A Look at Pacemakers
A pacemaker is an artificial device that electrically stimulates the myocardium to depolarize, which begins a contraction.
Pacemakers are usually used for (1) bradycardia caused by sinus node dysfunction (SND), medications, or atrioventricular (AV) block and (2) cardiac dyssynchrony because of advanced heart failure. The device may be temporary or permanent, depending on the patient’s condition. Pacemakers are commonly necessary for the aging heart and following myocardial infarction or cardiac surgery.

and the Beat Goes on…
Pacemakers work by generating an impulse from a power source and transmitting that impulse to the heart muscle. The impulse flows throughout the heart and causes the heart muscle to depolarize. Pacemakers usually consist of three components: the pulse generator, the pacing leads, and the electrodes at the tips of the pacing leads.
Making the Pacer Work
The pulse generator contains the pacemaker’s power source and circuitry. The lithium battery in a permanent or implanted pacemaker is its power source and lasts about 10 years. The circuitry of the pacemaker is a microchip that guides heart pacing.
A temporary pacemaker, which isn’t implanted, is about the size of large cell phone or a telemetry box and is powered by alkaline batteries. These units also contain a microchip and are programmed by a touch pad or dials.
A Stimulus on the Move
An electrical stimulus from the pulse generator moves through wires (referred to as pacing leads or leads) to the electrode tips. The leads for a pacemaker designed to stimulate a single heart chamber are placed in either the atrium or the ventricle. For dual-chamber, or AV, pacing, the leads are placed in both chambers, usually on the right side of the heart.
One Pole or Two
The electrodes—one on a unipolar lead or two on a bipolar lead—send information about electrical impulses in the myocardium back to the pulse generator. The pulse generator senses the heart’s electrical activity and responds according to how it has been programmed.
A unipolar lead system is more sensitive to the heart’s intrinsic electrical activity than is a bipolar system. A bipolar system isn’t as easily affected by electrical activity outside the heart and the generator (e.g., from skeletal muscle contraction or magnetic fields). (See A look at pacing leads.)
Working with Pacemakers
On an ECG, you’ll notice the spike from a unipolar system right away. (See Pacemaker spikes.) It occurs when the pacemaker sends an electrical impulse to the heart muscle. That impulse appears as a vertical line or spike. The spike with a bipolar system can sometimes be difficult to see.
Depending on the position of the electrode, the spike appears in different locations on the waveform.
- When the atria are stimulated by the pacemaker, the spike is followed by a P wave and then the paced or patient’s intrinsic QRS complex, then the T wave. This series of waveforms represents successful capture of the atrial myocardium. The P wave may look different from the patient’s intrinsic P wave.
- When the ventricles are stimulated by a pacemaker, the spike is followed by a QRS complex and a T wave. The paced QRS complex usually appears wider than the patient’s intrinsic QRS complex because of the longer time it takes the ventricles to depolarize when paced.
- When the pacemaker stimulates both the atria and the ventricles, the first spike is followed by a P wave, then another spike, and then a QRS complex. Be aware that the type of pacemaker used and the patient’s condition may affect whether every beat is paced.
Permanent and Temporary Pacemakers
Depending on the patient’s needs, a permanent or a temporary pacemaker can be used to maintain heart rhythm. Pacing lead placement varies according to the patient’s specific needs.
Permanent Pacemakers
A permanent pacemaker is used to treat chronic heart conditions such as SND, AV block, or dyssynchrony. SND causing symptomatic bradycardia can be because of advanced age or drug therapy. AV block is commonly because of cardiomyopathy, cardiac surgery, or septal ablation. Dyssynchrony between all the chambers and within the left ventricle is caused by advanced cardiomyopathy. Permanent pacemakers are surgically implanted, usually under local anesthesia. (See Placing a permanent pacemaker.)
Pocket Generator
The generator consists of a battery and microchip circuitry enclosed in a titanium case. It is implanted in a pocket made from subcutaneous tissue. The pocket is usually constructed under the clavicle. Permanent pacemakers are initially programmed during implantation. The programming determines how the pacemaker functions and can be adjusted externally when necessary.
Permanent Pacing Leads
Permanent pacing leads are usually placed transvenously. They are positioned in the appropriate chambers and then anchored to the endocardium or in the coronary sinus for left ventricular pacing. Some patients may require permanent epicardial pacing leads that are placed during cardiac surgery. This is common for patients with tricuspid valve surgery and for patients who require left ventricular pacing but a coronary sinus lead was unable to be placed transvenously. (See Placing a permanent pacemaker.)
