Objectives ⬇
- Trace the evolution of nursing informatics from concept to specialty practice.
- Relate nursing informatics metastructures, concepts, and tools to the knowledge work of nursing.
- Explore the quest for consistent terminology in nursing, and describe terminology approaches that accurately capture and codify the contributions of nursing to health care.
- Explore informatics education initiatives.
- Explore how nurses can create and derive clinical knowledge from information systems.
Key Terms ⬆ ⬇
Introduction ⬆ ⬇
The information and knowledge that inform 21st-century healthcare delivery have been growing at an unprecedented pace in recent years. Clinical research has propelled the understanding of the efficacy of various clinical practices, treatment regimens, and interventions. Extended and expanded access to clinical research findings and decision support tools has been significantly influenced by the advent of computerization and the internet. Indeed, the conduct of research itself has been accelerated by virtue of ubiquitous computing. Working in environments of increasingly complex clinical care and contending with the management of large volumes of data and information, all nurses need to avail themselves of the technological tools that can support quality practice that is optimally safe, informed, and knowledge based. Although the increased deployment of information technology (IT) within healthcare settings presumes that nurses and other health professionals are proficient in the use of computing devices, the processes and potential outcomes associated with informatics are yet to be fully realized or understood. Nurses need to participate in the creation of those possibilities.
Health service organizations, societies, and governments throughout the industrialized world are committed to ensuring that healthcare delivery is safe, knowledge based, cost-effective, seamless, and timely. Beyond these deliverables, there are expectations of improved efficiency and quality and of the active engagement of consumers in their care. Given the evolving emphasis on such issues as chronic disease management and aging at home, informatics tools need to include the use of technologies to empower citizens to manage their own health and wellness more effectively.
This chapter explores the history and evolution of nursing informatics (NI) and informatics education and defines and addresses the goal of informatics as it relates to nursing practice. The ways in which NI supports the creation of a culture of knowledge-based nursing practice that is enabled and advanced using information and communication technologies are described. The chapter also addresses some of the challenges associated with the attainment of this knowledge-based culture as well as the opportunities for nurses to create and derive knowledge from emerging health IT. Finally, the chapter provides a contemplative view of the future for nurses and informatics.
The Evolution of a Specialty ⬆ ⬇
Nurses have historically gathered and recorded data, albeit in a paper record. For example, nurses gather atomic-level data (e.g., blood pressure, pulse, blood glucose, and pallor), aggregate data to derive information (e.g., impending shock), and apply knowledge (e.g., implement the evidence-based practice [EBP] protocol for impending shock). Over the years, these data have been recorded into individuals' hard copy health records, thereby chronicling findings, actions, and outcomes; these data and information were then forever lost, unless they were manually extracted for research purposes. As computers were introduced into health care and data and information were recorded electronically, a nursing specialty was born.
Florence Nightingale has been credited as one of the first statisticians to collect and use data to change the way she cared for her patients. While serving in the Crimean War, she began to gather data regarding the conditions in which patients were living and the diseases they contracted and from which they died. These data were later used to improve patient conditions at both city and military hospitals (O'Connor & Robertson, 2003). There is no doubt that nursing experiences build knowledge and skill in nursing practice but that paper-based documentation has hindered the ability to share knowledge and aggregate experiences to build new knowledge.
NI pioneers recognized early on that computers had the potential to fundamentally change health care, and they became actively involved in shaping how computers were used in health care. For more specific information on NI pioneers and to view video recordings of the contributions of each pioneer in the NI history project, please visit this website: https://amia.org/community/working-groups/nursing-informatics/nursing-informatics-innovators.
According to Ozbolt and Saba (2008), one very early pioneer, Harriet Werley, a nurse researcher at Walter Reed Army Research Institute, consulted with IBM in the late 1950s to explore computer use in health care. Ms. Werley recognized the need for a minimum set of data to be collected from every patient so that comparisons could be made, which set the stage for the development of informatics. As computers became more commonplace in the 1970s and 1980s, more nurses became involved with developing approaches to using computers in health care. It is important to note that this was also the time when nurse leaders were writing about the need for and developing terminologies to represent patient data and nursing contributions to health care, beginning to conduct informatics research, and advocating for informatics education in nursing curricula (Ozbolt & Saba, 2008).
In 1989, Graves and Corcoran offered what is widely viewed as the seminal definition of NI. They defined NI as “a combination of computer science, information science, and nursing science designed to assist in the management and processing of nursing data, information, and knowledge to support the practice of nursing and the delivery of nursing care” (p. 227). In this same article, acknowledging the 1986 work of Blum, Graves and Corcoran provided the definitions and descriptions of the concepts of data (i.e., discrete entities described objectively without interpretation), information (i.e., data that are interpreted, organized, or structured), and knowledge (i.e., information that is synthesized so that relationships are identified and formalized) as they apply to the science and practice of NI. They also described what is meant by management and processing:
The management component of informatics is the functional ability to collect, aggregate, organize, move, and re-present information in an economical, efficient way that is useful to the users of the system. . . . In practice, processing is considered as a transformation of data or information from one form to another form, usually at a more complex state of organization or meaning. There is a progression of transformation of data into information and of information into knowledge. (p. 227)
We will return to a discussion of these concepts later in the chapter. For now, we continue our exploration of the evolution of informatics as a specialty.
In the 1990s, an NI workgroup was established within the newly founded American Medical Informatics Association, the American Nurses Association (ANA) recognized NI as a specialty and published two documents related to informatics practice, and the first informatics certification was established (Ozbolt & Saba, 2008). As NI pioneers and emerging leaders continued to champion the use of computers in health care, the need for computer-friendly terminologies to represent the work of nursing was increasingly apparent. Several terminology schemes were developed during this time, and there were also international efforts at developing a standardized nursing terminology to capture and codify the contributions of nursing to health care. At the same time, healthcare organizations were beginning to implement electronic information systems. There was much work being done around computerization in health care, but there was little coordination of these efforts and approaches. Ozbolt and Saba (2008) explained that the cost of using known nomenclatures and the difficulty in choosing among them resulted in many healthcare organizations deciding to use their own or vendor-provided, nonstandard terms. Use of nonstandard terms creates issues with data retrieval and analysis. We will discuss this issue in more detail later in the chapter.
President George W. Bush's call for electronic health records (EHRs) in 2004 further stimulated the development of NI, informatics competency identification, and informatics education reform and spawned several national and international informatics organizations. Knowledge creation in nursing is dependent on knowledge representation in the information management tools that are central to NI, thus we see the clear connection between nursing science and NI. That is, knowledge creation in nursing is dependent on knowledge representation in the information management tools that are central to NI. As the NI pioneers recognized these important connections and synergies, both nursing as a science and NI as a specialty evolved. Indeed, the evolution is not complete.
As the NI specialty was evolving, informatics pioneers and other nurse leaders collaborated on several ANA publications. As mentioned previously, NI was identified by the ANA as a specialty in 1992. In 1994, the first formal document identifying the scope of practice was published, followed by a separate standards of practice document in 1995. In 2001, a combined scope and standards document was published by the ANA, followed by a more robust scope and standards publication in 2008. In 2015, the ANA released the second edition of Nursing Informatics: Scope and Standards of Practice, and in 2022, the third edition was released.
What Is Nursing Informatics? ⬆ ⬇
The definition of NI has undergone several revisions to arrive at its current form. The 1994 ANA definition of NI indicated that it was the integration of nursing science, computer science, and information science and that it supports practice, education, research, and knowledge development (Murphy, 2010). The 2001 version mentioned the support of decision-making by patients and providers across all roles and settings and identified information structures, processes, and IT as central to informatics (Murphy, 2010). An important change in the 2008 definition of NI is the addition of wisdom to the key concepts of the management of data, information, and knowledge (Murphy, 2010).
The ANA's Nursing Informatics: Scope and Standards of Practice (2015) offered the following definition of NI:
Nursing informatics (NI) is the specialty that integrates nursing science with multiple information and analytical sciences to identify, define, manage, and communicate data, information, knowledge, and wisdom in nursing practice. NI supports nurses, consumers, patients, the interprofessional healthcare team, and all other stakeholders in their decision-making in all roles and settings to achieve desired outcomes. This support is accomplished through the use of information structures, information processes, and information technology. (pp. 1-2)
In the 2015 version, we note that the sciences are no longer limited to nursing science, information science, and computer science. Cognitive science is also a very important part of NI. Other sciences that may contribute to NI include library science and information management, mathematics, archival science, and the science of terminologies and taxonomies (ANA, 2015).
