A.1. What is thoracic aortic aneurysm (TAA)? How does it typically present? How is it diagnosed?
Answer:
Thoracic Aortic Aneurysm
An arterial aneurysm is an abnormal dilation of all three layers of an artery, that is, the intima, media, and adventitia, to at least 1.5 times its expected normal diameter by convention. This definition is typically applicable to the descending thoracic and thoracoabdominal aorta, while the thresholds for aortic root and ascending thoracic aorta aneurysms vary according to the presence of associated conditions. While 60% of TAAs involve the aortic root and/or ascending aorta, 40% involve the descending aorta, 10% involve the arch, and 10% involve the thoracoabdominal aorta. The dimensions that define normal aortic size are determined by the patient's age, sex, and body surface area.
A challenge in the care of patients with thoracic aortic disease is identifying them prior to the onset of a catastrophic aortic event. Despite their propensity for life-threatening complications, TAAs are often clinically silent and diagnosed during imaging for an unrelated disorder or as part of dedicated screening for those at risk. When symptoms do occur, they are often nonspecific, and diagnosis requires a high index of clinical suspicion. Symptoms of TAAs frequently result from compression of adjacent structures. Patients may exhibit hoarseness from recurrent laryngeal nerve compression, stridor from bronchial or tracheal compression, dyspnea from lung compression, dysphagia from esophageal compression, and/or facial edema from superior vena cava (SVC) compression. Pain in the neck, jaw, back, shoulders, or abdomen can also be present. Additionally, new-onset heart failure symptoms may occur as aortic enlargement, which results in progressive AI (Figure 9.1).
Figure 9.1.: Midesophageal Aortic Valve Long-Axis View on Transesophageal Echocardiography Demonstrating Moderate Central Aortic Insufficiency Secondary to Aortic Root and Ascending Aortic Dilatation in a Young Female with Turner Syndrome.
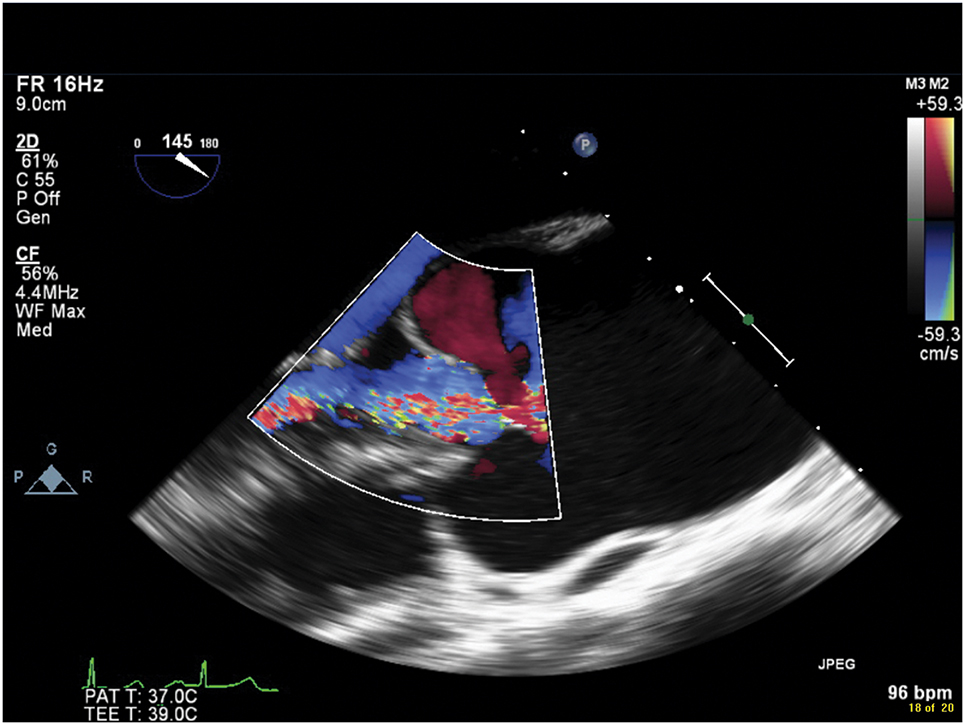
Midesophageal aortic valve long-axis view on transesophageal echocardiography demonstrating moderate central aortic insufficiency secondary to aortic root and ascending aortic dilatation in a young female with Turner syndrome.
