A.7. How are thoracic aortic dissections classified?
Answer:
The most commonly used systems to classify aortic dissections focus on anatomic detail while others additionally consider whether malperfusion and associated symptoms are present (Figure 9.8).
Figure 9.8.: A. The Stanford and Debakey Classifications of Aortic Dissections.
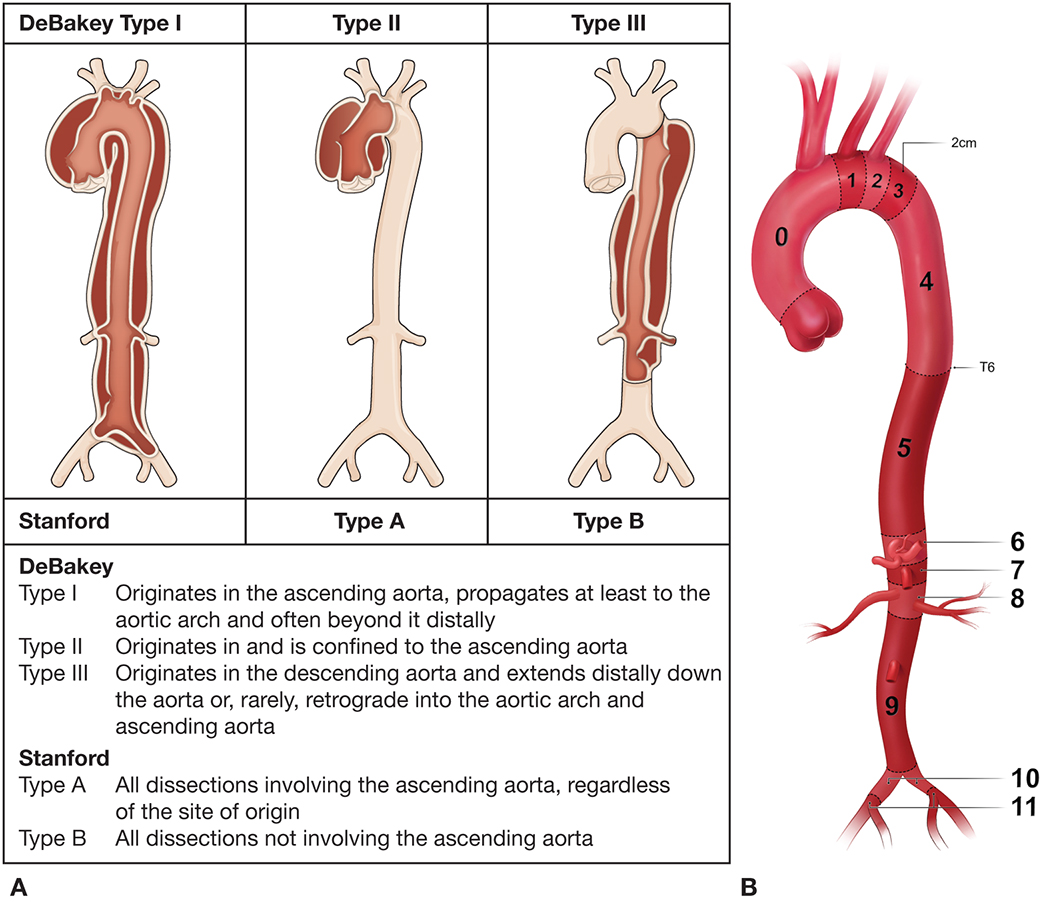
A. The Stanford and DeBakey classifications of aortic dissections. (Reprinted with permission from Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: part I: from etiology to diagnostic strategies. Circulation. 2003;108:628-635.) B. Classification of Aortic Anatomic Segments by 11 Landing Zones. Zone 0 (involves the ascending to the distal end of the origin of the innominate artery); Zone 1 (involves the origin of the left common carotid; between the innominate and the left carotid); Zone 2 (involves the origin of the left subclavian; between the left carotid and the left subclavian); Zone 3 (involves the proximal descending thoracic aorta down to the T4 vertebral body; the first 2 cm distal to the left subclavian); Zone 4 (the end of zone 3 to the mid-descending aorta—T6); Zone 5 (the mid-descending aorta to the celiac); Zone 6 (involves the origin of the celiac; the celiac to the superior mesenteric); Zone 7 (involves the origin of the SMA; the superior mesenteric to the renals); Zone 8 (involves the origin of the renal arteries; the renal to the infrarenal abdominal aorta); Zone 9 (the infrarenal abdominal aorta to the level of aortic bifurcation ); Zone 10 (the common iliac); Zone 11 (involves the origin of the external iliac arteries). (From Czerny M, Schmidli J, Adler S, et al. Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: an expert consensus document of the European Association for Cardio-Thoracic surgery [EACTS] and the European Society for Vascular Surgery [ESVS]. Eur J Cardiothorac Surg. 2019;55:133-162 by permission of Oxford University.)