Leadless Pacemakers
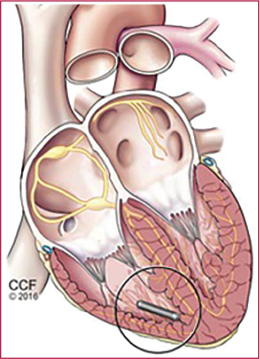
This is a self-contained pacemaker the size and shape of a large capsule of medicine. It is placed within the right ventricle via the femoral vein. Therefore, there is no chest incision or lead wire. It paces and senses only the right ventricle. It is indicated for people in whom atrial pacing is not needed. For example, for patients with:
- Symptomatic high-grade AV block in the presence of atrial fibrillation
- Symptomatic high-grade AV block or SND and when an atrial lead implant is difficult, high risk or not needed
Temporary Pacemakers
A temporary pacemaker is commonly inserted in an emergency. The patient may show signs of decreased cardiac output, such as hypotension or syncope. The temporary pacemaker supports the patient until the condition resolves.
A temporary pacemaker can also serve as a bridge until a permanent pacemaker is inserted, for example, immediately following cardiac surgery or while awaiting resolution of a bloodstream infection. Temporary pacemakers are used for patients with heart block, sinus bradycardia, or low cardiac output. Several types of temporary pacemakers are available, including transvenous, epicardial, and transcutaneous.
Temporary pacemakers should have the batteries, pacing thresholds, and connections between the pacing leads and generator routinely checked. The insertion sites should be kept sterile and be regularly monitored. Unit-based guidelines need to exist for this routine care.
Going the Transvenous Way
The transvenous approach is used when inserting a temporary pacemaker in nonsurgical environments. In this method, the pacing leads are commonly inserted through the subclavian or internal jugular vein. The transvenous pacemaker is probably the most common and reliable type of temporary pacemaker. It’s usually inserted at the bedside or in a fluoroscopy suite. The pacing lead is typically advanced through a catheter into the right ventricle and then connected to an external pulse generator.
Taking the Epicardial Route
Epicardial pacemakers are commonly placed while patients are undergoing cardiac surgery. The doctor attaches the tips of the pacing leads (thin wires) to the surface of the heart and then brings the wires through the chest wall, below the incision. They’re then attached to an external pulse generator. The pacing wires are usually cut or removed several days after surgery or when the patient no longer requires them.
Following the Transcutaneous Path

Use of an external or transcutaneous pacemaker has become commonplace. In this noninvasive method, one electrode pad is placed over the heart on the patient’s anterior chest wall, and a second is applied behind the heart on the back. An external pulse generator then emits pacing impulses that travel through the skin, muscle, and bone to the heart muscle. Transcutaneous pacing is also built into many external defibrillators for use in an emergency. In this case, the pacing electrode pads are built into the same electrode pads used for defibrillation.
Transcutaneous pacing is a quick and effective method of pacing heart rhythm and is commonly used in an emergency until a transvenous pacemaker can be inserted. However, some alert patients can’t tolerate the painful electrical stimuli produced from pacing at the levels needed to capture the myocardium through the chest wall.
Setting the Controls
When your patient has a temporary pacemaker, you’ll notice several types of settings on the pulse generator. The rate control regulates how many impulses are generated in 1 minute and is measured in pulses per minute (ppm). The rate is usually set at 60 to 80 ppm. (See A look at a pulse generator.) The pacemaker is usually programmed in a demand mode. Thus, it fires only if the patient’s heart rate falls below the rate (e.g., 60) set on the pacemaker. The rate may be set higher in an effort to increase cardiac output or if the patient has a tachyarrhythmia that’s being treated with overdrive pacing.
Measuring the Output
The electrical output of a temporary pacemaker is measured in milliamperes (mA). First, the stimulation threshold, or the minimum amount of energy required to capture or stimulate the cardiac muscle to depolarize, is assessed. Then the pacemaker’s output is set 10% higher than the stimulating threshold to ensure myocardial capture under various physiologic conditions, for example, hypokalemia.
