Objectives ⬇
- Describe the common components of an electronic health record.
- Assess the benefits of implementing an electronic health record.
- Explore the ownership of an electronic health record.
- Evaluate the flexibility of the electronic health record in meeting the needs of clinicians and patients.
- Examine the impact on patient outcomes when social determinants of health are included in the electronic health record.
Key Terms ⬆ ⬇
Introduction ⬆ ⬇
The significance of electronic health records (EHRs) to nursing cannot be overestimated. Although EHRs on the surface suggest a simple automation of clinical documentation, in fact their implications are broad, ranging from the ways in which care is delivered, to the types of interactions nurses have with patients in conjunction with the use of technology, to the research surrounding EHRs that will inform nursing practice for tomorrow. Although EHR standards are evolving and barriers to adoption remain, the collective work has a positive momentum that will benefit clinicians and patients alike.
A basic knowledge of EHRs and nursing informatics is now considered by many to be an entry-level nursing competency. Various nursing work groups have delineated nursing informatics competencies from entry level to nursing informatics specialists, and other groups have identified competencies specific to the EHR. The American Health Information Management Association (AHIMA) collaborated with the Health Professions Network and the Employment and Training Administration to create a graphic depiction of competencies necessary for EHR interaction. The Health Information Management Competency model is divided into six levels: personal effectiveness competencies, academic competencies, workplace competencies, industry-wide technical competencies, industry-sector technical competencies, and a management competencies level shared with occupation-specific requirements. The Health Information Management Competency model can be viewed at www.careeronestop.org/competencymodel/competency-models/electronic-health-records.aspx. Hovering over each block in the model provides a definition of each of the competencies covered by the model. For example, the industry-sector technical competencies section includes health information literacy and skills, health informatics skills using the EHR, privacy and confidentiality of health information, and health information/data technical security. The drive to adopt EHRs was underscored with the passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009. It is essential that EHR competency be developed if nurses are to participate fully in the changing world of healthcare information technology.
This chapter has four goals. First, it describes the common components of an EHR. Second, it reviews the benefits of using an EHR. Third, it provides an overview of successful ownership of an EHR, including nursing's role in promoting the safe adoption of EHRs in day-to-day practice. Fourth, it discusses the flexibility of an EHR in meeting the needs of both clinicians and patients and emphasizes the need for fully interoperable EHRs and clinical information systems (CISs).
Setting the Stage ⬆ ⬇
The U.S. healthcare system faces the enormous challenge of improving quality of care while simultaneously controlling costs. EHRs were proposed as one solution to achieve this goal (Institute of Medicine [IOM], 2001). In January 2004, President George W. Bush raised the profile of EHRs in his State of the Union Address by outlining a plan to ensure that most Americans have an EHR by 2014. He stated that “by computerizing health records, we can avoid dangerous medical mistakes, reduce costs and improve care” (Bush, 2004). This proclamation generated an increased demand for understanding EHRs and promoting their adoption, but relatively few healthcare organizations were motivated at that time to pursue adoption of EHRs. Congress passed the American Recovery and Reinvestment Act (ARRA) of 2009. This legislation included the HITECH Act, which specifically sought to incentivize health organizations and providers to become meaningful users of EHRs. These incentives came in the form of increased reimbursement rates from the Centers for Medicare and Medicaid Services (CMS); ultimately, the HITECH Act resulted in payment of a penalty by any healthcare organization that had not adopted an EHR by January 2015. The Healthcare Information and Management Systems Society (HIMSS) has been tracking EHR adoption since 2005 through its Stage 7 validation and in 2013 reported that most U.S. healthcare organizations (77%) were in Stage 3, reflecting implementation of only the basic EHR components of laboratory, radiology, and pharmacy ancillaries; a clinical data repository, including a controlled medical vocabulary; and simple nursing documentation and clinical decision support (HIMSS, n.d.-a, 2014, 2017). Higher stages of the EHR adoption model include more sophisticated use of clinical decision support systems and medication administration tools, with HIMSS Stage 7-the highest level-consisting of EHRs that have data sharing and warehousing capabilities and are completely interfaced with emergency and outpatient facilities (Burkey, 2015; HIMSS, n.d.-c, 2017). Real progress is being made on the adoption of more robust EHRs. HIMSS (n.d.-c) reports that 1,313 hospitals in the United States have achieved Stage 6, with full physician documentation, a robust clinical decision support system, and electronic access to medical images. Burkey (2015) reported that, to date, over 200 hospitals have achieved Stage 7 and are totally paperless and that more organizations reach this goal every day. Overall, 96% of U.S. hospitals and 78% of physicians' offices have adopted an EHR (Office of the National Coordinator for Health Information Technology, n.d.).
Components of Electronic Health Records ⬆ ⬇
Overview
Before enactment of the ARRA, several variants of EHRs existed, each with its own terminology and each developed with a different audience in mind. The sources of these records included, for example, the federal government (HIMSS, n.d.-a, 2017; IOM, 2003) and the National Institutes of Health (2006). The ARRA included an explicit requirement for providers and hospitals to use a certified EHR that meets a set of standard functional definitions to be eligible for an increased reimbursement incentive. Standards, standardized functions, and standard terminology requirements are important considerations so that information can be easily shared among providers. Initially, the U.S. Department of Health and Human Services (HHS) granted two organizations the authority to accredit EHRs: the Drummond Group and the Certification Commission for Healthcare Information Technology. These bodies are authorized to test and certify EHR vendors against the standards and test procedures developed by the National Institute of Standards and Technology (NIST) and endorsed by the Office of the National Coordinator for Health Information Technology (ONC) for EHRs. The number of certification bodies recognized by the ONC changes over time; for current information, see www.healthit.gov/topic/certification-ehrs/about-onc-health-it-certification-program.
The initial NIST test procedure included 45 certification criteria, ranging from the basic ability to record patient demographics, document vital signs, and maintain an up-to-date problem list to more complex functions, such as electronic exchange of clinical information and patient summary records (NIST, 2010a). Box 14-1 lists the 45 certification criteria outlined by NIST in 2010. These criteria have been updated several times since 2010, with the 2015 version developed after going out for public comment (ONC, 2023). In 2020, the changes that are now reflected in the revised criteria resulted from the implementation of the 21st Century Cures Act (Federal Register, 2020a, 2020b). Each iteration of certification criteria and testing procedures seeks to make the EHR more robust, interoperable, and functional to meet the needs of patients and users.
| Box 14-1 EHR Certification Criteria |
|---|
Criteria # | Certification Criteria |
|---|
§170.302 (a) | Drug-drug, drug-allergy interaction checks | §170.302 (b) | Drug formulary checks | §170.302 (c) | Maintain up-to-date problem list | §170.302 (d) | Maintain active medication list | §170.302 (e) | Maintain active medication allergy list | §170.302 (f)(1) | Vital signs | §170.302 (f)(2) | Calculate body mass index | §170.302 (f)(3) | Plot and display growth charts | §170.302 (g) | Smoking status | §170.302 (h) | Incorporate laboratory test results | §170.302 (i) | Generate patient lists | §170.302 (j) | Medication reconciliation | §170.302 (k) | Submission to immunization registries | §170.302 (l) | Public health surveillance | §170.302 (m) | Patient-specific education resources | §170.302 (n) | Automated measure calculation | §170.302 (o) | Access control | §170.302 (p) | Emergency access | §170.302 (q) | Automatic log-off | §170.302 (r) | Audit log | §170.302 (s) | Integrity | §170.302 (t) | Authentication | §170.302 (u) | General encryption | §170.302 (v) | Encryption when exchanging electronic health information | §170.302 (w) | Accounting of disclosures (optional) | §170.304 (a) | Computerized provider order entry | §170.304 (b) | Electronic prescribing | §170.304 (c) | Record demographics | §170.304 (d) | Patient reminders | §170.304 (e) | Clinical decision support | §170.304 (f) | Electronic copy of health information | §170.304 (g) | Timely access | §170.304 (h) | Clinical summaries | §170.304 (i) | Exchange clinical information and patient summary record | §170.304 (j) | Calculate and submit clinical quality measures | §170.306 (a) | Computerized provider order entry | §170.306 (b) | Record demographics | §170.306 (c) | Clinical decision support | §170.306 (d)(1) | Electronic copy of health information | §170.306 (d)(2) | Electronic copy of health information Note: For discharge summary | §170.306 (e) | Electronic copy of discharge instructions | §170.306 (f) | Exchange clinical information and patient summary record | §170.306 (g) | Reportable lab results | §170.306 (h) | Advance directives | §170.306 (i) | Calculate and submit clinical quality measures |
It is important to see the criteria first established by the ONC in 2010. In 2015, the new requirements expanded from 45 to 60 criteria organized into eight certification criteria categories (ONC, 2015). The categories follow: |
- Clinical Processes
- Care Coordination
- Clinical Quality Measurement
- Privacy and Security
- Patient Engagement
- Public Health
- Health IT Design and Performance
- Electronic Exchange
According to the Federal Register (2020a), the 21st Century Cures Act changed the 2015 criteria. This final rule by the ONC updated the 2015 criteria by removing several certification criteria. This final rule implements certain provisions of the 21st Century Cures Act, including the following: Conditions and Maintenance of Certification requirements for [health IT] developers under the ONC Health IT Certification Program, the voluntary certification of health IT for use by pediatric health care providers, and reasonable and necessary activities that do not constitute information blocking. (Federal Register, 2020b, para. 1) It also updated some of the “certification criteria to reflect standard and implementation specification updates. In consideration of public comments, the final rule adds only two new technical certification criteria and two new attestation-structured privacy and security certification criteria” (Federal Register, 2020a, para. 8). Reproduced from: National Institute of Standards and Technology. (2010b). Meaningful use test method: Approved test procedures version 1.0. www.nist.gov/news-events/news/2010/08/nist-publishes-approved-testing-procedures-electronic-health-records |
Despite the points articulated in the ARRA, the IOM definition of an EHR also remains a valid reference point. This definition is useful because it has distilled all the possible features of an EHR into eight essential components with an emphasis on functions that promote patient safety-a universal denominator that everyone in health care can accept. The eight components are (1) health information and data, (2) results management, (3) order entry management, (4) decision support, (5) electronic communication and connectivity, (6) patient support, (7) administrative processes, and (8) reporting and population health management (IOM, 2003). These initial core components, as well as more recent modifications, described by the Health Resources and Services Administration (Green, 2023) and the components of a comprehensive EHR identified by the ONC (Charles et al., 2015) are described in more detail here. With the exception of EHR infrastructure functions, such as security and privacy management, controlled medical vocabularies, and interoperability standards, the 45 initial NIST standards easily map onto the IOM categories.