Let us reflect more carefully on NI by deconstructing each of the statements contained in the ANA's (2015) definition (statements from the definition are italicized):
- Nursing informatics (NI) is the specialty that integrates nursing science with multiple information and analytical sciences to identify, define, manage, and communicate data, information, knowledge, and wisdom in nursing practice. As we established previously, there are concepts drawn from several sciences that are integrated to support and contribute to NI. The contributions of these sciences become apparent in the actions of NI: identify, define, manage, and communicate. The last part of this statement contains the critical central concepts of NI: the data, information, knowledge, and wisdom that are integral to our practice. We will explore these central concepts in more detail in the next section.
- NI supports nurses, consumers, patients, the interprofessional healthcare team, and all other stakeholders in their decision-making in all roles and settings to achieve desired outcomes. This statement refers to the IT tools that support our practice and help us to collaborate and communicate with other healthcare professionals and that support the evolving trends and tools related to patient engagement in managing their own health. All these tools contribute to better health outcomes. Examples of such tools are EHRs, barcode medication administration systems, clinical decision support and other expert systems, patient monitoring devices, and telehealth tools. These and other NI tools are discussed in subsequent chapters.
- This support is accomplished through the use of information structures, information processes, and information technology. This section of the definition clearly identifies the need for IT to provide structure to the data we collect from our patients and to allow for processing of data and information to create knowledge and support wisdom in nursing practice. Think about the fact that with the advent of clinical information systems (CISs), specifically electronic documentation and clinical decision support (CDS) applications, every nurse has the capacity to contribute to the advancement of nursing knowledge on many levels. Imagine the use of IT solutions to capture not only discrete, quantifiable data but also the nurse's experiential and intuitive personal knowledge not typically documented in paper records. Add to that mix the family history, culture, environmental and social factors, past experiences, and perspectives from patients and families, and it becomes clear that the possibilities for generating new understandings within populations and across the life span and care continuum are endless. Many of these technologies are covered in subsequent chapters.
In 2022, the ANA released the third edition of Nursing Informatics: Scope and Standards of Practice. The third edition is described as “the culmination of a 2-year intensive professional review and revision initiative, complicated by the significant interruptions of the Covid-19 pandemic in 2020 and 2021” (ANA, 2022, p. 1). The ANA offers this current definition of NI:
Nursing informatics is the specialty that transforms data into needed information and leverages technologies to improve health and health care equity, safety, quality, and outcomes. (ANA, 2022, p. 3)
We shall examine the essence of NI in detail in subsequent chapters.
The DIKW Paradigm ⬆ ⬇
The conceptual framework underpinning the science and practice of NI centers on the core concepts of data, information, knowledge, and wisdom, also known as the DIKW paradigm. As an aside, it is important to note that this paradigm is not exclusive to nursing and that it is in fact used by others who work with data and information. When we assess a patient to determine their nursing needs, we gather and then analyze and interpret data to form a conclusion. This is the essence of nursing science. Information is composed of data that were processed using knowledge. Knowledge is the awareness and understanding of a set of information and the ways that information can be made useful to support a specific task or arrive at a decision. When we apply previous knowledge to data, we convert those data into information and information into new knowledge-that is, an understanding of which interventions are appropriate in practice. Thus, information is data made functional through the application of knowledge. Wisdom is the appropriate application of knowledge to a specific situation. In the practice of nursing science, one expects actions to ultimately be directed by wisdom. Wisdom uses knowledge and experience to heighten common sense and insight to exercise sound judgment in practical matters.
Matney et al. (2011) and Topaz (2013) provided these expanded definitions and examples of the DIKW paradigm:
- Data:Data are the smallest components of the DIKW framework. They are commonly presented as discrete facts, the product of observation with little interpretation (Matney et al., 2011). These are the discrete factors describing the patient or their environment. Examples include the patient's medical diagnosis (e.g., International Classification of Diseases [ICD-10] diagnosis #150.20: Unspecified systolic [congestive] heart failure) or living status (e.g., living alone, living with family, or living in a retirement community). A single piece of data, known as datum, often has little meaning in isolation.
- Information:Information might be thought of as “data + meaning” (Matney et al., 2011). Information is often constructed by combining data points into a meaningful picture given a certain context. Information is a continuum of progressively developing and clustered data; it answers questions such as who, what, where, and when. For example, a combination of a patient's “ICD-10 diagnosis #150.20: Unspecified systolic (congestive) heart failure” and living status “living alone” has a certain meaning in the context of an older adult.
- Knowledge:Knowledge is information that has been synthesized so that relations and interactions are defined and formalized; it is built of meaningful information constructed of discrete data points (Matney et al., 2011). Knowledge is often affected by assumptions and central theories of a scientific discipline and is derived by discovering patterns of relationships among clusters of information. Knowledge answers questions of why or how. For healthcare professionals, the combination of information clusters, such as the “ICD-10 diagnosis #150.20: Unspecified systolic (congestive) heart failure” plus living status “living alone,” with additional information that an older man (78 years old) was just discharged from the hospital to home with a complicated new medication regimen (e.g., blood thinners) might indicate that this person is at a high risk for drug-related adverse effects (e.g., bleeding).
- Wisdom:Wisdom is an appropriate use of knowledge to manage and solve human problems (ANA, 2008; Matney et al., 2011). Wisdom implies a form of ethics, or knowing why certain things or procedures should or should not be implemented in healthcare practice. In nursing, wisdom guides the nurse in recognizing the situation at hand, based on the patient's values and the nurse's experience and healthcare knowledge. Combining all these components, the nurse decides on a nursing intervention or action. Benner (2000) presents wisdom as a clinical judgment that integrates intuition, emotions, and the senses. Using the previous examples, wisdom would be displayed when the home care nurse considers prioritizing the elderly heart failure patient who is using blood thinners for an immediate intervention, such as an initial nursing visit within the first hours of discharge from the hospital to ensure appropriate use of medications (para. 2).
Reflect on the examples previously given by Topaz, and create your own example of an application of the DIKW scenario.
