B.2. How would you optimize this patient's cardiovascular status before definitive diagnosis and treatment?
Answer:
The key resuscitation goals before definitive management are:
Optimize CO (which is determined by HR and SV), and
Maintain adequate perfusion pressure to critical organs (ie, heart, brain, kidneys).
Broadly, the hemodynamic goals for this patient are "full, tight and fast." This patient requires SV correction to increase CO; however, without a clear etiology for her low CO state, this should be approached cautiously. This high CVP is due to either cardiac tamponade or RV dysfunction; the effect of aggressive volume administration can either improve SV or precipitate RV failure because both conditions exist on different points of the Frank-Starling curve (Figure 12.6).
Figure 12.6.: Predicted Response to Volume Challenge in Cardiac Tamponade Compared with Right Ventricular (RV) Dysfunction.
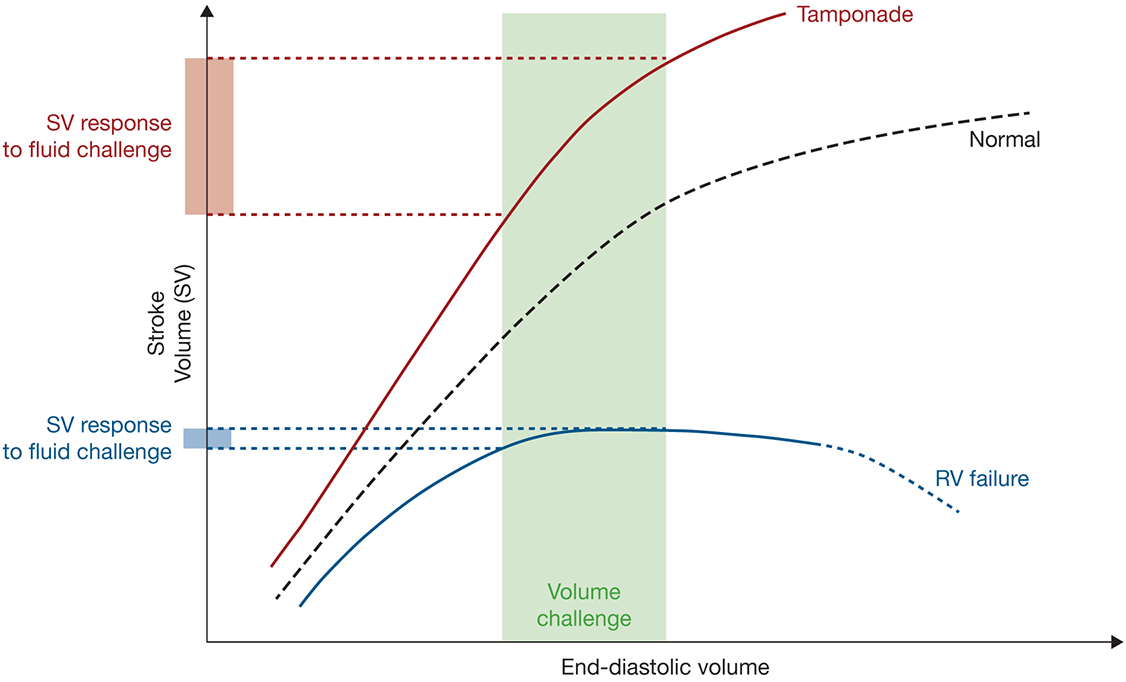
Predicted response to volume challenge in cardiac tamponade compared with right ventricular (RV) dysfunction. This figure shows two different Frank-Starling curves referenced to a hypothetical normal curve. In cardiac tamponade, the right ventricle is underfilled and hyperdynamic. This is in contrast to the curve in RV dysfunction, where the decreased slope and early plateau reflects its depressed inotropic state. Applying the same volume to these two models leads to a large SV response in cardiac tamponade, but a minimal change in RV dysfunction, and, in this example, pushes the right ventricle into failure.
The distinction between cardiac tamponade from RV failure can be made with echocardiography to immediately and safely administer volume to maintain adequate cardiac preload.
A vasoconstrictor or a positive inotrope with vasoconstrictor properties should be initiated to maintain afterload (Figure 12.6). The choice of vasoactive agent should take into account the patient's clinical trajectory as well. Norepinephrine and epinephrine are titratable, maintain or increase HR and have short half-lives. Dopamine, however, is associated with severe arrhythmias and increased mortality when used in cardiogenic shock at higher doses (>2 µg/kg/min). The inodilators dobutamine and milrinone decrease SVR and PVR and can improve myocardial performance in a failing ventricle, but can also compromise organ perfusion. Titrating norepinephrine infusion (0.05-0.5 µg/kg/min) or low-dose infusion of epinephrine (0.02-0.05 µg/kg/min) might confer the greatest benefit, while minimizing unexpected afterload reduction and dose-related tachyarrhythmia from dobutamine.
Together with preload optimization, a systemic mean arterial pressure (MAP) of at least 60 to 65 mm Hg should be targeted to maintain adequate cerebral and renal perfusion. Myocardial perfusion in this patient is compromised due to depressed coronary blood flow, preexisting tachycardia, and potential cardiac tamponade. Any attempts to lower HR in an effort to reduce myocardial oxygen demand without correcting preload will risk a further decline in CO that will correspondingly lower all organ blood flow, including the heart.
References
- Carmona P, Mateo E, Casanovas I, et al. Management of cardiac tamponade after cardiac surgery. J Cardiothorac Vasc Anesth. 2012;26:302-311.
- De Backer D, Biston P, Devriendt J, et al. Comparison of dopamine and norepinephrine in the treatment of shock. New Engl J Med. 2010;362:779-789.
- Grocott HP, Gulati H, Sadeesh S, Mackensen, GB. Anesthesia and the patient with pericardial disease. Can J Anaesth. 2011; 58:952-966.
- Kline JA, Hall CL, Jones AE, et al. Randomized trial of inhaled nitric oxide to treat acute pulmonary embolism: the iNOPE trial. Am Heart J. 2017;186:100-110.