Health Information and Data
Health information and data comprise the patient data required to make sound clinical decisions, including demographics, medical and nursing diagnoses, medication lists, allergies, and test results (IOM, 2003). This component of the EHR also includes care management data regarding details of patient visits and interactions with patients, medication reconciliation, consents, and directives (Green, 2023). A comprehensive EHR will also contain nursing assessments and problem lists (Charles et al., 2015). According to the ONC (2019a), the EHR is a digital, or electronic, record that can provide comprehensive health information about patients. The EHR systems are designed to disseminate patient information to healthcare providers, laboratories, imaging centers, pharmacies, clinics, and other organizations involved in the patient's care.
Results Management
Results management is the ability to manage results of all types electronically, including both current and historical laboratory and radiology procedure reports (IOM, 2003).
Order Entry Management
Order entry management is the ability of a clinician to enter medication and other care orders, including laboratory, microbiology, pathology, radiology, nursing, and supply orders; ancillary services; and consultations, directly into a computer (IOM, 2003). A comprehensive EHR will also contain nursing orders (Charles et al., 2015).
Decision Support
Decision support entails the use of computer reminders and alerts to improve the diagnosis and care of a patient, including screening for correct drug selection and dosing; screening for medication interactions with other medications; preventive health reminders in such areas as vaccinations, health risk screening, and detection; and clinical guidelines for patient disease treatment (IOM, 2003). The National Academy of Medicine (2017) reflected that the core potential of health information technology is its promise to revolutionize the data, information, knowledge, and wisdom (DIKW) process and alleviate the challenges related to clinical decision support. It believed that health information technology must be able to “ameliorate the burden that exponentially expanding clinical knowledge as well as care and choice complexity place on the finite time and attention of clinicians, patients, and every other member of the care team” (p. 1). Incorporating decision support into the EHR is crucial for the delivery of the right data, information, and knowledge to healthcare providers to offer the best support for advocated or recommended clinical decisions. Therefore, the EHR must consistently provide the best available data, information, and knowledge in the context of the patient's needs that can be applied to the patient's healthcare goals. Healthcare providers must be able to access the right data and information at the right time and in the proper format to facilitate their decision and care processes to optimize patient care and outcomes.
Electronic Communication and Connectivity
Electronic communication and connectivity include the online communication among healthcare team members and their care partners and with their patients, which includes email; web messaging; and an integrated health record within and across settings, institutions, and telemedicine (IOM, 2003). This component has been expanded to include the interfaces and interoperability required to exchange health information with other providers, laboratories, pharmacies (i.e., e-prescribing), patients, and government disease registries (Green, 2023). The ONC (2019a) believes that the EHR interfacing has the potential to reduce the fragmentation of care by enhancing care coordination.
Patient Support
Patient support encompasses patient education and self-monitoring tools, including interactive computer-based patient education, home telemonitoring, and telehealth systems (IOM, 2003).
Administrative Processes
Administrative processes are activities carried out by the electronic scheduling, billing, and claims management systems, including electronic scheduling for inpatient and outpatient visits and procedures, electronic insurance eligibility validation, claim authorization and prior approval, identification of possible research study participants, and drug recall support (IOM, 2003).
Reporting and Population Health Management
Reporting and population health management are the data collection tools that support public and private reporting requirements, including data represented in a standardized terminology and machine-readable format (IOM, 2003).
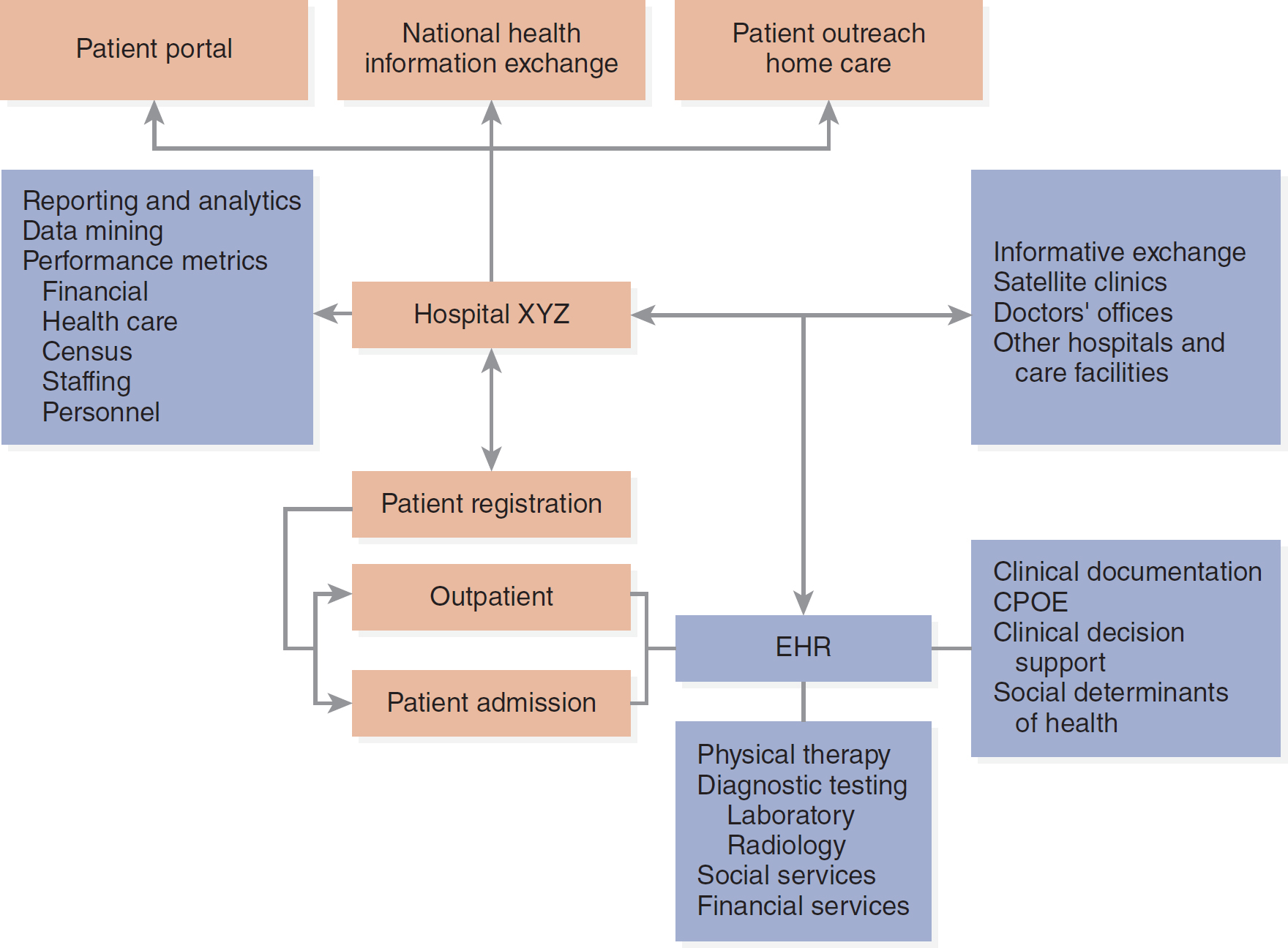
NIST has not provided an exhaustive list of all possible features and functions of an EHR. Consequently, vendors' EHR systems combine different components in their offerings, and often a single set of EHR components may not meet the needs of all clinicians and patient populations. For example, a pediatric setting may demand functions for immunization management, growth tracking, and more robust order entry features that include weight-based dosing (Spooner & Council on Clinical Information Technology, 2007). These types of features may not be provided by all EHR systems, and it is important to consider EHR certification to be a minimum standard. See Figure 14-1 for a graphic depiction of leveraging the EHR.