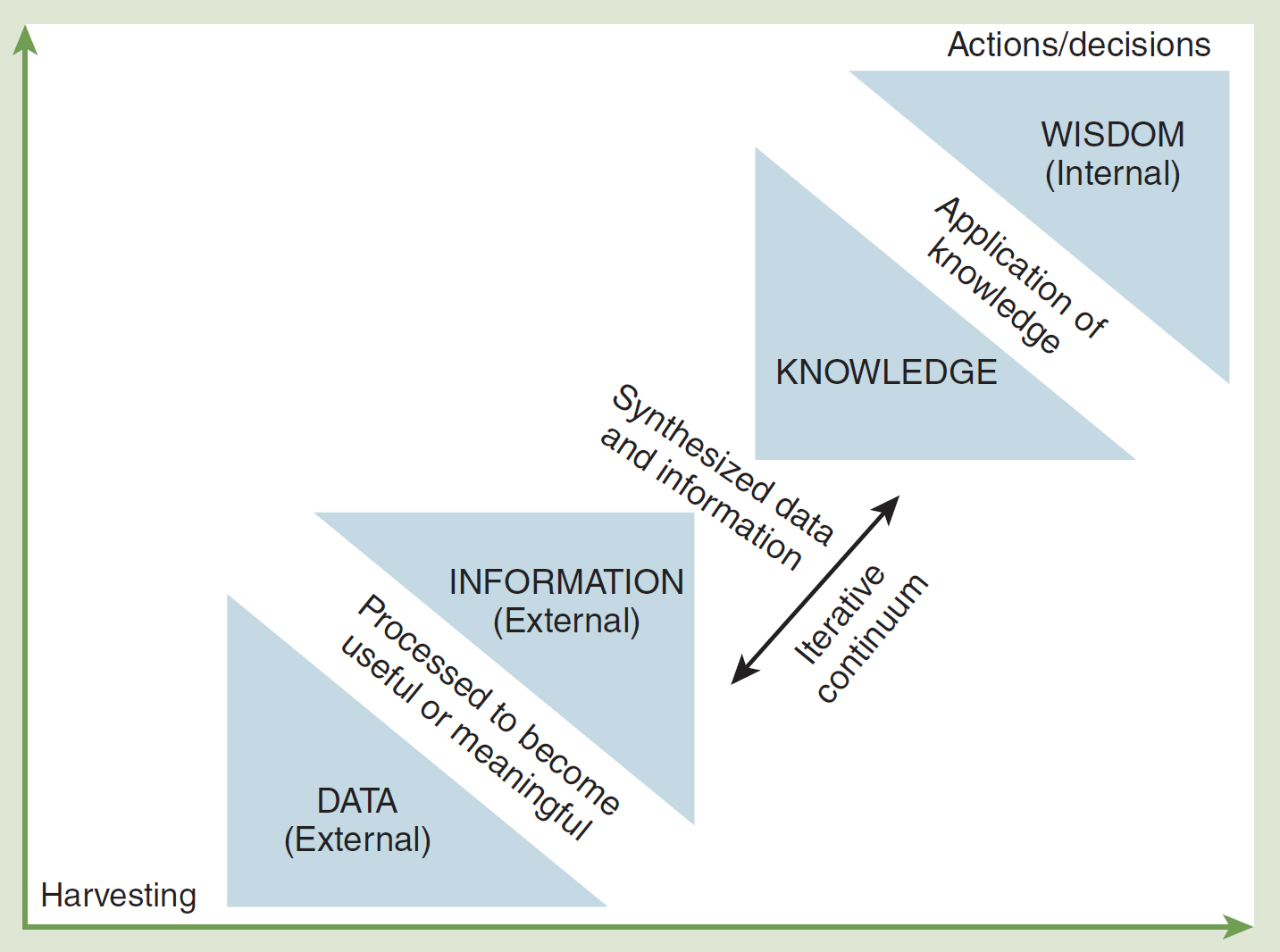
The DIKW paradigm is frequently depicted as a pyramid, which suggests a hierarchy, with data on the bottom, then information, then knowledge, and finally wisdom. With the use of IT solutions to harvest and mine data to extract meaning, this depiction does not really reflect reality. Rowley (2007) suggested that alternate representations might better capture the complexity of these concepts. “Is there a sharp divide between data, information and knowledge, or do they lie on a continuum with different levels of meaning, structure, and actionability occurring at different levels?” (p. 175). Ronquillo et al. (2016) reported that the critiques of the hierarchical DIKW model centered around the suggested linearity and unidirectionality of movement from data to information to knowledge to wisdom. We offer Figure 6-1, which depicts the iterative, or repetitive, nature of our ability (both human and machine) to process data and information to build knowledge and sometimes reach wisdom. There is constant critical thinking (and processing) between information and knowledge. Knowledge can be eventually used to gain wisdom. We believe that most of the critical thinking, analysis, and synthesis occurs between data, information, and knowledge, with some extending to wisdom. The processing of data does not always end with wisdom because of the high degree of human agency in wisdom, but it will end in knowledge that provides a basis for action. As we enhance our knowledge and gain wisdom, the way we process, analyze, synthesize, and disseminate data, information, and knowledge evolves. The result is sound clinical judgment.
Figure 6-1 Moving From Data and Information to Knowledge and Wisdom
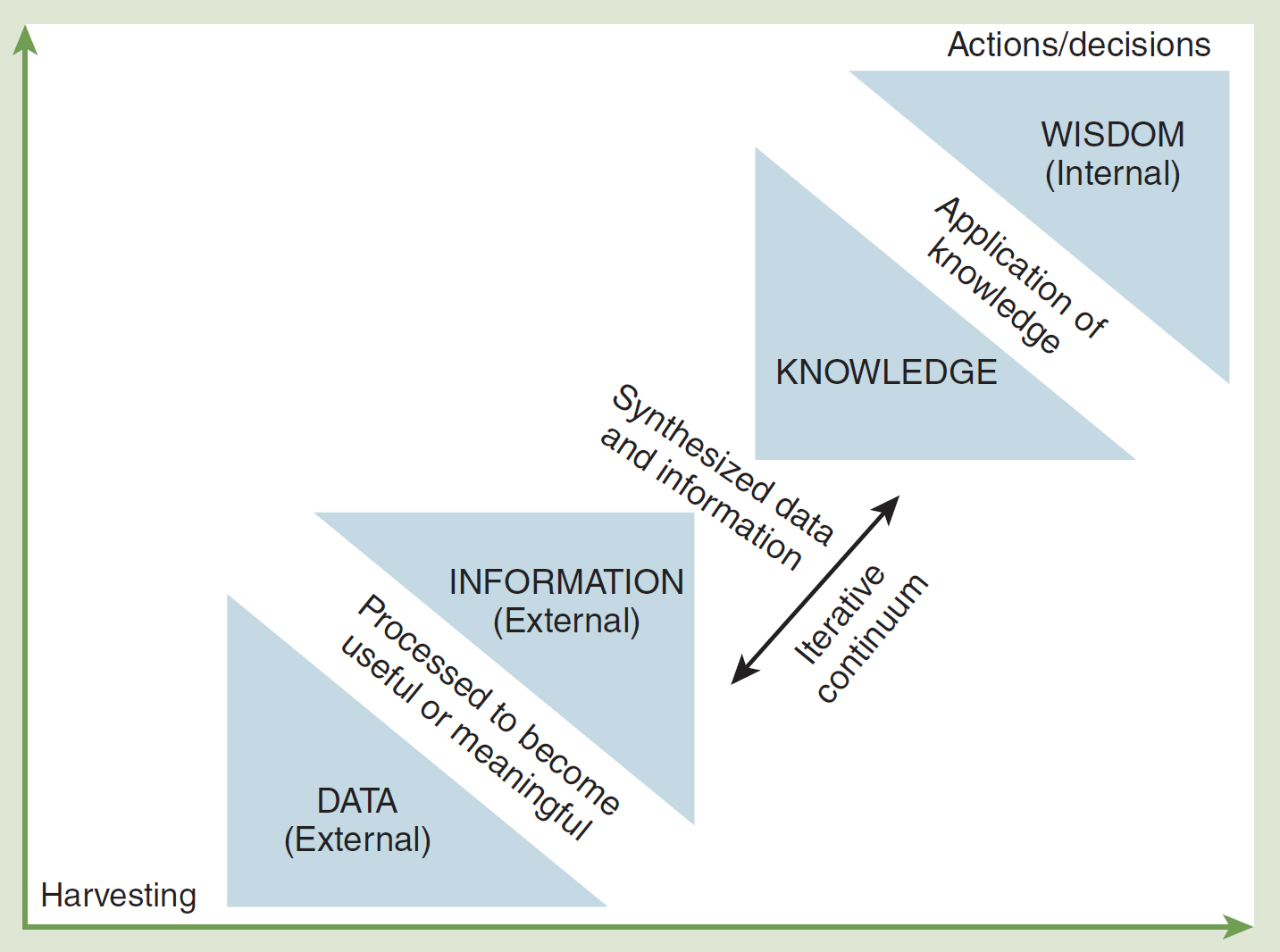
A flow diagram depicts the iterative process of processing data and information to build knowledge and reach wisdom.
The progression from bottom to top includes: Harvesting external data, which is processed to become useful or meaningful external information; Synthesizing data and information in an iterative continuum; Transforming this into knowledge, application of knowledge, and finally, wisdom as internal outcomes leading to actions and decisions.
Rowley (2007) was among the first to map data, information, knowledge, and wisdom to types of IT systems, which suggests that data reside in transaction processing systems; information, in information processing systems; knowledge, in decision support systems (DSSs); and wisdom, in expert systems. As IT tools become more sophisticated, we may gain more insight into how knowledge and wisdom are evolved from data and information. Because of the speed of processing and multiple iterations performed by these sophisticated tools, the lines between data, information, knowledge, and wisdom will be increasingly blurred. What really matters, though, is that the outcomes of this processing will provide important actionable insights to drive nursing practice.
Snyder-Halpern and colleagues (2001) identified four tasks associated with human information processing: (1) data gathering, (2) information use, (3) creative application of knowledge to clinical practice, and (4) generation of new knowledge. These four tasks are associated with the four roles that nurses take on as knowledge workers: data gatherer, information user, knowledge user, and knowledge builder, respectively.
