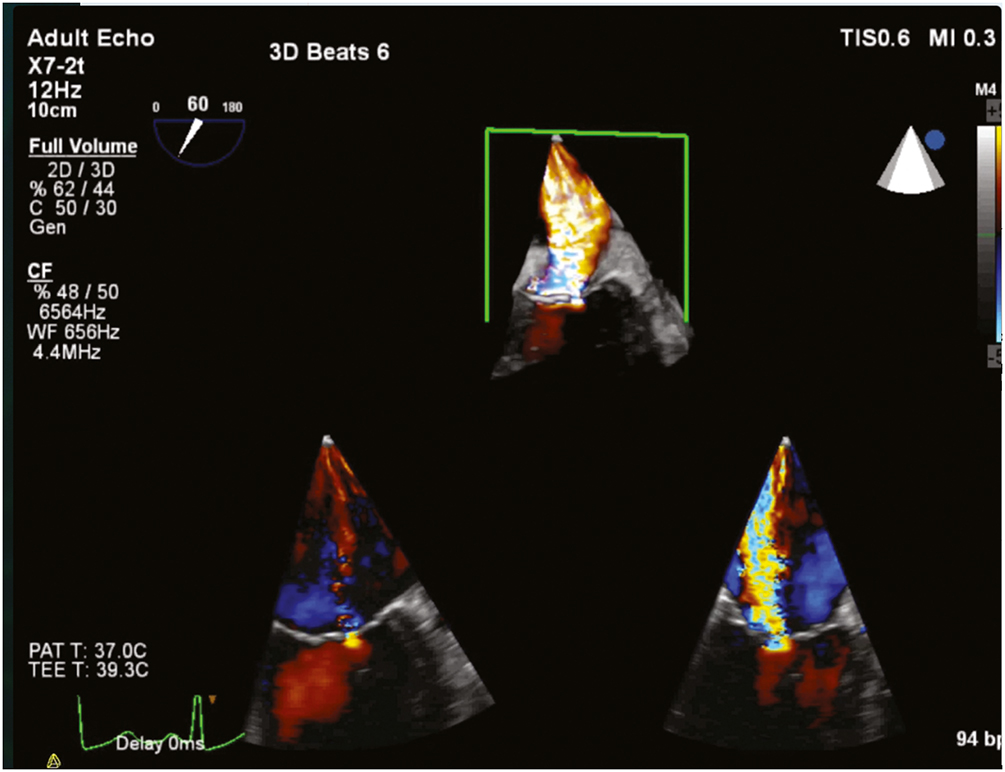
Transesophageal echocardiographic findings of moderate mitral stenosis (color flow Doppler) with 3D view (top) and 2D view (bottom).
Color Doppler echocardiography is often useful in identifying the cause of the valvular lesion, its extent of involvement within and around the valve, and the associated hemodynamic changes. It is sufficient for diagnosing and grading most valvular lesions. Catheterization, however, is often performed to assess the presence of concomitant coronary artery disease, especially in patients of advanced age. Notably, diagnoses of prosthetic valve stenosis are made according to device-specific thresholds supplied by the manufacturer.
References
- Baumgartner H, Hung J, Bermejo J, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017;30:372-392.
- Otto CM. Valvular stenosis and valvular regurgitation. In: Otto CM, ed. Textbook of Clinical Echocardiography. 6th ed. Elsevier; 2018:288-369.
- Pandian NG, Kim JK, Arias-Godinez JA, et al. Recommendations for the use of echocardiography in the evaluation of rheumatic heart disease: a report from the American Society of Echocardiography. J Am Soc Echocardiogr. 2023;36:3-28.
- Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30:303-371.