Figure 14-1 Leveraging the EHR
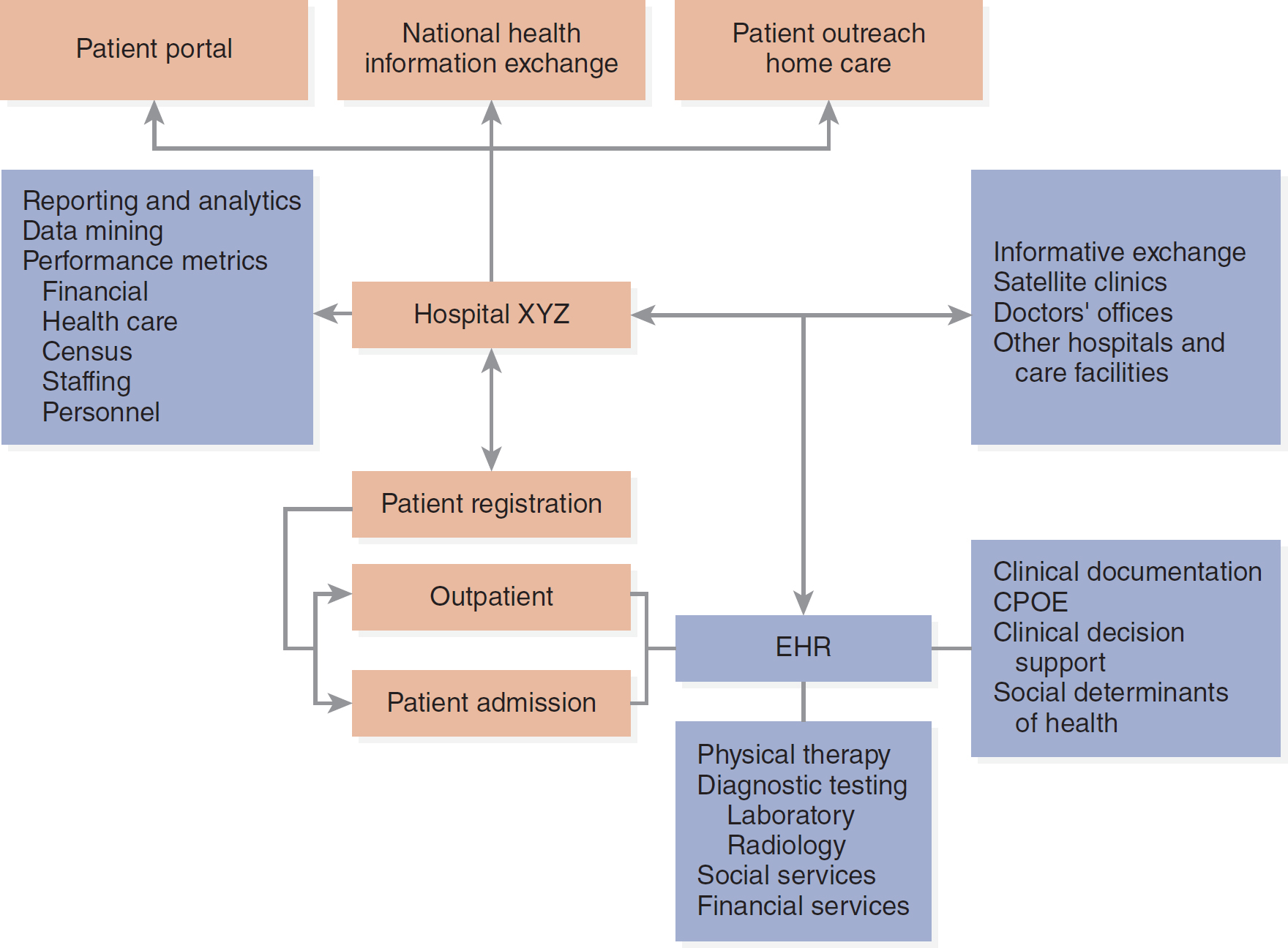
A flowchart depicts the integration of components of electronic health record.
The patient portal, National Health Information Exchange, and patient outreach home care converge to form Hospital X Y Z. Hospital X Y Z features reporting and analytics, data mining, performance metrics involving financial, healthcare, census, staffing, and personnel, informative exchange, satellite clinics, doctors' offices, other hospitals, and care facilities. Hospital X Y Z further leads to patient registration, including outpatient and patient admission. E H R components within the system include clinical documentation, computerized physician order entry, clinical decision support, social determinants of health, physical therapy, diagnostic testing, laboratory, radiology, social services, and financial services.
Courtesy of Dr. Dee McGonigle.
Another group that focuses on EHR standards and functionality is Health Level Seven International (HL7). Founded in 1987, “Health Level Seven International (HL7) is a not-for-profit, ANSI-accredited standards developing organization dedicated to providing a comprehensive framework and related standards for the exchange, integration, sharing, and retrieval of electronic health information that supports clinical practice and the management, delivery and evaluation of health services” (HL7 International, n.d., para. 1). This group concentrates on developing the behind-the-scenes programming standards (Level Seven is the application level of the Open Systems Interconnection model) for interfaces to ensure interoperability and connectivity among systems.
Advantages of Electronic Health Records ⬆ ⬇
Measuring the benefits of EHRs can be challenging. Possible methods for estimating EHR benefits include using data supplied by vendors that have been retrieved from their customers' systems, synthesizing and applying studies of overall EHR value, creating logical engineering models of EHR value, summarizing focused studies of elements of EHR value, and conducting and applying information from site visits (ONC, 2017a; Thompson et al., 2007).
Early in their development, the four most-cited benefits of EHRs were (1) increased delivery of guidelines-based care, (2) enhanced capacity to perform surveillance and monitoring for disease conditions, (3) reduction in medication errors, and (4) decreased use of care (Chaudhry et al., 2006; ONC, 2017a). These findings were echoed by two similar literature reviews. The first review, by Dorr et al. (2007), focused on the use of informatics systems for managing patients with chronic illness. They found that the processes of care that were most positively affected were guidelines adherence, visit frequency (i.e., a decrease in emergency department visits), provider documentation, patient treatment adherence, and screening and testing.
The second review, by Shekelle et al. (2006), was a cost-benefit analysis of health information technology, completed by the Agency for Healthcare Research and Quality, that studied the value of an EHR in ambulatory care and pediatric settings, including its overall economic value. Shekelle et al.'s study highlighted the common findings already described but also noted that most of the data available for review came from six leading healthcare organizations in the United States, which underscored the challenge of generalizing these results to the broader healthcare industry. The challenge to generalize results persists in the hospital arena, with fewer than 1% of U.S. hospitals, or eight leading organizations, providing most of the experience with comprehensive EHRs (HIMSS, n.d.-a, n.d.-c, 2017). Finally, the literature reviews cited here indicated that there are a limited number of hypothesis-testing studies of EHRs and even fewer that have reported cost data.
The descriptive studies do have value, however, and should not be hastily dismissed. Although not as rigorous in their design compared to experimental studies, they do describe the advantages of EHRs well and often include useful implementation recommendations learned from practical experience. As identified in these types of reviews, EHR advantages include simple benefits, such as no longer having to interpret poor handwriting and handwritten orders; reduced turnaround time for laboratory results in an emergency department; and decreased time to administration of the first dose of antibiotics in an inpatient nursing unit (Husk & Waxman, 2004; ONC, 2017a). In the ambulatory care setting, improved management of cardiac-related risk factors in patients with diabetes and effective patient notification of medication recalls have been demonstrated to be benefits of the EHR (Jain et al., 2005; Reed & Bernard, 2005). Two other unique advantages that have great potential are the ability to use the EHR and decision support functions to identify patients who qualify for research studies or prescription drug benefits offered by pharmaceutical companies at safety net clinics and hospitals (Embi et al., 2005; Poprock, 2005). Safety net refers to U.S. medical hospitals and clinics that have a mission, legal duty, or obligation to afford health care to individuals irrespective of their ability to pay or health insurance status, thus making all these facilities provide access and care to all the U.S. populations.
The HIMSS Davies Award may be the best resource for combined quantitative and qualitative results of successful EHR implementation. The Davies Award recognizes healthcare organizations that have achieved both excellence in implementation and value from health information technology (HIMSS, n.d.-b; Monegain, 2010). Winners demonstrate a significant avoidance of medication errors, a decrease in medical records expenses, a decrease in adverse drug reactions, and a reduction of duplicate laboratory orders (HIMSS, 2020). There have been qualitative and quantitative evidence of high rates of end user adoption and satisfaction with use of the EHR.
A 2011 study of the effects of EHR adoption on nurse perceptions of quality of care, communication, and patient safety documented that nurses report better care outcomes and fewer concerns with care coordination and patient safety in hospitals with a basic EHR (Kutney-Lee & Kelly, 2011). In this study, nurses perceived that in hospitals with a functioning EHR, there was better communication among staff, especially during patient transfers, and fewer medication errors. Bayliss et al. (2015) demonstrated that an integrated care system utilizing an EHR resulted in fewer hospital readmissions and emergency room visits for over 12,000 seniors with multiple health challenges.
Without an EHR system, any of these benefits would be very difficult and costly to accomplish. Thus, despite limited standards and published studies, there is enough evidence to embrace widespread implementation of the EHR (Halamka, 2006; ONC, 2017a) and certainly enough evidence to warrant further study of the use and benefits of EHRs. Box 14-2 describes some of the specific CIS functions of an EHR.
| Box 14-2 The EHR as a Clinical Information System |
|---|
| Denise Tyler
A CIS is a technology-based system applied at the point of care and designed to support care by providing instant access to information for clinicians. Early CISs, implemented before the advent of EHRs, were limited in scope and provided such information as interpretation of laboratory results or a medication formulary and drug interaction information. With the implementation of EHRs, the goal of many organizations is to expand the scope of the early CISs to become comprehensive systems that provide clinical decision support; an electronic patient record; and, in some instances, professional development and training tools. Benefits of such a comprehensive system include easy access to patient data at the point of care; structured and legible information that can be searched easily and lends itself to data mining and analysis; and improved patient safety, especially the prevention of adverse drug reactions and the identification of health risk factors, such as falls.
|
| Tracking Clinical Outcomes |
|---|
| The ability to measure outcomes can be enhanced or impeded by the way an information system is designed and used. Although many practitioners can paint a very good picture of the patient by using a narrative (free text), employing this mode of expression in a clinical system without the use of a coded entry makes it difficult to analyze the care given or the patient's response. Free-text reporting also leads to inconsistencies of reporting from clinician to clinician and patient information that is fragmented or disorganized. Such inconsistencies can limit the usefulness of patient data to other clinicians and interfere with the ability to create reports from the data for quality assurance and measurement purposes. Moreover, not all clinicians are equally skilled at the free-text form of communication, which yields inconsistent quality of documentation. Integrating standardized nursing terminologies into computerized nursing documentation systems enhances the ability to use the data for reporting and further research.