Nurses are data gatherers by nature. They collect and record objective clinical data daily. These items include such things as patients' medical history, vital signs, and assessment data. As data gatherers, nurses transition to information users when they begin to interpret the data that they have collected and recorded. As information users, nurses then structure the clinical data into information that can be used to guide patient-care decisions (Snyder-Halpern et al., 2001). An example of this progression is when nurses notice that a patient's blood pressure is elevated. Information users transition to knowledge users when they notice trends in a patient's clinical data and determine whether the clinical data fall within or outside of the normal data range. Nurses transition from knowledge users to knowledge builders when they examine clinical data and trends across groups of patients. These trends are interpreted and compared to current scientific data to determine whether these data would improve the nursing knowledge domain. An example of the transition of a nurse as knowledge user to a nurse as knowledge builder is an observation of medication compliance rates over a specified time period for patients diagnosed with chronic high blood pressure, with the nurse then comparing these rates to evidence-based literature to determine whether this information improves the nursing knowledge base (Snyder-Halpern et al., 2001).
Snyder-Halpern and colleagues (2001) found that as nurses assumed each of these roles, they required different types of decision support processes to support their knowledge needs. The data gatherer requires a system that captures and stores data accurately and reliably and allows the data to be readily accessed. Most current healthcare DSSs support the nurse in this role. The information user role requires a system that can transform clinical data into a format that allows for easy recognition of patterns and trends. These systems recognize the trend and display it for the nurse, who in turn uses this information to adjust the plan of care for the patient. The information user role is generally well supported by current DSSs. The knowledge user role is the least supported, and many systems are currently looking at ways to support nurses in this role. One advantage of these DSSs is their ability to bring knowledge to nurses so that they do not have to retrieve the information themselves, which allows them to adjust a patient's plan of care in a more efficient and timely manner. The knowledge builder role is typically seen in conjunction with the nurse-researcher and quality management roles. These roles typically look at aggregated data that have been captured over time and from numerous patients. Then these data are compared to clinical variables and interventions. This analysis then results in the development of new domain knowledge (Snyder-Halpern et al., 2001).
Most of the available DSS tools for nursing practice, although promising, are simplistic and in early development. Typically, a DSS includes tools such as (1) computerized alerts and reminders (e.g., medication due, patient has an allergy, or potassium level abnormal), (2) clinical guidelines (e.g., best practices for prevention of skin breakdown), (3) online information retrieval (e.g., CINAHL or drug information), (4) clinical order sets and protocols, and (5) online access to organizational policies and procedures. In the future, these tools may be expanded to include applications with embedded case-based reasoning.
In the context of nursing practice that is supported by CISs, nurses will eventually have access to evidence and knowledge derived from large aggregates of clinical data, including nursing interventions and resultant outcomes. Experiential evidence provides practice guidelines and directives to ensure concurrence with optimal clinical decisions and actions. To illustrate, consider this example: A nurse assesses a patient who has experienced a stroke for signs of skin breakdown, photographs and documents early skin integrity changes, and submits the photos and documentation to the CIS. The nurse receives an option to review the best practices for care of the patient and to submit a request for a consult to a wound management specialist. The ongoing clinical findings, treatment, and response are logged and aggregated with similar cases, thereby contributing to the knowledge base related to nursing and care of the integumentary system.
The informational elements of CISs can also be designed to include specifics about individuals' multicultural practices and beliefs. Consider the situation in which a client voices concerns about her prescribed dietary treatment and expresses a preference for a female care provider. With a query to the CIS for the client's history and sociocultural background, the nurse obtains explanations for these requests that derive from the patient's religious and cultural background and makes a notation to highlight and carry this information forward in the electronic record for any future admissions. Future systems may also be designed to provide access to standards of ethical practice and online access to experts in the field of moral reasoning to guide clinical interactions and decision-making.
Through each instance of interacting with the CIS, nurses add to this repository of knowledge by chronicling their daily clinical challenges and queries. The delivery of personalized, knowledge-based care is enhanced by the continued expansion and aggregation of knowledge about clients and populations, which includes their personal, cultural, physical, and clinical presentations and experiences coupled with the guidance received from others.
Graves and Corcoran (1989) have suggested that nursing knowledge is “simultaneously the laws and relationships that exist between the elements that describe the phenomena of concern in nursing (factual knowledge) and the laws or rules that the nurse uses to combine the facts to make clinical nursing decisions” (p. 230). In their view, not only does knowledge support decision-making, but it also leads to new discoveries. Thus, one might think about the future creation of nursing knowledge as being the discovery of new laws and relationships that can continue to advance nursing practice.
New technologies have made the capture of multifaceted data and information possible using such technologies as digital imaging (e.g., photography to support wound management). Now included as part of the clinical record, such images add a new dimension to the assessment, monitoring, and treatment of illness and the maintenance of wellness. Beyond the use of computer keyboards, input devices are being integrated with CISs and used to gather data and information for the following clinical and administrative purposes:
- Biometrics (e.g., facial recognition and security)
- Voice and video recordings (e.g., client interviews and observations, diagnostic procedures, and ultrasounds)
- Voice-to-text files (e.g., voice recognition for documentation)
- Medical devices (e.g., infusion pumps, ventilators, and hemodynamic monitors)
- Barcode and radio-frequency identification (RFID) technologies (e.g., medication administration)
- Telehomecare monitoring (e.g., for use in diabetes and other chronic disease management)
These are but a few of the emerging capabilities that allow for numerous data inputs to be transposed, combined, analyzed, and displayed to provide information and views of clinical situations currently not possible with hard copy documentation. Through the application of information and communication technologies to support the capture and processing (i.e., interpreting, organizing, and structuring) of all relevant clinical data, relationships can be identified and formalized into new knowledge. This transformational process is at the core of generating new nursing knowledge at a rate never experienced before; in the context of current research paradigms, the same relationships would likely take years to uncover.
As CISs advance, nurses will eventually become generators of new knowledge by virtue of designs that embed machine learning and case-based reasoning methods within their core functionality. This functionality will become possible only with national and international adoption of a standardized nursing language, which is described in the following section. Imagine the power of having access to systems that aggregate the same data elements and information garnered from multiple clinical situations and provide a probability estimate of the likely outcome for individuals of a certain age, with a specific diagnosis and comorbid conditions, medication profile, symptoms, and interventions. How much more rapidly would an understanding of the efficacy of clinical interventions be elucidated? Historically, some knowledge might have taken years of research to discover-for example, that sometimes long-standing practices are more harmful than beneficial. A case in point is the long-standing practice of instilling endotracheal tubes with normal saline before suctioning (O'Neal et al., 2001). Based on the evidence gathered through several studies, the potentially deleterious effects of this practice have become widely recognized. Conceivably, a meta-analysis approach to clinical studies would be expedited by convergence of large clinical data repositories across care settings, thereby making available to practitioners the collective contributions of health professionals and longitudinal outcomes for individuals, families, and populations.
Nurses need to be engaged in the design of CIS tools that support access to and the generation of nursing knowledge. As we have emphasized, the adoption of clinical data standards is of particular importance to the future design of CIS tools. We are also beginning to see the development and use of expert systems, which implement knowledge automatically without human intervention. For example, an insulin pump that senses the patient's blood glucose level and administers insulin based on those data is a form of an expert system. Expert systems differ from decision support tools in that the decision support tools require the human to act on the information provided, whereas expert systems intervene automatically, based on an algorithm that directs the intervention. Consider that as CISs are widely implemented, standards for nursing documentation and reporting are adopted, and healthcare IT solutions continue to evolve, the synthesis of findings from a variety of methods and worldviews becomes much more feasible.
Central to the development of robust expert systems is the agreement on and use of standard data formats and terminologies that accurately codify and capture the essence of nursing processes and outcomes in these electronic systems. Consider that physician contributions to the health of a patient have been specifically codified (and billed) for some time (i.e., ICD-10). What if we were able to code and thus capture nursing contributions in a similar way? This information would help to highlight the specific nursing contributions to patient outcomes.