Sensing the Norm
You can also program the pacemaker’s sensing or ability to sense electricity (e.g., P waves and QRS complexes). Sensing is measured and set in millivolts (mV). Most pacemakers are programmed in a demand mode; therefore, only pacing when the heart’s own electrical activity is not sensed. Pacing is inhibited when the heart’s own P waves and QRS complexes are sensed. This may be referred to as demand pacing. So many patients will at times have a paced rhythm, an intrinsic rhythm, or a rhythm with both paced and intrinsic beats at any given time.
| Ages and stages |
Adult patients are more apt to have AV block. Therefore, they usually get a dual-chamber pacemaker. This allows for synchronous pacing and contraction between the atria and ventricles. Cardiac output and exercise tolerance are increased because of increased ventricular filling. Older adults are more prone to permanent atrial fibrillation. Because atrial pacing is not possible during atrial fibrillation, a single-chamber ventricular pacemaker is typical for these patients when they have bradycardia. |
Pacemaker Codes
The capabilities of permanent pacemakers may be described by a generic five-letter coding system, although three letters are more commonly used. (See Pacemaker coding system.)
Introducing Letter 1
The first letter of the code identifies the heart chambers that can be paced when necessary. These are the options and the letters used to signify those options:
- V = Ventricle
- A = Atrium
- D = Dual (ventricle and atrium)
- O = None
Learning About Letter 2
The second letter of the code signifies the heart chamber in which the pacemaker senses the intrinsic activity:
- V = Ventricle
- A = Atrium
- D = Dual (ventricle and atrium)
- O = No sensing. When a pacemaker doesn’t sense intrinsic electricity, it paces, even if intrinsic activity exists. This is referred to as asynchronous pacing. Although permanent pacemakers may be programmed this way when the patient is undergoing certain procedures, temporary pacemakers should not be. Asynchronous pacing in the ventricle with a temporary pacemaker can lead to ventricular tachycardia (VT), ventricular fibrillation, or torsades de pointes.

Looking at Letter 3
The third letter indicates the pacemaker’s response to the intrinsic electrical activity it senses in the atrium or ventricle:
- T = Triggers pacing (For instance, if atrial activity is sensed, ventricular pacing may be triggered.)
- I = Inhibits pacing (If the pacemaker senses intrinsic activity in a chamber, it won’t fire in that chamber.)
- D = Dual (The pacemaker can be triggered or inhibited in the atrium, ventricle, or both.)
- O = None (The pacemaker doesn’t respond to electrical activity.) If a pacemaker can’t sense because the second letter is an O, then the third letter is usually also an O. A pacemaker that can’t sense can’t respond to an event.

Figuring Out Letter 4
The fourth letter of the code describes rate modulation, also known as rate responsiveness or rate adaptive pacing:
- R = Rate modulation. (A sensor adjusts the programmed paced heart rate in response to the patient’s physiologic need. For example, increased movement or respiratory rate will increase the paced rate.) This is used for chronotropic incompetence or when the patient’s sinus node can’t increase the sinus rate during increased physiologic demand .
- O = None. (Rate modulation is unavailable or disabled.)
Finally, Letter 5
The final letter of the code is rarely used but specifies the location or absence of multisite pacing:
- O = None (No multisite pacing is present.)
- A = Atrium or atria (Multisite pacing in the atrium or atria is present.)
- V = Ventricle or ventricles (Multisite pacing in the ventricle or ventricles is present.)
- D = Dual site (Dual-site pacing in both the atrium and ventricles is present.)
Pacemaker Modes
The mode of a pacemaker indicates its functions. Several different modes may be used during pacing. Here are three of the more commonly used modes and their three-letter abbreviations. (A three-letter code, rather than a five-letter code, is typically used to describe pacemaker function.) Pacemaker rates vary by age (see Pediatric pacemakers) and other patient characteristics.
AAI Mode
The AAI, or atrial demand , pacemaker is a single-chambered pacemaker that paces and senses the right atrium. When the pacemaker senses intrinsic atrial activity, it inhibits pacing and resets itself. If it does not sense intrinsic atrial activity, it paces. Only the atria are sensed and paced.
Not in Block
Because an AAI pacemaker requires a healthy and functioning AV node and resulting consistent ventricular conduction, it isn’t used in AV block. An AAI pacemaker may be used in patients with sinus bradycardia, as after heart transplant, or with sick sinus syndrome as long as the His–Purkinje system isn’t diseased.