According to the IOM (2012), “Payers, healthcare delivery organizations and medical product companies should contribute data to research and analytic consortia to support expanded use of care data to generate new insights” (para. 2). Goldsmith (2019) stated that “many health organizations are already taking advantage of technologies such as AI [artificial intelligence] and advanced analytics to gain insights that help them improve clinical treatment processes and outcomes” (para. 1). Clinical analytics are being used to promote medical care outcomes research. The use of a CIS in conjunction with standardized codes for patient clinical issues helps to support the rigorous analysis of clinical data. Outcomes data produced as part of these analyses may include length of stay, mortality, readmissions, and complications. Future goals include the ability to compare data and outcomes across various institutions as a means of developing clinical or best practices guidelines. With the implementation of a comprehensive CIS, similar analyses of nursing outcomes could also be performed and shared. Likewise, such a system could aid nurse administrators in cross-unit comparisons and staffing decisions, especially when coupled with acuity systems data. In addition, clinical analytics can support required data reporting functions, especially those required by accreditation bodies.
|
| Supporting Evidence-Based Practice |
|---|
| Evidence-based practice (EBP) can be thought of as the integration of clinical expertise and best practices based on systematic research to enhance decision-making and improve patient care. References supporting EBP, such as clinical guidelines, are available for review at the click of a mouse or the execution of a few keystrokes. The CIS's prompting capabilities can also reinforce the practice of looking for evidence to support nursing interventions rather than relying on how things have been done historically. This approach enhances processing and understanding of the information and allows the nurse to apply the information to other areas, which increases the knowledge obtained about why certain conditions or responses result in prompts for additional questions or actions.
To incorporate EBP into the practice of clinical nursing, the information needs to be embedded into the computerized documentation system so that it is part of the workflow. The most typical way of embedding this timely information is through clinical practice guidelines. The resulting interventions and clinical outcomes need to be measurable and reportable for further research. The supporting documentation for the EBP must be easily retrievable and meaningful. Links, reminders, and prompts can be used as vehicles for transmission of this information. The format needs to allow for rapid scanning, with the ability to expand the amount of information when more detail is required or desired. Balancing a consistency in formatting with creativity can be difficult but is worth the effort to stimulate an atmosphere for learning.
EBP is supported by translational research, which is an exciting movement that has enormous potential for the sharing and use of EBP. The use of translational research to support EBP may help to close the gap between what is known (i.e., research) and what is done (i.e., practice).
|
| The CIS as a Staff Development Tool |
|---|
| Joy Hilty, a registered nurse from Kaweah Delta, devised a creative way to provide staff development and education without taking staff away from the bedside to a classroom setting. She created pop-up boxes on the opening charting screens for all staff who chart on the computer. These pop-ups vary in color and content and include a short piece of clinical information along with a question. Staff can earn vacations from these pop-ups for as long as 14 days by emailing the correct answer to the question. This medium has provided information, stimulation, and a definite benefit: the vacation. The pop-up box education format has also encouraged staff members to share their answers, thereby creating interaction, knowledge dissemination, and reinforcement of the education provided.
Embedding EBP into nursing documentation can also increase the compliance with Joint Commission core measures, such as providing information on influenza and pneumococcal vaccinations to at-risk patients. In the author's experience at Kaweah Delta, educating staff via classes, flyers, and storyboards was not successful in improving compliance with the documentation of immunization status or offering education on these vaccinations to at-risk patients. Embedding the prompts, information, and related questions into the nursing documentation with a link to the protocol and educational material, however, improved the compliance to 96% for pneumococcal vaccinations and to 95% for influenza vaccinations (Hettinger, 2007). Downing et al. (2019) studied the implementation of a sepsis alert for inpatients using patient-level randomization and leveraging EHR functionality for real-time alerts along with a patient-centered design in a standardized clinical workflow. They found that even though it is realistic to develop sepsis alerts using the EHR, further research is necessary to comprehend how to design these sepsis alerts to actually change healthcare providers' behavior.
As more information is stored electronically, nurse informaticists must translate the technology so that the input and retrieval of information are developed in a manner that is easy for clinicians to learn and use. A highly usable product should decrease errors and improve information entry and retrieval. Nurse informaticists must be able to work with staff and expert users to design systems that meet the needs of the staff who will actually use the systems. Even after the system has been installed, work continues to develop and improve it because as staff members use it, they will be able to suggest changes to improve it. This ongoing revision should result in a system that is mature and meets the needs of the users.
In an ideal world, all clinical documentation would be shared through a national database, in a standard language, to enable evaluation of nursing care, increase the body of evidence, and improve patient outcomes. With minimal effort, the information would be translated into new research that could be analyzed and linked to new evidence that would be intuitively applied to the CIS. Alerts would be meaningful and specific to patient and provider. The steps required of the clinician to find current, reliable information would be almost transparent, and the information would be presented in a personalized manner, based on user preferences stored in the CIS.
|
A more recent description of the benefits of an EHR by the ONC (2022) emphasized that EHRs hold the promise of transforming health care. Specifically, EHRs will lead to the following benefits:
- Better health care by improving all aspects of patient care, including safety, effectiveness, patient-centeredness, communication, education, timeliness, efficiency, and equity
- Better health by encouraging healthier lifestyles in the entire population, including increased physical activity, better nutrition, avoidance of behavioral risks, and wider use of preventative care
- Improved efficiencies and lower healthcare costs by promoting preventative medicine and improved coordination of healthcare services, as well as by reducing waste and redundant tests
- Better clinical decision making by integrating patient information from multiple sources (para. 3)
The ONC (2019a) amended the benefits of an EHR that it had listed in 2014. The ONC reminded us in the update that the EHR provides information whenever and wherever it is needed to improve patient care, increase patient engagement, enhance care coordination, and advance diagnostics and patient outcomes with practice efficiencies and cost savings.
The EHR can be an important source of information on patient vulnerability risks related to social determinants of health (SDOH). SDOH are the economic and social conditions, in relation to their diffusion and distribution, among the population that actually influence individual and group differences and disparities in health status and health outcomes; “they are the conditions of the environment in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks” (Healthy People 2030, n.d., para. 1). SDOH have an effect on our life expectancy, morbidity, and mortality. Paruk (2019) shared that the research has demonstrated that “these factors contribute significantly to health and well-being. For example, average life expectancy is reduced by 15 to 20 years for people living in low-income communities, due to increased risk for stroke, chronic disease and other health concerns” (para. 2). Healthy People 2030 (n.d.) stated that there are five key domains for SDOH: “(1) Economic Stability, (2) Education Access and Quality, (3) Health Care Access and Quality, (4) Neighborhood and Built Environment, and (5) Social and Community Context” (para. 1). The eHealth Initiative (2019) provided examples of SDOH that included safe housing and food markets, access to healthcare services, opportunities for recreation, public safety and exposure to crime, and access to emerging technologies.
To gain access to SDOH data, users must be able to extract data found in unstructured text and diagnosis codes as well as what is collected in the EHR. According to Paruk (2019), Allscripts has “discovered more than 2 million SDoH-related diagnoses in our [Allscripts's] data lake of more than 40 million de-identified patient records. Top diagnoses include disruption of family by separation or divorce, disappearance or death of a family member and unemployment” (para. 7). Rohatgi (2022) advocates for the use of specific screening tools to capture SDOH data rather than teasing the information out of data lakes as described above. “While medical care accounts for approximately 20 percent of healthcare, physical environment, socioeconomic factors, and health-related behaviors, all elements of SDOH account for about 80 percent of outcomes” (para. 1). These insights into patients' circumstances can help nurses advocate for them and transform the healthcare delivery system by tailoring services to meet their needs. If nurses can improve the health of individual patients within the population, they will be able to improve the population's health.
Nurses can gather, analyze, and synthesize data and information from each of the SDOH domains. It is imperative that they determine the priorities they must focus on to improve health status. The CMS (2023) developed an Accountable Health Communities model to identify and attend to the SDOH needs that affect healthcare utilization and costs; the model “addresses a critical gap between clinical care and community services in the current health care delivery system” (para. 1). This model is based on emerging proof that tackling health-related social needs through improved clinical-community relationships can improve health outcomes and decrease costs. According to the CMS (2023), “unmet health-related social needs, such as food insecurity and inadequate or unstable housing, may increase the risk of developing chronic conditions, reduce an individual's ability to manage these conditions, increase health care costs, and lead to avoidable health care utilization” (para. 2). The Accountable Health Communities model is an example of data analytics being used to guide our actions on the data and information that exist at our fingertips. Working collectively with individuals, communities, organizations, the healthcare delivery system, and government agencies, data-driven solutions could be planned, implemented, monitored, and evaluated. If nurses and healthcare professionals can truly act on the data and information to advance health equity, this could restructure social and physical environments to promote better health for everyone.
Standardized Terminology and the EHR ⬆ ⬇
As we inch closer to interoperable EHRs, which provide for seamless health information exchange among providers and healthcare institutions, the need for standardizing terminologies becomes ever clearer. Consider also the trend toward value-based care reimbursements, for which healthcare data are mined “to demonstrate nursing's contributions to improving the cost, quality, and efficiency of care, key elements of the value equation” (Ponte et al., 2016, p. 127). EHR data must be formatted in a machine-readable manner to support interoperable exchange of information and data mining. An important distinction that needs to be made here is the difference between interface terminologies (i.e., North American Nursing Diagnosis Association [NANDA], Nursing Interventions Classification [NIC], and Nursing Outcomes Classification [NOC]) and reference terminologies (i.e., Systematized Nomenclature of Medicine Clinical Terms [SNOMED CT] and Logical Observation Identifiers Names and Codes [LOINC]). It is important to understand the function of the nursing terminologies that interface between nurses' everyday language, used to describe patients and document patient care, and the structured elements of the specific information systems that nurses use. “The mapping of interface terminologies to reference terminologies allows a standard, shared vocabulary to communicate data across settings” (ONC, 2017b, p. 8).