Capturing and Codifying the Work of Nursing ⬆ ⬇
There are major efforts underway-internationally through the International Council of Nurses' International Classification of Nursing Practice (ICNP) and in many other initiatives among and within countries-in which nurses are attempting to standardize the language of nursing practice (Hannah et al., 2009). These efforts are particularly important in the face of the development of EHRs and health information exchanges (HIEs), which have been stimulated by the HITECH Act of 2009. The capacity to encourage and enforce consistent nomenclatures that reflect the practice of nurses is now possible. Standardized language gives both the nursing profession and the healthcare delivery systems the capability to capture, codify, retrieve, and analyze the impact of nursing care on client outcomes. For example, with the use and documentation of standardized client assessments, including risk measures, interventions based on best practices, and consistently measured outcomes within different care settings and across the continuum of care, there will be an ability to demonstrate more clearly the contributions and impact of nursing care through the analysis of EHR outputs. In addition, clinical outcomes can be further understood in the context of care environments, particularly implications related to the availability of human and material resources to support care delivery. The standardization of clinical inputs and outputs into EHRs will eventually provide a rich knowledge base from which practice and research can be enhanced and administrative and policy decisions can be better informed (Nagle et al., 2010). According to Androwich (2010), it is important to understand that there is a dual role for accessing and using information (content) in health care. In the first instance, when the nurse is caring for an individual patient, evidence-based information (content) and patient data need to be available at the point of care to inform the present patient encounter. In the second instance, patient data that are entered by the nurse in the process of documentation need to be entered in such a manner that they are able to be aggregated to inform future patient encounters.
Rutherford (2008) provided this insight:
A standardized nursing language should be defined so that nursing care can be communicated accurately among nurses and other health care providers. Once standardized, a term can be measured and coded. Measurement of the nursing care through a standardized vocabulary by way of an ED [electronic documentation] will lead to the development of large databases. From these databases, evidence-based standards can be developed to validate the contribution of nurses to patient outcomes. (para. 5)
Thede and Schwiran (2011) identified the benefits of using standardized terminology as (1) better communication among nurses and other healthcare providers, (2) increased visibility of nursing interventions, (3) improved patient care, (4) enhanced data collection to evaluate nursing care outcomes, (5) greater adherence to standards of care, and (6) facilitation of assessment of nursing competency (para. 2).
Think about this. Some EHRs measure height in feet and inches and others in centimeters. Weight may be measured in pounds or kilograms. If we wanted to compare patient data from multiple EHRs in several healthcare institutions to develop a model to predict the onset of type 2 diabetes, these disparate measures would not translate well. Some EHRs force data collection into coded database fields, and thus these data are more easily analyzed for trends than those same data recorded as free text. Clinicians who are used to recording data (charting) as text may resist the use of the coded data fields that are typically presented as drop-down menus in the EHR. As Skrocki (2013) pointed out, “Data interoperability is hindered when clinicians utilize free text documentation. Although text data can be searched with a specific word or word phrases, it does not allow for optimal data sharing. When an organization transfers data to another organization, standardized codified data allows for better data interpretation” (p. 77).
Although significant progress has been made in this standardization work, it is still evolving. Box 6-1 discusses the evolution of standardized terminologies in nursing; it was contributed by Nicholas Hardiker (2011), a leader in the development of standardized languages that support clinical applications of information and communication technology.
| Box 6-1 The Evolution of Standardized Terminologies to Support |
|---|
| Nicholas Hardiker |
| Nursing Practice |
|---|
| Agreement on the consistent use of a term, such as impaired physical mobility allows that term to be used for a number of purposes: to provide continuity of care from care provider to care provider, to ensure care quality by facilitating comparisons between care providers, or to identify trends through data aggregation. Since the early 1970s, there has been a concerted effort to promote consistency in nursing terminology. This work continues today, driven by the following increasing demands placed on health-related information and knowledge: |
- Accessibility:Accessibility means that the information and knowledge needed to deliver care or manage a health service should be easy to access.
- Ubiquity:Ubiquity means that with changing models of healthcare delivery, information and knowledge should be available anywhere.
- Longevity: Information should be usable beyond the immediate clinical encounter.
- Reusability:Reusability means that information should be useful for a range of purposes.
Without consistent terminology, nursing runs the risk of becoming invisible; nursing will remain difficult to quantify, the unique contribution and impact of nursing will go unrecognized, and the nursing component of EHR systems will remain rudimentary at best. Not least, without consistent terminology, the nursing knowledge base will suffer in terms of development and access, thereby delaying the integration of evidence-based health care into nursing practice. External pressures merely compound this problem. For example, in the United States, the HITECH Act, signed in January 2009, provided a financial incentive for the use of EHRs; similar steps were taken in other regions. The HITECH Act mandated that EHRs be used in a meaningful way, but without consistent terminology, achieving this goal will be problematic. Finally, the current and future landscape of information and communication technologies (e.g., connection anywhere, borderless communication, web-based applications, collaborative working, disintermediation and reintermediation, consumerization, ubiquitous advanced digital content [van Eecke et al., 2007]) and their inevitable infiltration into health care will only serve to reinforce the need for consistent nursing terminology while providing an additional sense of urgency. This box explains what is meant by a standardized nursing terminology and lists several examples. It describes in detail the different approaches taken in the development of two terminologies. It presents, in the form of an international technical standard, a means of ensuring consistency among the plethora of contemporary standardized nursing terminologies, with a view toward harmonization and possible convergence. Finally, it provides a rationale for the shared development of models of terminology use-models that embody both clinical and pragmatic knowledge to ensure that contemporary nursing record systems reflect the best available evidence and fit comfortably with routine practice. |
| Standardized Nursing Terminologies |
|---|
| A term at its simplest level is a word or phrase used to describe something concrete (e.g., leg) or abstract (e.g., plan). A nursing terminology is a body of the terms used in nursing. Many nursing terminologies exist, both formal and informal. Nursing terminologies allow nurses to consistently capture, represent, access, and communicate nursing data, information, and knowledge. A standardized nursing terminology is a nursing terminology that is in some way approved by an appropriate authority (de jure standardization) or by general consent (de facto standardization).
In North America, one such authority was the ANA, which operated a process of de jure standardization through its Committee for Nursing Practice Information Infrastructure (CNPII), which now no longer exists. The CNPII recognized two data element sets: the Nursing Minimum Data Set (NMDS) and the Nursing Management Minimum Data Set (NMMDS). In the United States, work on a standardized data element set for nursing began in the 1980s with the NMDS (Werley & Lang, 1988), which provided an additional catalyst for the development of many nursing terminologies that could provide values (e.g., chronic pain) for particular data elements in the NMDS (e.g., nursing diagnosis). The data element sets provided a framework for the uniform collection and management of nursing data and encouraged the use of a standardized nursing terminology to represent those data as a way to enhance consistency.
|
| Approaches to Nursing Terminology |
|---|
| From relatively humble beginnings, nursing terminologies have evolved significantly over the past several decades in line with best practices in terminology work. The enumerative approach consists of words or phrases in a list or a simple hierarchy format. In the nursing diagnosis terminology system of the North American Nursing Diagnosis Association (NANDA), a nursing diagnosis has an associated name and a textual definition (NANDA International, 2008). Each nursing diagnosis may have a set of defining characteristics and related risk factors. These additional features do not constitute part of the core terminology but instead are intended to be used as an aid to diagnosis. What an enumerative approach to standardizing terminology may lack in terms of hierarchical sophistication, it makes up for in terms of simplicity and potential ease of implementation and use.
In contrast, the ontological approach is compositional in nature and provides a partial representation of the entities within a domain and the relationships between them. The evolution of this approach to terminology standardization has been facilitated by advances in knowledge representation (e.g., the refinement of the description logic that underpins many contemporary ontologies) and in their accompanying technologies (e.g., automated reasoners that can check consistency and identify equivalence) as well as the subsumption (i.e., subclass-superclass) relationships within those ontologies.
ICNP version 2 is an example of an ontology. ICNP is described as a unified nursing language system. It seeks to provide a resource that can be used to develop local terminologies and facilitate cross-mapping between terminologies to compare and combine data from different sources; the existence of a number of overlapping but inconsistent standardized nursing terminologies is problematic in terms of data comparison and aggregation. The core of ICNP is represented in the Web Ontology Language (OWL), a recommendation of the World Wide Web Consortium (W3C) and a de facto standard language for representing ontologies (McGuiness & van Harmelen, 2004). Because it is underpinned by description logic, OWL permits the use of automated reasoners that can check consistency, identify equivalence, and support classification within the ICNP ontology.