VVI Mode
The VVI, or ventricular demand , pacemaker paces and senses the ventricles. (See AAI and VVI pacemakers.) When it senses intrinsic ventricular activity, it inhibits pacing. This single-chambered pacemaker benefits patients with complete heart block and those needing rare or less frequent pacing. Because it doesn’t affect atrial activity, it may be used for patients with a temporary pacemaker (e.g., postcardiac surgery) who don’t need an atrial kick. Atrial kick is the extra 15% to 30% of cardiac output that comes from atrial contraction. The VVI mode is also common for patients with a permanent pacemaker who have long-stand ing persistent atrial fibrillation.

Unsynchronized Activity
If the patient has spontaneous atrial activity, the VVI pacemaker won’t synchronize the ventricular activity with it. So there will be no relationship between the P waves and paced QRS complexes, and tricuspid and mitral regurgitation may develop. Sedentary patients who don’t need the atrial kick, or patients with atrial fibrillation, may receive this pacemaker.
DDD Mode
A DDD pacemaker is used with AV block. Annual incidence of AVB development in people with SND is about 1–5%. Therefore, some patients with SND get a dual-chamber pacemaker. (See DDD pacemaker rhythm strip.) However, because the pacemaker possesses so many capabilities, it may be hard to troubleshoot problems. Its advantages include its
- versatility
- programmability
- ability to provide a more physiologic cardiac cycle than VVI pacing by pacing the ventricles following atrial activity (P waves) but not above the set maximal rate limit
- ability to change modes automatically. DDD pacemakers can be programmed in an AAI mode that automatically switches to DDD when a P wave is not conducted to the ventricles. This is advantageous for patients with intermittent loss of AV conduction because intrinsic AV conduction, as used in AAI mode, is more physiologic than dual-chamber pacing. However, a patient with AVN disease would not receive a pacemaker that only paces in the atrium. Pacemakers can also automatically change to a nontracking mode if the atrial rate goes too high, as in atrial fibrillation.
Home, Home on the Rate Range
Unlike other pacemakers, the DDD pacemaker is set with a rate range, rather than a single critical rate. It senses atrial activity and ensures that the ventricles track or respond to each atrial stimulation up to an upper ventricular rate limit, thereby maintaining normal AV synchrony. A typical rate range is from 60 to 120 bpm. This causes pacing in the atrium once the atrial rate falls below 60. The ventricles will track (be paced after each P wave) if there is no sensed QRS complex, up to 120 bpm. A pacemaker can’t stop a heart’s intrinsic conduction. Therefore, even though a pacemaker’s upper rate may be 120, the patient’s heart rate may well exceed 120 bpm when there is intact intrinsic AV conduction.
Taking the Low Road
The DDD pacemaker paces (sometimes referred to as “fires”) in the atria when the atrial rate falls below the lower set rate. If the ventricles don’t respond to an atrial event, the pacemaker will pace the ventricles. (See Evaluating a DDD pacemaker rhythm strip.) You or the telemetry monitor may calculate the heart rate by averaging 6 or 10 seconds. However, the pacemaker calculates the heart rate between two consecutive beats. Therefore, although you or a monitor may average the heart rate as being 60 or higher, the pacemaker will pace if the patient’s intrinsic rate is 59 between two consecutive beats.
Taking the High Road
The upper set rate acts as a safety mechanism by preventing the pacemaker from following (or tracking) an atrial tachyarrhythmia such as atrial fibrillation, atrial tachycardia, or atrial flutter. That upper rate limit is usually set at 120 or 130 bpm. One’s AV node would normally block the approximate 500 atrial bpm during atrial fibrillation from passing to the ventricle. The AV node is bypassed with a pacemaker, making the upper rate limit necessary with a DDD pacemaker.
Evaluating Pacemakers
Now you’re ready to find out if your patient’s pacemaker is working correctly. To do this, follow the procedure described below.
Read the Records
First, determine the pacemaker’s mode and settings, particularly the rate setting. If your patient had a permanent pacemaker implanted before admission, ask them whether they have a wallet card from the manufacturer that notes which generator and pacing leads were implanted.
If the pacemaker was recently implanted, check the patient’s records for information. Don’t check only the ECG tracing—you might misinterpret it if you don’t know the mode or which pacing leads the patient has.