CT angiography (Figure 9.2) is the first-line imaging modality that can provide accurate measurement of the maximal diameter of the aneurysm, delineate the extent of the aneurysm, and detect branch vessel involvement and acute aortic syndromes (AASs), such as aortic dissection, intramural hematoma (IMH), or penetrating aortic ulcer. Magnetic resonance angiography (MRA) also provides high-resolution three-dimensional aortic assessment but is considered a second-line modality due to longer scan times, higher costs, and limited availability. Transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) provide assessment of aortic pathology, valvular disease, and cardiac function; TEE has a limited role in the primary assessment of TAA unless concurrent structural cardiac disease or AASs are suspected (Figure 9.3).
Figure 9.2.: Three-Dimensional (3D) Compute Tomography Reconstruction Demonstrating a Thoracoabdominal Aneurysm that Begins in the Descending Thoracic Aorta and Extends to the Infrarenal Aorta, above the Bifurcation into the Iliac Arteries.
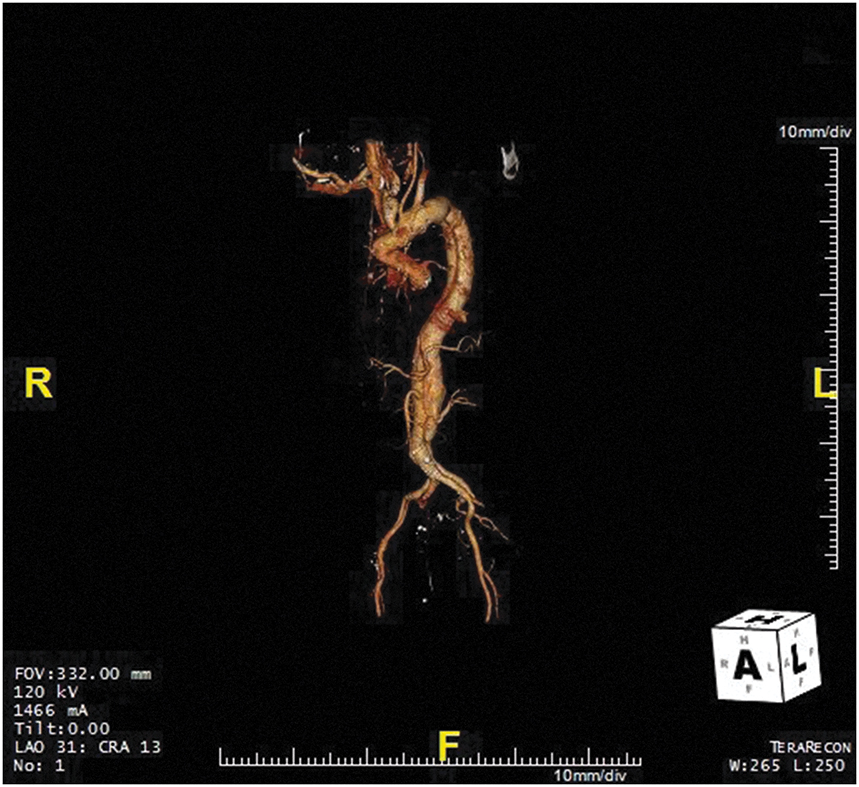
Three-dimensional (3D) compute tomography reconstruction demonstrating a thoracoabdominal aneurysm that begins in the descending thoracic aorta and extends to the infrarenal aorta, above the bifurcation into the iliac arteries. Also seen is a chronic type B aortic dissection.
Figure 9.3.: A. Midesophageal Aortic Valve Long-Axis View on Transesophageal Echocardiography Demonstrating the Aortic Valve Annulus, Sinus, and Sinotubular Junction Dimensions at Mid-Systole.