The results of contemporary terminology work are encouraging. Nevertheless, further work is needed to harmonize standardized nursing terminologies and scale up and mainstream the development and implementation of models of terminology use.
|
At least two decades of work have been directed toward articulating standardized data elements that reflect nursing practice. The nursing profession has been steadily moving toward consensus on the adoption of data standards. In fact, several “consensus conferences” have been hosted in recent years by the University of Minnesota, with the goal to develop “a national action plan and harmonize existing and new efforts of multiple individuals and organizations to expedite integration of standardized nursing data within EHRs and ensure their availability in clinical data repositories for secondary use” (Westra et al., 2015, para. 3). See Chapter 14, The Electronic Health Record and Clinical Informatics, for more information about using standardized terminologies in the EHR.
The National Library of Medicine has been designated by the Department of Health and Human Services as the central coordinating body for clinical terminology standards. Its web page (www.nlm.nih.gov/healthit/index.html) provides several training and implementation resources as well as current information on updates to important terminologies.
The Office of the National Coordinator for Health Information Technology (ONC) has also been working diligently to develop national standards for EHR interoperability. The result of the work is the United States Core Data for Interoperability (USCDI) Version 3 released in July 2022. “The USCDI is a standardized set of health data classes and constituent data elements for nationwide, interoperable health information exchange” (ONC, 2022, para. 1). Access the USCDI here: www.healthit.gov/isa/sites/isa/files/2022-07/USCDI-Version-3-July-2022-Final.pdf.
The ANA (2018) updated its position statement and advocated for “the use of the ANA recognized terminologies supporting nursing practice within the Electronic Health Record (EHR) and other health information technology solutions” (para. 2). A landscape analysis of standard nursing terminologies, conducted by the ONC (2017), reported that the ANA recognizes 12 standard nursing terminologies-2 minimum data sets, 2 reference terminologies, and 8 interface terminologies. These terminologies are provided in Box 6-2.
| Box 6-2 ANA-Recognized Standard Nursing Terminologies |
|---|
| Minimum Data Sets |
|---|
|
| Reference Terminologies |
|---|
|
| Interface Terminologies |
|---|
|
Consider that as clinical information systems are widely implemented, standards for nursing documentation and reporting are adopted, and healthcare IT solutions continue to evolve, the synthesis of findings from a variety of methods and worldviews becomes much more feasible. As we move toward a standard terminology to capture the work of nursing, we will also have the ability to mine electronic record data to tease out best practices and promote care improvements. It is important to note that we do not yet have an agreed-upon standardized terminology for nursing documentation in the EHR, as demonstrated by the list of eight ANA-recognized interface terminologies in Box 6-2. This fact is hampering seamless data exchanges among competing healthcare systems and opportunities for data mining and research. One interesting and highly developed terminology system for documenting nursing care in an EHR is the CCC (https://careclassification.org). An overview and examples of the use of this system are presented in Box 6-3.
| Box 6-3 Clinical Care Classification System |
|---|
| Framework |
|---|
| The CCC was developed by Virginia Saba and colleagues to provide a standardized approach to clinical care documentation in an EHR. The CCC consists of 4 health care patterns (i.e., physiological, psychological, functional, and health behavioral); 21 care component classes (e.g., activity, behavior, medication, nutrition, and elimination); 176 nursing diagnoses, 804 nursing interventions/actions, and 528 nursing outcomes; 3 outcome qualifiers (i.e., improved, stabilized, and deteriorated); and 4 action type qualifiers (i.e., monitor, perform, teach, or manage) (https://careclassification.org/framework). |
| Coding Structure |
|---|
| The concept codes promote information exchange and interoperability. Each code consists of five alphanumeric characters:
1st: Alpha character represents = care component = A
2nd: Two or three digits represent = nursing concepts = A02.1
|
- A nursing concept represents either a nursing diagnosis or a nursing intervention.
5th: Last digit represents either Examples: - Diagnosis code A.01.4.1
- Intervention code A.01.3.1
Summary of steps used to build code: - Assessment: A-Activity
- Diagnosis: 01.4 (subdiagnosis)-Fatigue
- Outcome identification: 1-Improve
- Planning: 03.1 (subintervention)-Ambulation therapy
- Implementation (action type): 1-Assess
- Evaluation (outcome): 1-Improved
The Online Code Builder tool allows you to practice with the system to appreciate its comprehensiveness. Please visit the following website to experience code building for yourself: https://careclassification.org/online-code-builder-1. |
IT is not a panacea for all the challenges found in health care, but it will provide the nursing profession with an unprecedented capacity to generate and disseminate new knowledge at a rapid speed, thus supporting the knowledge work of nursing. To practice effectively in this ever-changing environment, all healthcare professionals, regardless of specialty, will need a basic level of informatics education. Here we will focus on NI education.
Nursing Informatics Education ⬆ ⬇
If we are to fully embrace the knowledge work of nursing, we must also embrace technologies that support knowledge and practice. The future of nursing science and NI is closely associated with nursing education and nursing research. Skiba (2007) suggested that technologically savvy and well-informed faculty who can demonstrate the appropriate use of technologies to enhance the delivery of nursing care are needed. Along those lines, Whitman-Price et al. (2012) conducted research among senior nursing students to determine perceptions of personal phone use to access healthcare information during clinical experiences. Their study indicated that ready access to electronic resources enhanced clinical decision-making and confidence in patient care. As early as 2007, Girard discussed cutting-edge operating room technologies, such as nanosurgery using nanorobots, smart fabrics that aid in patient assessment during surgery, biopharmacy techniques for the safe and effective delivery of anesthesia, and virtual reality training. She made an extremely provocative point about nursing education: “Educators will need to expand their knowledge and teach for the future and not the past. They must take heed that the old tried-and-true nursing education methods and curriculum that has lasted 100 years will have to change, and that change will be mandated for all areas of nursing” (p. 353). Bassendowski (2007) specifically addressed the potential for the generation of knowledge in educational endeavors as faculty apply new technologies to teaching and the focus shifts away from individual to group instruction, which promotes sharing and processing of knowledge. We are also likely to see more interprofessional education initiatives because professionals must be prepared to work together and support one another to ensure robust patient outcomes.
Several key national groups continue to promote the inclusion of informatics content in nursing education programs. These initiatives include the Vision Series by the National League for Nursing (NLN) (2015), the Quality and Safety Education for Nurses (QSEN; n.d.-b) learning modules, and the Technology Informatics Guiding Education Reform (TIGER) initiative (Healthcare Information and Management Systems Society, n.d.). These organizations focus on the need to integrate informatics competencies into nursing curricula to prepare future nurses for the tasks of managing data, information, and knowledge; alleviating errors and promoting safety; supporting clinical judgment and decision-making; and improving the quality of patient care. Nurse educators are challenged to prepare informatics-competent nurses who can practice safely in technology-laden settings.
The TIGER (2007) initiative identified steps toward a 10-year vision and stated a key purpose: “to create a vision for the future of nursing that bridges the quality chasm with information technology, enabling nurses to use informatics in practice and education to provide safer, higher-quality patient care” (p. 4). The pillars of the TIGER vision include the following:
- Management & Leadership: Revolutionary leadership that drives, empowers, and executes the transformation of health care.
- Education: Collaborative learning communities that maximize the possibilities of technology toward knowledge development and dissemination, driving rapid deployment and implementation of best practices.
- Communication & Collaboration: Standardized, person-centered, technology-enabled processes to facilitate teamwork and relationships across the continuum of care.
- Informatics Design: Evidence-based, interoperable intelligence systems that support education and practice to foster quality care and safety.
- Information Technology: Smart, people-centered, affordable technologies that are universal, useable, useful, and standards based.
- Policy: Consistent, incentives-based initiatives (organizational and governmental) that support advocacy and coalition-building, achieving and resourcing an ethical culture of safety.
- Culture: A respectful, open system that leverages technology and informatics across multiple disciplines in an environment where all stakeholders trust each other to work together toward the goal of high quality and safety. (p. 4)
The American Association of Colleges of Nursing (AACN) has embraced a competency-based model of nursing education. The Essentials: Core Competencies for Professional Nursing Education released in 2021 consists of 10 essential domains with each having 2 levels of subcompetencies reflecting entry-level and advanced-level education (AACN, 2021a). Domain 8 is titled Informatics and Healthcare Technologies and includes five competencies with subcompetencies specific to entry-level and advanced-level nursing education. The five competencies follow:
- Describe the various information and communication technology tools used in the care of patients, communities, and populations.
- Use information and communication technology to gather data, create information, and generate knowledge.