Look at the 12-Lead ECG
Next, review the patient’s 12-lead ECG. If it isn’t available, examine lead V1 or MCL1 on telemetry. If there is only one ventricular lead, it is usually in the right ventricle. Therefore, expect a negatively deflected paced QRS complex in V1 or MCL1, just as with a left bundle branch block. An upright QRS complex in V1 or MCL1 may mean that the pacing lead is out of position, perhaps even perforating the septum and lodging in the left ventricle, or that there is a properly positioned pacing lead in the coronary sinus vein. When the His bundle is paced, the QRS complex should be narrow.
Scrutinize the Spikes
Then select a monitoring lead that clearly shows the pacemaker spikes. Some monitors have a filter or band width menu that allows adjustment for seeing larger pacemaker spikes. Make sure to use the “paced mode” on the telemetry monitor. If the monitor doesn’t “know” it’s looking at a rhythm that may have pacemaker spikes, it can interpret a pacemaker spike as a QRS complex. Therefore, a pacemaker spike that is not followed by a QRS complex without the “paced mode” on will NOT cause an important alarm.
Mull over the Mode
When looking at the ECG tracing of a patient with a pacemaker, consider the pacemaker mode. Then interpret the paced rhythm. Does it match what you know about the pacemaker?
Unravel the Rhythm

Look for information that tells you which chamber is paced. Is there capture? Is there a P wave or QRS complex after each atrial or ventricular spike? Or do the P waves and QRS complexes stem from intrinsic activity?
Look for information about the pacemaker’s sensing ability. Do you see spikes where you wouldn’t expect them? Like within or too close after a P wave or QRS complex? Remember if the pacemaker is sensing the electricity causing the P waves and QRS complexes, it should withhold a spike. Look at the rate. What’s the pacing rate per minute? Is it appropriate given the pacemaker upper and lower rate setting? Although you can determine the rate quickly by counting the number of complexes in a 6-second ECG strip, a more accurate method is to count the number of small boxes between two complexes and divide this into 1,500.
Troubleshooting Problems
Pacemaker malfunction can lead to arrhythmias and /or loss of AV synchrony. (See When a temporary pacemaker malfunctions) If you see questionable pacemaker activity for a patient with a permanent pacemaker, call the cardiology or cardiac electrophysiology team. There are actions you should take for patients with temporary pacemakers who have questionable pacemaker activity. Pacemaker problems that can lead to low cardiac output, hypotension, syncope, and death include
| Mixed signals | |||||||
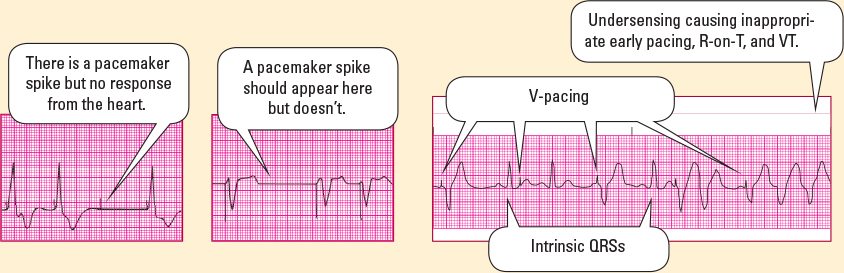
Occasionally, pacemakers fail to function properly. When that happens, you need to take immediate action to correct the problem. The strips shown below are examples of problems that can occur with a temporary pacemaker and corrective actions to take in response.
|
- failure to capture
- failure to pace
- undersensing
- oversensing.
Failure to Capture
Failure to capture is indicated on an ECG by a pacemaker spike without the appropriate atrial or ventricular response—a spike without a complex. Think of failure to capture as the pacemaker’s inability to stimulate the chamber to contract.
Causes include hypoxia, acidosis, an electrolyte imbalance, fibrosis, an incorrect lead position, a low pacing output setting (milliampere with temporary pacemakers and volts with permanent pacemakers), depletion of the battery, a broken or cracked pacing lead, or perforation of the pacing lead through the myocardium. It can lead to light-headedness, hypotension, or asystole.
Failure to Pace
Failure to pace is indicated by no pacemaker activity or spike at the set rate on an ECG. The problem is caused by battery or circuit failure, cracked or broken pacing leads, loose connections, oversensing, or the pacing output set too low. It can also lead to light-headedness, hypotension, or asystole.