Since the nursing standards support the EHR and nursing practice, the ONC (2017b) assessed the “current state of development and usage within the 12 Standard Nursing Terminologies (SNT) recognized by the American Nurses Association” (p. 4). The ONC conducted a “landscape assessment to better understand the current state and challenges associated with using terminologies and classifications to support nursing practice within health information technology (health IT) solutions” (p. 4). They noted that some health systems found the language in some of the terminologies awkward and difficult to implement, especially when they are moving “to implement an interdisciplinary care plan and other types of clinical documentation” (p. 23).
The various interface terminologies and their subsets are coded in the EHR and typically presented to the user in drop-down menus. Users may also be able to use a search function in the EHR to identify the most appropriate term that represents the patient's condition. The electronic presentation of these terminologies supports clinician workflow and promotes data retrieval and exchange in future use.
HHS has designated the National Library of Medicine as the central coordinating body for clinical terminologies. (See Box 14-3 for descriptions of administrative and reference terminologies used in an EHR.) (See Chapter 6, History and Evolution of Nursing Informatics, for a list of approved nursing terminologies.) In 2018, the American Nurses Association reaffirmed its support for the use of standardized terminologies:
| Box 14-3 Standard EHR Administrative and Reference Terminologies |
|---|
| Administrative (Billing) Terminologies |
|---|
- ICD-10 (International Classification of Diseases, Version 10): Medical diagnosis code set
- CPT (Current Procedural Terminology): Used to code procedures for billing
|
| Clinical Terminologies |
|---|
- SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms): Comprehensive clinical terminology (mapping to this terminology is ongoing, including nursing-orders mapping)
- LOINC (Logical Observation Identifier Names and Codes): Universal codes for laboratory and clinical observations
- RxNorm: Terminology system for drug names, which provides links to drug vocabularies and interaction software
- Unified Medical Language System (UMLS) and the Metathesaurus: Support terminology integration efforts and online searches (not a terminology system)
See the National Library of Medicine's website for more comprehensive information: www.nlm.nih.gov/research/umls/Snomed/nursing_terminology_resources.html. |
The purpose of this position statement is to reaffirm the American Nurses Association's (ANA) support for the use of recognized terminologies supporting nursing practice as valuable representations of nursing practice and to promote the integration of those terminologies into information technology solutions. Standardized terminologies have become a significant vehicle for facilitating interoperability between different concepts, nomenclatures, and information systems. (para. 1)
Because no single model of standardized terminology for health care or nursing can represent all the contributions to the health of a patient, work is ongoing to map terminologies to one another. For example, Kim et al. (2014) studied the degree of similarity between the International Classification for Nursing Practice (ICNP) and the SNOMED CT. Although they identified some areas of overlap, they cautioned that there is still more work to be done to truly represent nursing concepts in the EHR. Ponte et al. (2016) issued a call to action to chief nursing officers (CNOs): “CNOs must begin partnering with and influencing EHR developers and vendors to ensure the EHRs implemented in their organizations capture nursing content using a standardized taxonomy that is evidence based and mapped to SNOMED-CT and LOINC” (p. 127). Ongoing efforts to map nursing problem lists to SNOMED CT are evident in the work of Matney et al. (2012) and on the National Library of Medicine website (www.nlm.nih.gov/research/umls/Snomed/nursing_terminology_resources.html). It is probably safe to say that the number of types and the variability of EHRs are likely to contract and converge as the demand for robust systems to support interoperability expands. Nurse informatics specialists and CNOs participating in the selection and implementation of EHRs must ask a critical question: To what extent are nursing care contributions visible, retrievable, and accurately represented in this EHR?
Ownership of Electronic Health Records ⬆ ⬇
The selection and implementation of an EHR has the potential to affect every member of a healthcare organization. The process of becoming a successful owner of an EHR requires multiple steps and integrating the EHR into the organization's day-to-day operations and long-term vision as well as into clinicians' day-to-day practice. All members of the healthcare organization-from the executive level to the clinician at the point of care-must feel a sense of ownership to make the implementation successful for themselves, their colleagues, and their patients. Successful ownership of an EHR may be defined in part by the level of clinician adoption of the tool, and this section reviews key steps and strategies for the selection, implementation, evaluation, and optimization of an EHR in pursuit of that goal.
The first step of ownership is typically a vendor selection process for a certified, commercially available EHR. Although clinicians, as the primary end users, should drive the project, the assessment should also include the needs and readiness of the executive leadership, information technology, and project management teams. In addition, this pre-acquisition phase should concentrate on understanding the current state of the health information technology industry to identify appropriate questions and the next steps in the selection process (American Organization of Nurse Executives, 2009). These first steps begin to identify organizational risks related to successful implementation and pave the way for initiating a change management process to educate the organization about the future state of delivering health care with an EHR system.
The second step of the selection process is to choose a system based on the organization's current and predicted needs. It is common during this phase to see a demonstration of several vendors' EHR products. Based on the completed needs assessment, the organization should establish key evaluation criteria to compare the different vendors and products. These criteria should include both subjective and objective items that cover such topics as common clinical workflows, decision support, reporting, usability, technical build, and maintenance of the system. Providing the vendor with these guidelines will ensure that the process meets the organization's needs; however, it is also essential to let the vendor demonstrate a proposed future state from its own perspective. This activity is critical to ensuring that the vendor's and the organization's visions are well aligned (Konschak & Shiple, n.d.). It also helps spark dialogue about the possible future state of clinical work at the organization and the change required in obtaining it. Such demonstrations not only enable the organization to compare and contrast the features and functions of different systems but also are a good way to engage the organization's members in being a part of this strategic decision.
Implementation planning should occur concurrently with the selection process, particularly the assessment of the scope of the work, initial sequencing of the EHR components to be implemented, and resources required. However, this step begins in earnest once a vendor and a product have been selected. In addition to further refining the implementation plan, this is the time to identify key metrics by which to measure the EHR's success. An organization may realize numerous benefits from implementing an EHR. It should choose metrics that match its overall strategy and goals in the coming years and may include expected improvements in financial, quality, and clinical outcomes. Commonly used metrics focus on reductions in the number of duplicate laboratory tests through duplicate orders alerting, reductions in the number of adverse drug events through the use of barcode medication administration, meaningful use objectives and measures, and the EHR advantages mentioned earlier in this chapter. To ensure that the desired benefits are realized, it is important to avoid choosing so many that they become meaningless or unobtainable and to carefully and practically define those that are selected, measure before and after the implementation, and assign accountability to a member of the organization to ensure that the work is completed.
End user adoption of the EHR is also essential to realizing its benefits. Clinicians must be engaged to use the EHR successfully in their practice and daily workflows so that data may be captured to drive the decision support that underlies so many of the advantages and metrics described. To promote adoption, a change management plan must be developed in conjunction with the EHR implementation plan. The most effective change management plans offer end users several exposures to the system and relevant workflows in advance of its use and continue through the go-live and post-live time periods. Successful pre-live strategies include involving end users as subject matter experts to validate the EHR workflow design and content build, hosting end user usability testing sessions, shadowing end users in their current daily work in parallel with the new system, and conducting formal training activities. The goal of these pre-live activities is not only to ensure that the EHR implementation will meet end users' needs but also to assess the effect of the new EHR on current workflow and processes. The larger the effect, the more change management is required above and beyond system training. For example, simulation laboratory experiences may be offered to more thoroughly rehearse a significant workflow change; executive leaders may need to convey their support and expectations of clinicians about a new way of working; and, generally, more anticipatory guidance is required to communicate to those affected by the changes.
Training may be delivered in a variety of media. Often, a combination of approaches works best, including classroom time; electronic learning; independent exercises; and peer-to-peer, at-the-elbow support. Training must be workflow based and reflect real clinical processes. It must be planned and budgeted for through the post-live period to ensure that competency with the system is assessed at the go-live point and any necessary retraining or reinforcements are made in the 30 to 60 days post-live. This process not only promotes reliability and safe use of the system as it was designed but also can have a positive effect on end users' morale; users will feel that they are being supported beyond the initial go-live period and have an opportunity to move from basic skills to advanced proficiency with the system.
Finally, the implementation plan should account for the long-term optimization of the EHR. This step is commonly overlooked and often results in benefits falling short of expectations because the resources are not available to realize them permanently. It also often means the difference between end users of EHRs merely surviving the change versus becoming savvy about how to adopt the EHR as another powerful clinical tool, much as clinicians have embraced such technologies as the stethoscope (ONC, 2017a). Optimization activities of the EHR should be considered a routine part of the organization's operations and resourced accordingly and should emphasize the continued involvement of clinician users to identify ways that the EHR can enable the organization to achieve its overall mission. Many organizations start implementations of EHRs with the goal of transforming their care delivery and operations. An endeavor that differs from simply automating a previously manual or fragmented process, transformation often includes steps to improve the process to realize better patient care outcomes or added efficiency. Although some transformation is experienced with the initial use of the system, most of this work is done after implementation and relies on widespread clinician adoption of the EHR. As such, it makes optimization a critical component to successful ownership of an EHR.
Flexibility and Expandability ⬆ ⬇
Health care is as unique as the patients themselves. It is delivered in a variety of settings, for a variety of reasons, over the course of a patient's lifetime. In addition, patients rarely receive all their care from one healthcare organization; indeed, choice is a cornerstone of the U.S. healthcare system. An EHR must be flexible and expandable to meet the needs of patients and caregivers in all these settings, despite the challenges.