- Use information and communication technologies and informatics processes to deliver safe nursing care to diverse populations in a variety of settings.
- Use information and communication technology to support documentation of care and communication among providers, patients, and all system levels.
- Use information and communication technologies in accordance with ethical, legal, professional, and regulatory standards, and workplace policies in the delivery of care. (AACN, 2021b, para. 3)
You can view the specifics of the competencies and subcompetencies for this domain at www.aacnnursing.org/Essentials/Domains/Informatics-and-Healthcare-Technologies.
Quality and Safety Education for Nurses ⬆ ⬇
As nursing science evolves, it is critical that patient care improve. Unfortunately, sometimes patient care is unsafe and less than adequate. Therefore, quality and safety have become paramount. The QSEN Institute project seeks to prepare future nurses who will have the knowledge, skills, and attitudes (KSAs) necessary to continually improve the quality and safety of the healthcare systems within which they work.
Prelicensure informatics KSAs are shown in Table 6-1 (QSEN Institute, n.d.-c). Graduate-level informatics KSAs are shown in Table 6-2 (QSEN Institute, n.d.-a).
Table 6-1 Prelicensure Informatics KSAsKnowledge | Skills | Attitudes |
|---|
Explain why information and technology skills are essential for safe patient care | Seek education about how information is managed in care settings before providing care Apply technology and information management tools to support safe processes of care | Appreciate the necessity for all health professionals to seek lifelong, continuous learning of information technology skills |
Identify essential information that must be available in a common database to support patient care Contrast benefits and limitations of different communication technologies and their impact on safety and quality | Navigate the electronic health record Document and plan patient care in an electronic health record Employ communication technologies to coordinate care for patients | Value technologies that support clinical decision-making, error prevention, and care coordination Protect the confidentiality of protected health information in electronic health records |
Describe examples of how technology and information management are related to the quality and safety of patient care Recognize the time, effort, and skill required for computers, databases, and other technologies to become reliable and effective tools for patient care | Respond appropriately to clinical decision-making supports and alerts Use information management tools to monitor outcomes of care processes Use high-quality electronic sources of healthcare information | Value nurses' involvement in design, selection, implementation, and evaluation of information technologies to support patient care |
Informatics definition: Use information and technology to communicate, manage knowledge, mitigate error, and support decision-making. |
Reproduced from Cronenwett, L., Sherwood, G., Barnsteiner, J., Disch, J., Johnson, J., Mitchell, P., Sullivan, D. T., & Warren, J. (2007). Quality and safety education for nurses. Nursing Outlook, 55(3), 122-131. http://dx.doi.org/10.1016/j.outlook.2007.02.006. Copyright 2007, with permission from Elsevier.
Table 6-2 Graduate-Level Informatics KSAsKnowledge | Skills | Attitudes |
|---|
Contrast benefits and limitations of common information technology strategies used in the delivery of patient care Evaluate the strengths and weaknesses of information systems used in patient care | Participate in the selection, design, implementation, and evaluation of information systems Communicate the integral role of information technology in nurses' work Model behaviors that support implementation and appropriate use of electronic health records Assist team members to adopt information technology by piloting and evaluating proposed technologies | Value the use of information and communication technologies in patient care |
Formulate essential information that must be available in a common database to support patient care in the practice specialty Evaluate benefits and limitations of different communication technologies and their impact on safety and quality | Promote access to patient care information for all professionals who provide care to patients Serve as a resource for how to document nursing care at basic and advanced levels Develop safeguards for protected health information Champion communication technologies that support clinical decision-making, error prevention, care coordination, and protection of patient privacy | Appreciate the need for consensus and collaboration in developing systems to manage information for patient care Value the confidentiality and security of all patient records |
Describe and critique taxonomic and terminology systems used in national efforts to enhance interoperability of information systems and knowledge management systems | Access and evaluate high-quality electronic sources of healthcare information Participate in the design of clinical decision-making supports and alerts Search, retrieve, and manage data to make decisions using information and knowledge management systems Anticipate unintended consequences of new technology | Value the importance of standardized terminologies in conducting searches for patient information Appreciate the contribution of technological alert systems Appreciate the time, effort, and skill required for computers, databases, and other technologies to become reliable and effective tools for patient care |
Informatics definition: Use information and technology to communicate, manage knowledge, mitigate error, and support decision-making. |
Reproduced from Cronenwett, L., Sherwood, G., Pohl, J., Barnsteiner, J., Moore, D., Sullivan, D., Ward, D., & Warren, J. (2009). Quality and safety education for advanced nursing practice. Nursing Outlook, 57(6), 338-348. http://dx.doi.org/10.1016/j.outlook.2009.07.009. Copyright 2009, with permission from Elsevier.
| Case Study: Casting to the Future |
|---|
| In the year 2030, enabled by technology, nursing practice has created a professional culture of reflection, critical inquiry, and interprofessional collaboration. Nurses use technology at the point of care in all clinical settings (e.g., primary, acute, community, and long-term care) to inform their clinical decisions and effect the best possible outcomes for their clients. Information is gathered and retrieved via human-technology biometric interfaces, including voice, visual, sensory, gustatory, and auditory interfaces, which continuously monitor physiological parameters for potentially harmful imbalances. Longitudinal records are maintained for all citizens, from their initial prenatal assessment to death; all lifelong records are aggregated into the knowledge bases of expert systems. These systems provide the basis of the artificial intelligence being embedded in emerging technologies. Smart technologies and invisible computing are ubiquitous in all sectors where care is delivered. Clients and families are empowered to review and contribute actively to their record of health and wellness. Invasive diagnostic techniques are obsolete, nanotechnology therapeutics are the norm, and robotics supplement or replace much of the traditional work of all health professions. Nurses provide expertise to citizens to help them effectively manage their health and wellness life plans and navigate access to appropriate information and services.
The basic education of all health professions will evolve over the next decade to incorporate core informatics competencies. In general, clinical care environments will be connected, and information will be integrated across disciplines to the benefit of care providers and citizens alike. The future of health care will be highly dependent on the use of CISs and CDSs to achieve the global aspiration of safe and quality care for all citizens.
The ideal is a nursing practice that has wholly integrated informatics and nursing education and that is driven using information and knowledge from a myriad of sources, creating practitioners whose way of being is grounded in informatics. Nursing research is dynamic and an enterprise in which all nurses are engaged by virtue of their use of technologies to gather and analyze findings that inform specific clinical situations. In every practice setting, the contributions of nurses to the health and well-being of citizens will be highly respected and will parallel, if not exceed, the preeminence granted physicians.
|
The Future ⬆ ⬇
The future landscape is yet to be fully understood as technology continues to evolve with a rapidity that is rich with promise and potential peril. The previous case study helps us to imagine what future practice might entail. Nurse informaticists and nurse executives are anticipating that computing power will be capable of aggregating and transforming additional multidimensional data and information sources (e.g., historical, multisensory, experiential, and genetic sources) into CIS. With the availability of such rich repositories, further opportunities will open to enhance the education of health professionals, advance the design and application of CDSs, deliver care that is informed by the most current evidence, and engage with individuals and families in ways yet unimagined.
Summary ⬆ ⬇
In this chapter, we have defined NI, reviewed the historical evolution of informatics, and explored the DIKW paradigm central to informatics. We also explored the need for and the development of standardized nursing terminologies to capture and codify the work of nursing and how NI supports the knowledge work of nursing. An overview of initiatives to integrate informatics education in both undergraduate and graduate nursing programs was also provided. This chapter advanced the view that every nurse's practice will make contributions to new nursing knowledge to support clinical judgment in dynamically interactive CIS environments. The core concepts associated with informatics will become embedded in the practice of every nurse, whether administrator, researcher, educator, or practitioner. Informatics will be prominent in the knowledge work of nurses, yet it will be a subtlety because of its eventual transparent integration with clinical care processes. Today and tomorrow, clinical care and clinical judgment will be substantially supported by the capacity and promise of technology.
Most importantly, readers need to contemplate a future that is not limited by the world of practice as it is known today. IT is not a panacea for all the challenges found in health care, but it will provide the nursing profession with an unprecedented capacity to rapidly generate and disseminate new knowledge. Realizing these possibilities necessitates that all nurses understand and leverage the informatician within and contribute to the future.
| Thought-Provoking Questions |
|---|
- How is the concept of wisdom in NI like or unlike professional nursing judgment? Can any aspect of nursing wisdom be automated?