DeBakey Classification
The DeBakey system categorizes dissections based on the origin of the intimal tear and the degree of distal extension. Type I and type II dissections are almost always treated surgically, while type III dissections are often managed medically.
Type I: Dissection tear originates in the ascending aorta and propagates distally to include the aortic arch and typically the descending aorta.
Type II: Dissection tear is confined only to the ascending aorta.
Type III: Dissection tear originates in the descending thoracic aorta and propagates most often distally.
Stanford Classification
The Stanford classification system is simpler and divides dissections according to whether the ascending aorta is involved or not, irrespective of the site of origin. It highlights the need for surgical repair to improve survival in the setting of Stanford type A dissections, in contrast to Stanford type B dissections that demonstrate survival benefit in response to medical therapy.
Society for Vascular Surgery/Society of Thoracic Surgeons (SVS/STS) Classification
The DeBakey and Stanford criteria are limited by their inability to classify dissections originating in the aortic arch. Thus, after the introduction of a third category of non-A-non-B dissections for proximal dissection flaps that begin in the aortic arch, the SVS and STS introduced a new classification scheme in 2020 that subdivides aortic anatomy into 11 zones to allow for more granular reporting of aortic dissections.
AD denotes a type A dissection with an entry tear in zone 0 and extends distally to the zone designated by the subscript D (0-11).
BPD indicates a type B dissection with an entry tear in zone 1 or beyond with the proximal and distal extents of the dissection denoted by subscripts P and D, respectively.
ID indicates a dissection that begins in zone 0 but has an unidentified entry tear with the distal extent denoted by the subscript D.
Penn Classification of Malperfusion Syndromes
The Penn classification system was developed to better predict perioperative mortality among patients with acute Stanford type A dissections subcategorized according to ischemic symptoms from malperfusion on presentation.
Class Aa patients are hemodynamically stable and present without ischemia, branch vessel malperfusion, or circulatory collapse.
Class Ab patients present with branch vessel malperfusion that manifests as stroke, paraplegia, renal dysfunction, mesenteric malperfusion, or ischemic extremities.
Class Ac patients experience circulatory collapse with or without cardiac involvement, such as cardiac tamponade, coronary dissection, myocardial infarction, new-onset left or right ventricular dysfunction, AR, or aortic rupture.
Class Abc patients present with local ischemia from branch vessel malperfusion and generalized ischemia from circulatory collapse.
Prognosis is best for class Aa patients with a hospital mortality of only 3.1% and worst for class Abc patients with a hospital mortality of 40%. Class Ab and Ac patients had similar intermediate hospital mortalities (25.6% and 17.6%, respectively). The Penn classification system for predicting perioperative mortality may also be applicable to patients with type B dissections who undergo surgical or medical management.
Classification Based on Malperfusion Syndromes
Due to the substantial effects of malperfusion syndromes on patient outcomes, new classification systems have been proposed that integrate clinical evidence with symptoms and etiologies of malperfusion syndromes into the therapeutic approach for types A, B, non-A-non-B dissections. These systems may lead to a push for earlier, more aggressive open surgical or endovascular procedural management. The introduction of the first web-based score that predicts 30-day mortality in acute TAAD appears to be promising and can help refine disease process-oriented treatment strategies for patients.
Aortic dissections were historically regarded as acute or chronic if they occurred within or beyond 2 weeks of symptom onset, respectively. More recently, the SVS and STS proposed a contemporary temporal classification system to guide prognostication and clinical decision-making about interventions. This classification system is subdivided into four temporal types: hyperacute (<24 hours), acute (1-14 days), subacute (15-90 days), and chronic (>90 days).
References
- Augoustides JG, Geirsson A, Szeto WY, et al. Observational study of mortality risk stratification by ischemic presentation in patients with acute type A aortic dissection: the Penn classification. Nat Clin Pract Cardiovasc Med. 2009;6:140-146.
- Czerny M, Rylski B. Acute type A aortic dissection reconsidered: it's all about the location of the primary entry tear and the presence or absence of malperfusion. Eur Heart J. 282021;43:53-55.
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897-903.
- Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al; Peer Review Committee Members. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on clinical practice guidelines. Circulation. 2022;146:e334-e482.
- Tien M, Ku A, Martinez-Acero N, Zvara J, Sun EC, Cheung AT. The Penn Classification predicts hospital mortality in acute Stanford type A and type B aortic dissections. J Cardiothorac Vasc Anesth. 2020;34:867-873.