At a very basic level, there is as yet no EHR system available that can provide all functions for all specialties to such a degree that all clinicians would successfully adopt it. Consider oncology as an example. Most systems do not yet provide the advanced ordering features required for the complex treatment planning undertaken in this field. An oncologist could use a general system, but they would not find as many benefits without additional features for chemotherapy ordering, lifetime cumulative dose tracking, or the ability to adjust a treatment day schedule and recalculate a schedule for the remaining days of the plan. Some EHRs do a good job of supporting the work of nursing staff and physicians but are not as supportive of the work of clinicians, such as dieticians, physical and occupational therapists, and other healthcare personnel. These systems will continue to evolve and support interprofessional collaboration as more healthcare professionals are exposed to the power of these systems to support their work and become better able to articulate their specific needs.
Conditions are improving every day at both vendor and healthcare organizations alike. Some improvements were recently fueled by ARRA incentives (see Box 14-4).
| Box 14-4 Cloudy EHRs |
|---|
| A paradigm shift from healthcare facility-owned, machine-based computing to off-site, vendor-owned cloud computing with web browser-based, log-on-accessible data, software, and hardware could link systems together and reduce costs. Hospitals with shrinking budgets and extreme IT needs are exploring the successes in this area achieved in other industries, such as Amazon's S3. As providers strive to implement potent EHRs, they are looking for cloud-based models that offer the necessary functionality without having to assume the burden associated with all the hardware, software, application, and storage issues. However, in the face of the HITECH Act and its associated penalties, how can nurses and healthcare professionals overcome the challenges to realize the benefits of this approach? Cloud computing has both advantages and disadvantages, and while healthcare providers explore this new paradigm, they must relinquish control as they continue to strive to maintain security. The vendors that are responsible for developing and maintaining this new environment are also facing challenges originating from both legislatures and healthcare providers. As the vendors and healthcare providers work together to improve the implementation and adoption of the cloud-based EHR, the sky is the limit! |
ARRA has also set the expectation that despite the large number of settings in which a patient may receive care, a minimum set of data from those records must flow, or “interoperate,” among each setting and the unique EHR systems used in those settings. Today, interoperability exists through what is called a Continuity of Care Document (CCD). This data set includes information about a patient's health care, such as patient demographics, medications, allergies, and problems. The document is formatted according to HL7 standards and is both machine and human readable.
Despite this positive step forward, financial and patient privacy hurdles remain to be overcome to achieve an expansive EHR. Most health care is delivered by small community practices and hospitals, many of which do not have the financial or technical resources to implement robust, interoperable EHRs. HHS recently loosened regulations so that physicians may now be able to receive healthcare information technology software, hardware, and implementation services from hospitals to alleviate the financial burden placed on individual providers and foster more widespread adoption of the EHR. Interoperable EHRs facilitate data sharing to help “coordinate care, reduce costs, manage population health, improve patient experience and outcomes, and address health equity challenges” (Juhn & Galvez, 2022, p. 426).
Accountable Care Organizations and the EHR ⬆ ⬇
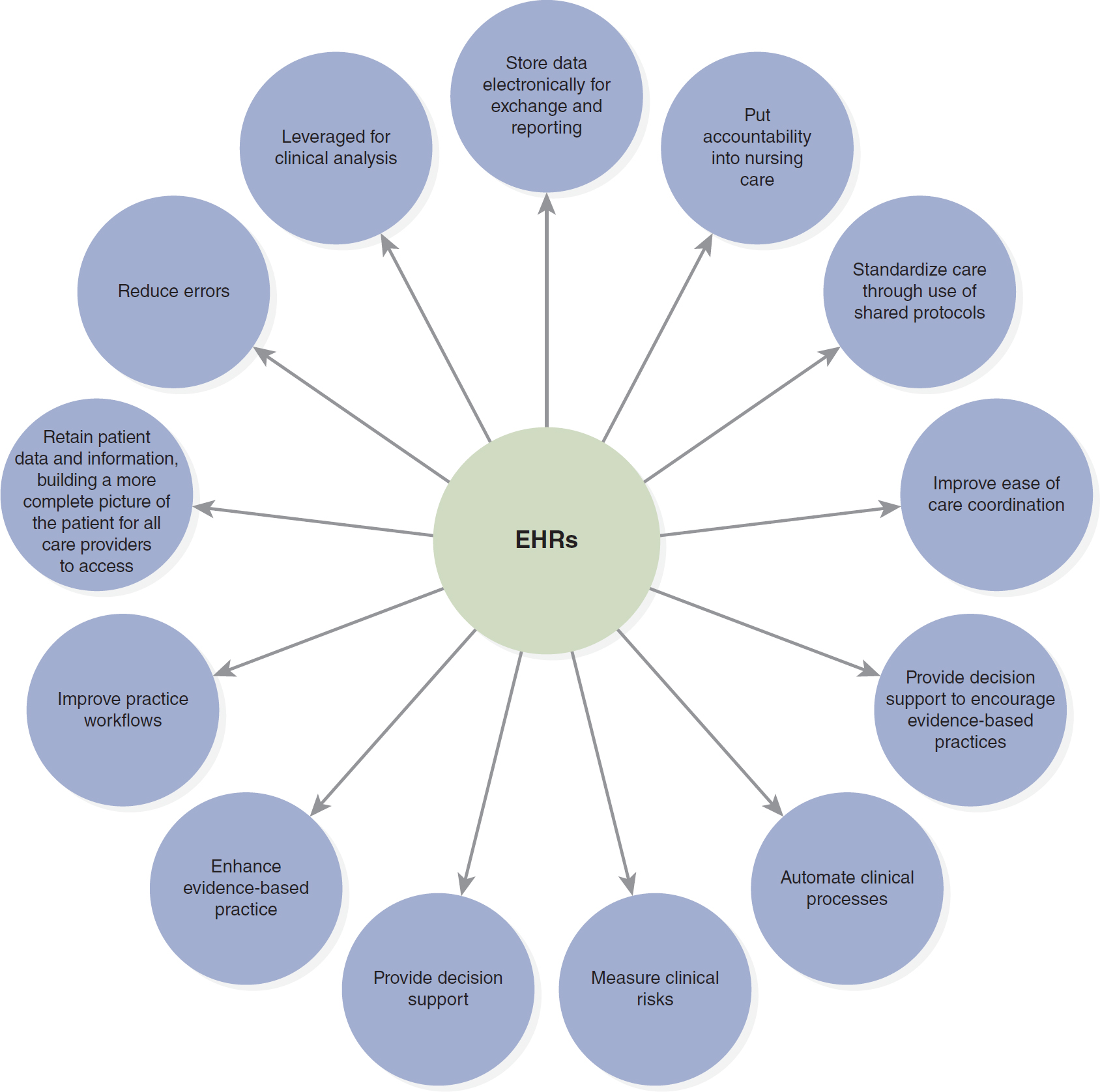
EHRs with data-sharing capabilities are central to the support of Accountable Care Organizations (ACOs), a payment incentive program established by the CMS (2022). As discussed elsewhere, this program of shared medical and financial responsibility is designed to provide quality, coordinated care while limiting costs. Some of the core information technology requirements for an ACO are EHRs, HIEs, care management systems, and analytics and reporting systems (Welter, 2015; Figure 14-2). A robust EHR can support many of these functions:
Figure 14-2 How EHRs Support Accountable Care
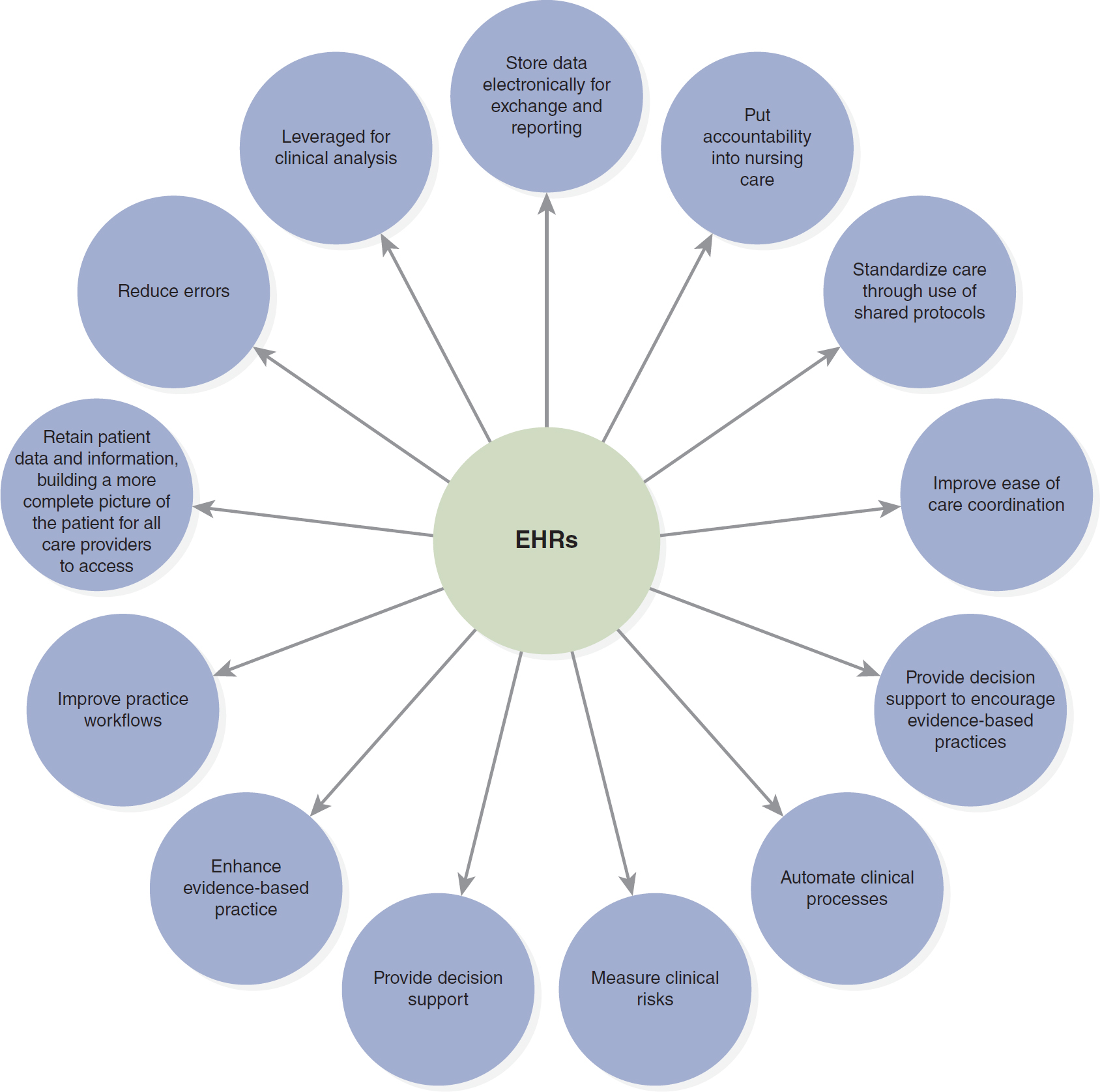
An illustration depicts the ways in which electronic health records facilitate accountable care.