- How can a single agreed-upon model of terminology use (with linkages to a single terminology) help to integrate knowledge into routine clinical practice?
- Can you create examples of how expert systems (not decision support systems but true expert systems initiating actions without human intervention) can be used to support nursing practice?
- How would you incorporate the data-to-wisdom continuum into a job description for nurses?
- What are the possibilities for accelerating the generation and uptake of new nursing knowledge?
|
References ⬆
- American Association of Colleges of Nursing. (2021a). The essentials: Core competencies for professional nursing education.www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf
- American Association of Colleges of Nursing. (2021b). The essentials: Domain 8: Informatics and healthcare technologies.www.aacnnursing.org/Essentials/Domains/Informatics-and-Healthcare-Technologies
- American Nurses Association. (2008). Nursing informatics: Scope and standards of practice.Nursesbooks.org.
- American Nurses Association. (2015). Nursing informatics: Scope and standards of practice (2nd ed.). Nursesbooks.org.
- American Nurses Association. (2018). Inclusion of recognized terminologies supporting nursing practice within electronic health records and other health information technology solutions. www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/Inclusion-of-Recognized-Terminologies-Supporting-Nursing-Practice-within-Electronic-Health-Records
- American Nurses Association. (2022). Nursing informatics: Scope and standards of practice (3rd ed.). Nursesbooks.org.
- Androwich I. (2010, June 4). We the people: How nursing informatics can contribute to healthcare reform through patient-centric HIT [Conference session]. Delaware Valley Nursing Informatics Annual Meeting, Malvern, Pennsylvania.
- Bassendowski S. (2007). NursingQuest: Supporting an analysis of nursing issues. Journal of Nursing Education, 46(2), 92-95. http://dx.doi.org/10.3928/01484834-20070201-11
- Benner P. (2000). The wisdom of our practice. American Journal of Nursing, 100(10), 99-101, 103, 105. https://doi.org/10.2307/3522335
- Blum B. (1986). Clinical information systems. Springer-Verlag.
- Girard N. (2007). Science fiction comes to the OR. AORN Journal, 86(3), 351-353. https://aornjournal.onlinelibrary.wiley.com/doi/abs/10.1016/j.aorn.2007.08.003
- Graves J., & Corcoran S. (1989). The study of nursing informatics. Image: Journal of Nursing Scholarship, 21(4), 227-230. http://dx.doi.org/10.1111/j.1547-5069.1989.tb00148.x
- Hannah K. J., White P., Nagle L. M., & Pringle D. M. (2009). Standardizing nursing information in Canada for inclusion in electronic health records: C-HOBIC. Journal of the American Medical Informatics Association, 16(4), 524-530. https://doi.org/10.1197/jamia.M2974
- Hardiker N. (2011). Developing standardized terminologies to support nursing practice. In D.McGonigle & K.Mastrian (Eds.), Nursing informatics and the foundation of knowledge (2nd ed., pp. 111-120). Jones & Bartlett Learning.
- Healthcare Information and Management Systems Society. (n.d.). TIGER initiative for technology and health informatics education. www.himss.org/tiger-initiative-technology-and-health-informatics-education
- Matney S., Brewster P., Sward K., Cloyes K., & Staggers N. (2011). Philosophical approaches to the data-information-knowledge-wisdom framework. Advances in Nursing Science, 34(1), 6-18. https://doi.org/10.1097/ANS.0b013e3182071813
- Murphy J. (2010). Nursing informatics: The intersection of nursing, computer, and information sciences. Nursing Economic$, 28(3), 204-207.
- Nagle L. M., White P., & Pringle D. (2010). Realizing the benefits of standardized measures of clinical outcomes. Electronic Healthcare, 9(2), e3-e9.
- National League for Nursing. (2015). A vision for the changing faculty role: Preparing students for the technological world of health care. www.nln.org/docs/default-source/uploadedfiles/about/nln-vision-series-position-statements/nlnvision-8.pdf?sfvrsn=1219df0d_0
- O'Connor J. J., & Robertson E. F. (2003). Florence Nightingale. MacTutor. http://mathshistory.st-andrews.ac.uk/Biographies/Nightingale.html
- Office of the National Coordinator for Health Information Technology. (2017). Standard nursing terminologies: A landscape analysis. https://www.healthit.gov/sites/default/files/snt_final_05302017.pdf
- Office of the National Coordinator for Health Information Technology. (2022). United States Core Data for Interoperability (USCDI), Version 3. www.healthit.gov/isa/sites/isa/files/2022-07/USCDI-Version-3-July-2022-Final.pdf
- O'Neal P. V., Grap M. J., Thompson C., & Dudley W. (2001). Level of dyspnoea experienced in mechanically ventilated adults with and without saline instillation prior to endotracheal suctioning. Intensive Critical Care Nursing, 17(6), 356-363. https://doi.org/10.1054/iccn.2001.1604
- Ozbolt J., & Saba V. (2008). A brief history of nursing informatics in the United States of America. Nursing Outlook, 56(5), 199-205. https://doi.org/10.1016/j.outlook.2008.06.008
- Quality and Safety Education for Nurses Institute. (n.d.-a). Graduate QSEN competencies. www.qsen.org/competencies/graduate-ksas
- Quality and Safety Education for Nurses Institute. (n.d.-b). QSEN learning modules. www.aacnnursing.org/our-initiatives/education-practice/teaching-resources/qsen-learning-modules
- Quality and Safety Education for Nurses Institute. (n.d.-c). QSEN competencies. www.qsen.org/competencies/pre-licensure-ksas
- Ronquillo C., Currie L. M., & Rodney P. (2016). The evolution of data-information-knowledge-wisdom in nursing informatics. Advances in Nursing Science, 39(1), E1-E18. http://dx.doi.org/10.1097/ANS.0000000000000107
- Rowley J. (2007). The wisdom hierarchy: Representations of the DIKW hierarchy. Journal of Information Science, 33(2), 163. https://doi.org/10.1177/0165551506070706
- Rutherford M. (2008). Standardized nursing language: What does it mean for nursing practice? Online Journal of Issues in Nursing, 13(1), 1-12. https://ojin.nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/Health-IT/StandardizedNursingLanguage.html
- Skiba D. (2007). Faculty 2.0: Flipping the novice to expert continuum. Nursing Education Perspectives, 28(6), 342-344. ProQuest Nursing & Allied Health Source Database [Document ID: 1401240241].
- Skrocki M. (2013). Standardization needs for effective interoperability. Transactions of the International Conference on Health Information Technology Advancement, 2(1), 76-83. https://scholarworks.wmich.edu/cgi/viewcontent.cgi?article=1039&context=ichita_transactions
- Snyder-Halpern R., Corcoran-Perry S., & Narayan S. (2001). Developing clinical practice environments supporting the knowledge work of nurses. Computers in Nursing, 19(1), 17-26.
- Technology Informatics Guiding Education Reform. (2007). Evidence and informatics transforming nursing: 3-Year action steps toward a 10-year vision. www.tigersummit.com/uploads/TIGERInitiative_Report2007_Color.pdf
- Thede L., & Schwiran P. (2011). Informatics: The standardized nursing terminologies: A national survey of nurses' experiences and attitudes-Survey I. Online Journal of Issues in Nursing, 16(2). http://ojin.nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/Health-IT/Standardized-Nursing-Terminologies.html
- Topaz M. (2013). Invited editorial: The hitchhiker's guide to nursing informatics theory: Using the data-knowledge-information-wisdom framework to guide informatics research. Online Journal of Nursing Informatics, 17(3). https://cmapspublic2.ihmc.us/rid=1TM7H9MW0-1BC81HG-46V/The_Hitchhiker_s_Guide_to_nursing_inform.pdf
- Westra B., Latimer G., Matney S., Park J., Sensmeier J., Simpson R., Swanson M. J., Warren J. J., & Delaney C. (2015). A national action plan for sharable and comparable nursing data to support practice and translational research for transforming health care. Journal of the American Medical Informatics Association, 22(3), 600-607. https://doi.org/10.1093/jamia/ocu011
- Whitman-Price R., Kennedy L., & Godwin C. (2012). Use of personal phones by senior nursing students to access health care information during clinical education: Staff nurses' and students' perceptions. Journal of Nursing Education, 51(11), 642-646. http://dx.doi.org/10.3928/01484834-20120914-04