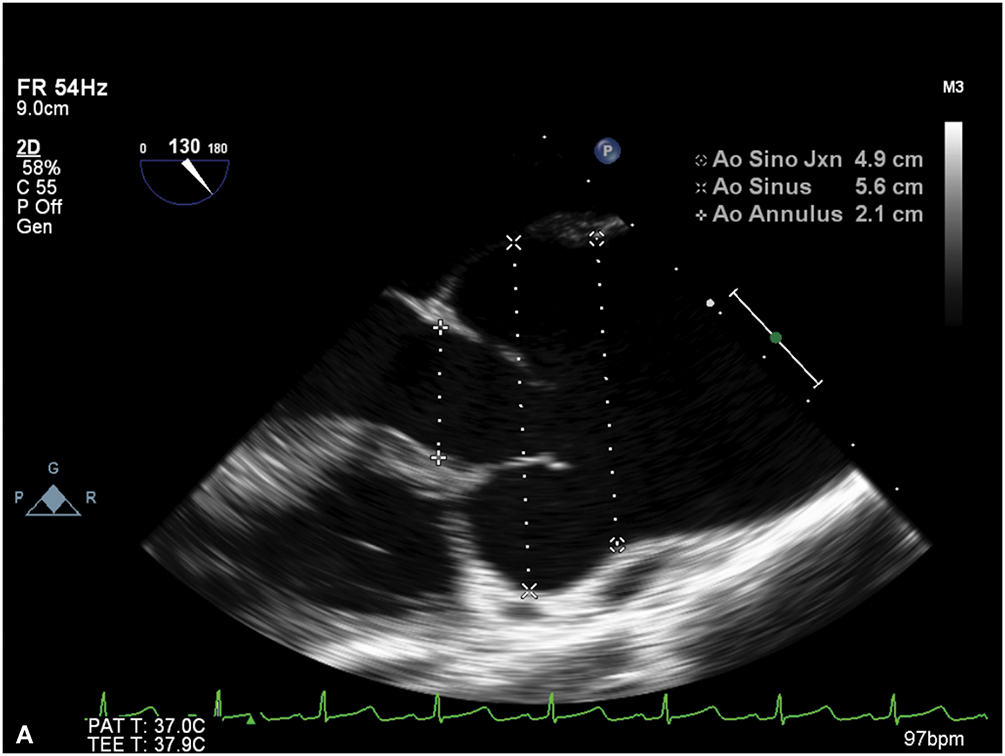
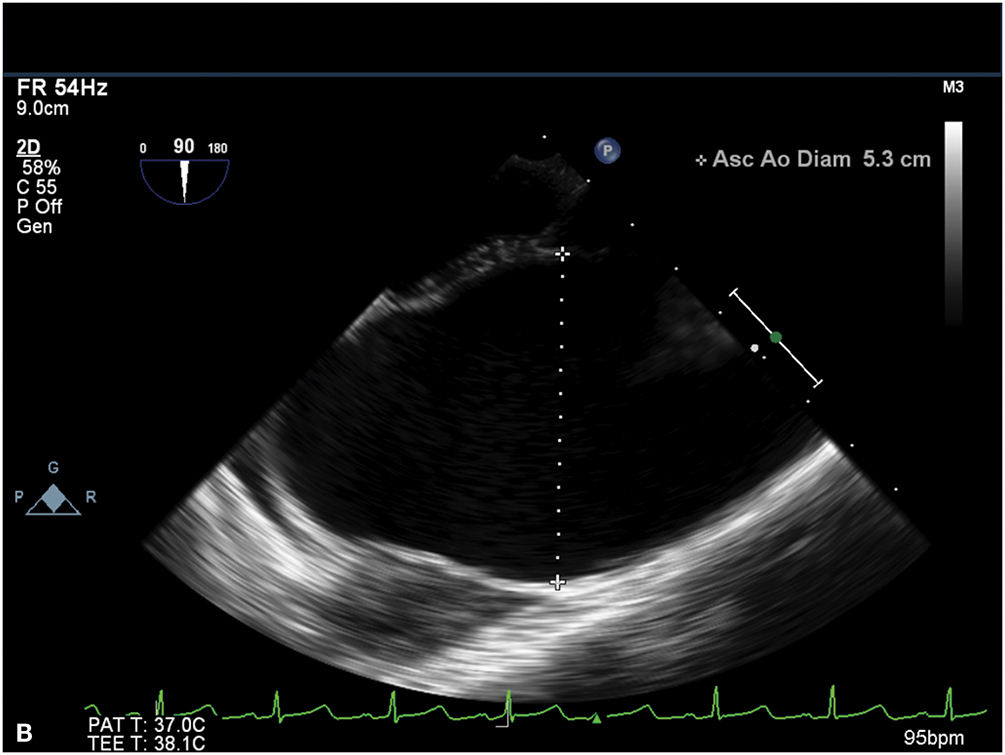
A. Midesophageal aortic valve long-axis view on transesophageal echocardiography demonstrating the aortic valve annulus, sinus, and sinotubular junction dimensions at mid-systole. B. Ascending aorta in short axis demonstrating aneurysmal enlargement with a diameter of 5.3 cm in a young female with Turner syndrome.
References
- Isselbacher EM. Thoracic and abdominal aortic aneurysms. Circulation. 2005;111:816-828.
- Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al; Peer Review Committee Members. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on clinical practice guidelines. Circulation. 2022;146:e334-e482.
- Wang TKM, Desai MY. Thoracic aortic aneurysm: optimal surveillance and treatment. Cleve Clin J Med. 2020;87:557-568.