The ways include the following. Store data electronically for exchange and reporting; Put accountability into nursing care; Standardize care through use of shared protocols; Improve ease of care coordination; Provide decision support to encourage evidence-based practices; Automate clinical processes; Measure clinical risks; Provide decision support; Enhance evidence-based practice; Improve practice workflows; Retain patient data and information, building a more complete picture of the patient for all care providers to access; Reduce errors; and Leveraged for clinical analysis.
Data from: ECG Consultants. (2015). The use of technology in healthcare reform: IT considerations for accountable care. www.ecgmc.com/thought-leadership/articles/the-use-of-technology-in-healthcare-reform-it-considerations-for-accountable-care.
EHR solutions that are interoperable across organizations can significantly reduce the cost and complication of IT infrastructure by creating full EHR visibility between providers. This shared visibility reduces or eliminates the need to participate in HIEs or invest in solutions to integrate data across different EHR platforms. Many EHRs also can serve as a program's care management system, eliminating the need for a separate system to document care management efforts and help care teams engage with patients. (Welter, 2015, para. 5)
The Future ⬆ ⬇
Despite the challenges, the future of EHRs is an exciting one for patients and clinicians alike. Benefits may be realized by implementing stand-alone EHRs, as described here, but the more significant transformation will come as interoperability is realized between systems.
The U.S. population depends on health IT to “securely, efficiently, and effectively share electronic health information with patient consent to achieve better care, smarter spending and healthier people” (ONC, 2019b, para. 1). The barriers that must be eliminated are the lack of confidence and trust in the healthcare delivery system, lack of standardized health information, payment and reimbursement issues, and the fact that privacy laws are not standard and can lead to misinterpretation (ONC, 2019b, para. 2). Patients and healthcare providers must continue to fight to overcome the barriers to interoperability because it has the potential to truly transform our healthcare delivery system “from a static one to a learning health system that improves individual, community and population health” (ONC, 2019b, para. 1).
The future also holds tremendous potential for EHR features and functions that will include not only more sophisticated decision support and clinical reporting capacity but also improved support for patients and all healthcare professionals; improved biomedical device integration, ease of use, and intuitiveness; and access through more hardware platforms (see the Applications: Enhancing the EHR box).
Implementation of robust and interoperable EHRs is becoming more commonplace. As more organizations adopt EHRs, broader dissemination of implementation best practices will be facilitated, with the hope of further shortening the time required to take advantage of advanced EHR features.
| Applications: Enhancing the EHR |
|---|
| Artificial Intelligence (AI) |
|---|
| Siwicki (2019) reported on Vanderbilt's AI-powered EHR voice assistant. This “VEVA tool has helped improve caregiver productivity and efficiency” (para. 1). Healthcare providers can interact with the EHR using their voice through natural speech recognition. Using AI is valued because it saves time by decreasing the number of clicks per query. |
| Patient Engagement |
|---|
| The ONC (2023) stated that we should realize the opportunity to engage patients in their health and care by using and expanding EHR patient portals. The patient portals have the ability to streamline and simplify clinical workflows while improving patient engagement by meeting patients' needs. You could provide the ability to schedule an appointment or reorder prescription refills, thereby drawing your patients to the EHR portal. |
| Blockchain |
|---|
| Carfagno (2018) reminded us of the fragmented medical records in health care across multiple providers and how healthcare professionals could miss important patient information. Blockchain technology is a secure technology that could cure this transactional inefficiency and bring all these pieces of information concerning a patient together so that all the records are in sync all the time. Blockchain is being implemented in the Mayo Clinic EHR. Because blockchain technologies enhance EHRs, they can streamline processes, such as associating or connecting patients with their EHR information to activate insurance reimbursement payments related to a specific disease process without having to reverify the diagnosis or file a claim. This process could also expedite the filling of a prescription because all the information would be available, including whether this drug is the best drug, the insurance benefit related to what the company will cover, and even so far as to make sure that the pharmacy is able to provide the patient with the specific drug that was ordered. As an example of one transactional inefficiency that could be addressed through blockchain technology, think of insurance, a resource-intensive area. With blockchain technology, the physician's office staff would not need to know every insurance plan's benefits or make numerous calls to find out, and the patient would not have to play the waiting game to see whether the drug is approved and available.
|
In the future, we can expect to see more enhanced EHRs housed in the cloud, usable patient portals as we move toward more patient-centered health care, the integration of wearables and data into the EHR, the expansion of telemedicine applications for rural patients and those with chronic illnesses, precision medicine advances supported by data analytics, integration of both care and wellness plans, and better consumer engagement, making the care plan a living document (Sterrett et al., 2022).
Summary ⬆ ⬇
It is an important time for health care and technology. EHRs are evolving to include SDOH, AI, blockchain, and patient engagement strategies. EHRs will remain central to shaping the future of health care. In an ideal world, all nurses, from entry-level personnel to executives, would have a basic competency in nursing informatics, which would enable them to participate fully in shaping the future use of technology in the practice at a national level and wherever care is delivered. Such initiatives as Technology Informatics Guiding Education Reform (TIGER) and the important nursing terminology work are imperative for better integration and, ultimately, more visibility of nursing contributions to health care (HIMSS, n.d.-d).
| Thought-Provoking Questions |
|---|
- What are the implications for nursing education in relation to preparing nursing students to leverage the EHR in caring for patients, communicating with other healthcare professionals, decision-making, and research?
- What are the ethical considerations related to interoperability and a shared EHR?
- What are the SDOH? Describe in detail the areas of the EHR where the SDOH would be captured. In your description, make sure to detail the data and information. State whether the data would be structured or unstructured and how meaningful SDOH information could be extracted.
- You are asked about a diagnosis with which you are unfamiliar. Where would you start looking for information? How would you determine the validity of the information?
- Think about the documentation and knowledge management functions of your specialty. If you had the opportunity to create a wish list, what would you include in an EHR to support your work?
- Reflect on EHRs. Describe in detail how an EHR engages healthcare providers. How can it engage a patient? Provide a comprehensive rationale for each way you determine you could use the EHR to engage your patient.
|
References ⬆
- American Nurses Association. (2018, April 19). Inclusion of recognized terminologies supporting nursing practice within electronic health records and other health information technology solutions. www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/Inclusion-of-Recognized-Terminologies-Supporting-Nursing-Practice-within-Electronic-Health-Records
- American Organization of Nurse Executives. (2009). AONE guiding principles for the nurse executive to enhance clinical outcomes by leveraging technology.www.aonl.org/sites/default/files/aone/Leveraging-Technology.pdf
- Bayliss E. A., Ellis J. L., Shoup J. A., Chan Z., McQuillan D. B., & Steiner J. F. (2015). Effect of continuity of care on hospital utilization for seniors with multiple medical conditions in an integrated health care system. Annals of Family Medicine, 13(2), 123-129. http://dx.doi.org/10.1370/afm.1739
- Burkey A. (2015, March 9). 7 tips for EMR success from Stage 7 hospitals. Healthcare IT News. www.healthcareitnews.com/news/7-tips-emr-success-stage-7-hospitals
- Bush G. W. (2004, January 20). Text of President Bush's 2004 State of the Union Address. Washington Post. www.washingtonpost.com/wp-srv/politics/transcripts/bushtext_012004.html
- Centers for Medicare and Medicaid Services. (2022). Accountable Care Organizations (ACOs): General information. www.cms.gov/priorities/innovation/innovation-models/aco
- Centers for Medicare and Medicaid Services. (2023). Accountable health communities model. https://innovation.cms.gov/innovation-models/ahcm
- Charles D., Gabriel M., & Searcy T. (2015, April). Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008-2014. Office of the National Coordinator for Health Information Technology. www.healthit.gov/sites/default/files/data-brief/2014HospitalAdoptionDataBrief.pdf
- Chaudhry B., Wang J., Wu S., Maglione M., Mojica W., Roth E., Morton S. C., & Shekelle P. (2006). Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine, 144(10), E-12-E-22. http://cs.oswego.edu/~bichinda/isc471-hci571/impactofHIT.pdf
- Dorr D., Bonner L. M., Cohen A. N., Shoai R. S., Perrin R., Chaney E., & Young A. (2007). Informatics systems to promote improved care for chronic illness: A literature review. Journal of the American Medical Informatics Association, 14(2), 156-163. https://doi.org/10.1197/jamia.M2255
- ECG Consultants. (2015). The use of technology in healthcare reform: IT considerations for accountable care.www.ecgmc.com/thought-leadership/articles/the-use-of-technology-in-healthcare-reform-it-considerations-for-accountable-care
- eHealth Initiative. (2019). The importance of social determinants of health data. www.ehidc.org/sites/default/files/resources/files/Importance%20of%20SDOH%20Data%20March%202019.pdf
- Embi P. J., Jain A., Clark J., Bizjack S., Hornung R., & Harris C. M. (2005). Effect of a clinical trial alert system on physician participation in trial recruitment. Archives of Internal Medicine, 165(19), 2272-2277. http://dx.doi.org/10.1001/archinte.165.19.2272
- Federal Register. (2020a). 21st Century Cures Act: Interoperability, information blocking, and the ONC health IT certification program. Final rule. www.federalregister.gov/documents/2020/05/01/2020-07419/21st-century-cures-act-interoperability-information-blocking-and-the-onc-health-it-certification
- Federal Register. (2020b). Department of Health and Human Services: Office of the Secretary, 45 CFR Parts 170 and 171, RIN 0955-AA01, 21st Century Cures Act: Interoperability, information blocking, and the ONC health IT certification program. www.govinfo.gov/content/pkg/FR-2020-05-01/pdf/2020-07419.pdf
- Green J. (2023, January 5). What are the core functions of EHR? EHR in Practice. www.ehrinpractice.com/ehr-core-functions.html
- Halamka J. D. (2006). Health information technology: Shall we wait for the evidence? Annals of Internal Medicine, 144(10), 775-776. https://doi.org/10.7326/0003-4819-144-10-200605160-00013
- Healthcare Information and Management Systems Society. (n.d.-a). Electronic medical record adoption model: EMRAM. www.himss.org/what-we-do-solutions/digital-health-transformation/maturity-models/electronic-medical-record-adoption-model-emram
- Healthcare Information and Management Systems Society. (n.d.-b). HIMSS Davies Award of Excellence. www.himss.org/what-we-do-opportunities/davies-award-excellence
- Healthcare Information and Management Systems Society. (n.d.-c). Stage 6 and 7 facilities by location. www.himss.org/what-we-do-solutions/digital-health-transformation/achievement-list
- Healthcare Information and Management Systems Society. (n.d.-d). TIGER: An initiative for technology and health informatics education.www.himss.org/tiger-initiative-technology-and-health-informatics-education
- Healthcare Information and Management Systems Society. (2014). 6th annual HIMSS security survey. www.himss.org/sites/hde/files/2013_HIMSS_Security_Survey.pdf
- Healthcare Information and Management Systems Society. (2017). EMRAM overview and criteria update. www.himss.org/what-we-do-solutions/digital-health-transformation/maturity-models/electronic-medical-record-adoption-model-emram
- Healthcare Information and Management Systems Society. (2020). 2019 HIMSS Davies Award winners: Improving health and wellness through information and technology. www.himss.org/resource-news/2019-himss-davies-award-winners
- Healthy People 2030. (n.d.). Social determinants of health. U.S. Department of Health and Human Services. https://health.gov/healthypeople/priority-areas/social-determinants-health
- HL7 International. (n.d.). About HL7. www.hl7.org/about/index.cfm?ref=nav
- Husk G., & Waxman D. A. (2004). Using data from hospital information systems to improve emergency care. Academic Emergency Medicine, 11(11), 1237-1244. https://doi.org/10.1197/j.aem.2004.08.019
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press.
- Institute of Medicine. (2003). Key capabilities of an electronic health record system: Letter report.National Academies Press.
- Jain A., Atreja A., Harris C. M., Lehmann M., Burns J., & Young J. (2005). Responding to the rofecoxib withdrawal crisis: A new model for notifying patients at risk and their healthcare providers. Annals of Internal Medicine, 142(3), 182-186. https://doi.org/10.7326/0003-4819-142-3-200502010-00008
- Juhn E., & Galvez E. (2022). Incentivizing data sharing among health plans, hospitals, and providers to improve quality. The American Journal of Managed Care, 28(12), e426-e427. https://doi.org/10.37765/ajmc.2022.89277
- Kim T. Y., Hardiker N., & Coenen A. (2014). Inter-terminology mapping of nursing problems. Journal of Biomedical Informatics, 49, 213-220. https://doi.org/10.1016/j.jbi.2014.03.001
- Konschak C., & Shiple D. (n.d.). System selection: Aligning vision and technology. Divurgent. http://divurgent.com/wp-content/uploads/2013/12/White-Paper.Vendor-Selection.vfinal.pdf
- Kutney-Lee A., & Kelly D. (2011). The effect of hospital electronic health record adoption on nurse-assessed quality of care and patient safety. Journal of Nursing Administration, 41(11), 466-472. http://dx.doi.org/10.1097/NNA.0b013e3182346e4b
- Matney S. A., Warren J. J., Evans J. L., Kim T. Y., Coenen A., & Auld V. A. (2012). Development of the nursing problem list subset of SNOMED CT. Journal of Biomedical Informatics, 45(4), 683-688. http://dx.doi.org/10.1016/j.jbi.2011.12.003
- Monegain B. (2010, February 24). Davies goes to multicare. Healthcare IT News. www.healthcareitnews.com/news/davies-goes-multicare
- National Academy of Medicine. (2017). Optimizing strategies for clinical decision support. https://nam.edu/wp-content/uploads/2017/11/Optimizing-Strategies-for-Clinical-Decision-Support.pdf
- National Institute of Standards and Technology. (2010a). Standards for health IT: Meaningful use and beyond. www.nist.gov/speech-testimony/standards-health-it-meaningful-use-and-beyond
- National Institute of Standards and Technology. (2010b). Meaningful use test method: Approved test procedures version 1.0.www.nist.gov/news-events/news/2010/08/nist-publishes-approved-testing-procedures-electronic-health-records
- National Institutes of Health. (2006, April). Electronic health records overview. MITRE Corporation. https://webarchive.library.unt.edu/eot2008/20090114061920/http://www.ncrr.nih.gov/publications/informatics/EHR.pdf
- Office of the National Coordinator for Health Information Technology. (n.d.). National trends in hospital and physician adoption of electronic health records. www.healthit.gov/data/quickstats/national-trends-hospital-and-physician-adoption-electronic-health-records
- Office of the National Coordinator for Health Information Technology. (2015). Understanding certified health IT. www.healthit.gov/sites/default/files/understanding-certified-health-it-2.pdf
- Office of the National Coordinator for Health Information Technology. (2017a). Benefits of EHRs. www.healthit.gov/topic/health-it-and-health-information-exchange-basics/benefits-ehrs
- Office of the National Coordinator for Health Information Technology. (2017b). Standard nursing terminologies: A landscape analysis. www.healthit.gov/sites/default/files/snt_final_05302017.pdf
- Office of the National Coordinator for Health Information Technology. (2019a). Electronic health records: The basics.www.healthit.gov/faq/what-information-does-electronic-health-record-ehr-contain
- Office of the National Coordinator for Health Information Technology. (2019b). Shared nationwide interoperability roadmap: The journey to better health and care. www.healthit.gov/infographic/shared-nationwide-interoperability-roadmap-journey-better-health-and-care
- Office of the National Coordinator for Health Information Technology. (2022). Advantages of electronic health records.www.healthit.gov/faq/what-are-advantages-electronic-health-records
- Office of the National Coordinator for Health Information Technology. (2023). 2015 edition cures update test method. www.healthit.gov/topic/certification-ehrs/2015-edition-cures-update-test-method
- Paruk F. (2019, January 8). Uncovering social determinants of health in your EHR data. Becker's Hospital Review. www.beckershospitalreview.com/hospital-physician-relationships/uncovering-social-determinants-of-health-in-your-ehr-data.html
- Ponte P., Somerville J., & Adams J. (2016). Assuring the capture of standardized nursing data: A call to action for chief nursing officers. International Journal of Nursing Knowledge, 27(3), 127-128. https://doi.org/10.1111/2047-3095.12136
- Poprock B. (2005, September). Using Epic's alternative medications reminder to reduce prescription costs and encourage assistance programs for indigent patients. Paper presented at the Epic Systems Corporation Users Group Meeting, Madison, WI.
- Reed H. L., & Bernard E. (2005). Reductions in diabetic cardiovascular risk by community primary care providers. International Journal of Circumpolar Health, 64(1), 26-37. https://doi.org/10.3402/ijch.v64i1.17951
- Rohatgi A. (2022). Improve patient outcomes by integrating SDOH data into EHRs. Journal of AHIMA. https://journal.ahima.org/page/improve-patient-outcomes-by-integrating-sdoh-data-into-ehrs
- Shekelle P. G., Morton S. C., & Keeler E. B. (2006). Costs and benefits of health information technology. Agency for Healthcare Research and Quality. www.ahrq.gov/downloads/pub/evidence/pdf/hitsyscosts/hitsys.pdf
- Spooner S. A., & Council on Clinical Information Technology. (2007). Special requirements of electronic health record systems in pediatrics. Pediatrics, 119(3), 631-637. https://doi.org/10.1542/peds.2006-3527
- Sterrett L., Batra N., Harris C., Talbot C., Chang C., & Malhotra R. (2022, October 19). Preparing for the next generation of electronic health records. Deloitte Insights. www2.deloitte.com/us/en/insights/industry/health-care/ehr-systems-the-future-of-electronic-health-records.html
- Thompson D. I., Osheroff J., Classen D., & Sittig D. F. (2007). A review of methods to estimate the benefits of electronic medical records in hospitals and the need for a national database. Journal of Healthcare Information Management, 21(1), 62-68.
- Welter T. (2015, May 13). The use of technology in healthcare reform: IT considerations for accountable care. ECG Management Consultants. www.ecgmc.com/thought-leadership/articles/the-use-of-technology-in-healthcare-reform-it-considerations-for-accountable-care