Undersensing
Undersensing is demonstrated by a pacemaker spike when intrinsic cardiac activity is already present. Undersensing causes the pacemaker to fire even if intrinsic electricity is present. Think of it as help being given when none is needed. With undersensing, spikes occur on the ECG where they shouldn’t. Although they may appear in any part of the cardiac cycle, the spikes are especially dangerous with a temporary pacemaker if they fall on the T wave. This can cause “R-on-T,” resulting in VT, ventricular fibrillation, or torsades de pointes. The output of a temporary pacemaker is much higher than that of a permanent pacemaker. Therefore, undersensing with a temporary pacemaker as opposed to a permanent pacemaker can lead to a fatal arrhythmia. With a permanent pacemaker, the unneeded pacing would most likely result in early battery depletion.
The problem can be caused by millivoltage set too high, electrolyte imbalances, disconnection or dislodgment of a lead, improper pacing lead placement, edema or fibrosis at the electrode tip, drug interactions, or a depleted or dead pacemaker battery.
Oversensing
If the pacemaker is too sensitive, it can misinterpret other electricity as the heart’s electricity and therefore withhold pacing. This extraneous electricity can be from myopotentials from nearby muscle movement, electrical events in a different chamber, electricity from nongrounded items, or certain equipment that have a strong magnetic or electrical field. You should wear rubber gloves when hand ling exposed temporary pacing wires. This will prevent you from transmitting electrical current from static or ungrounded equipment to the patient. Likewise, temporary pacing wires should be covered with something nonconductive, like the finger of a rubber glove. Oversensing causes inhibition of pacing when the patient actually needs it. The heart rate, AV synchrony, and cardiac output won’t be maintained. This can cause asystole, hypotension, light-headedness, and /or syncope.
How You Intervene
Make sure you’re familiar with different types and modes of pacemakers and how they function. This will save you time and worry during an emergency. When caring for a patient with a pacemaker, follow these guidelines.
Checks and Balances
Temporary Pacemakers
- Assist with pacemaker insertion as appropriate.
- Regularly check the patient’s pacemaker settings, connections, and functions.
- Reposition the patient carefully. Turning may dislodge the pacing wire.
- Avoid potential microshocks to the patient by ensuring that electrical equipment is grounded properly, including the patient’s bed.

All Pacemakers
- Remember that pacemaker spikes on the monitor don’t mean there is capture or that your patient is stable. Be sure to check the vital signs and assess for signs and symptoms of decreased cardiac output, such as hypotension, chest pain, dyspnea, light-headedness, and syncope.
- Turn the telemetry monitor’s “paced mode” on.
- Monitor the patient to see how well they tolerate the pacemaker.
On the Alert
- Be alert for signs of local and /or systemic infection.
- Look for pectoral or diaphragmatic muscle twitching or hiccups that occur in synchrony with the pacemaker. Both are signs of stimulation of a structure other than the heart, which may be serious. Notify the practitioner if you note either condition.
- Watch for a perforated ventricle and cardiac tamponade. Signs and symptoms include persistent hiccups, distant heart sounds, pulsus paradoxus (a drop in the strength of a pulse or a drop in systolic blood pressure greater than 10 mm Hg during inspiration), hypotension with narrowed pulse pressure, cyanosis, distended jugular veins, decreased urine output, restlessness, and complaints of fullness in the chest. Notify the practitioner immediately if you note any of these signs and symptoms.
- Watch for pneumothorax signs and symptoms, including shortness of breath, restlessness, and hypoxia. Mental status changes and arrhythmias may also occur. Palpate for subcutaneous air, which feels crunchy under your fingers, around the pacemaker insertion site. Auscultate for diminished breath sounds over the pneumothorax, usually at the apex of the lung on the side where the pacemaker was placed. Notify the practitioner if you suspect pneumothorax.
- Assess the area around the incision and report swelling, tenderness, drainage, redness, unusual warmth, or hematoma. Patients on anticoagulation or antiplatelet therapy are at higher risk of bleeding at the insertion site, which increases the chances of infection.
What to Teach the Patient and Significant Other (s)
Temporary pacemakers:
- Explain why a pacemaker is needed, how it works, and what they can expect.
- Warn the patient with a temporary pacemaker not to get out of bed without assistance.
- Explain that a transcutaneous pacemaker causes twitching of the pectoral muscles. Reassure that you will be asking the patient if medication is desired for the discomfort.
- Instruct the patient not to manipulate the temporary pacemaker wires or pulse generator; and not to “fiddle” with the implanted generator.
Permanent pacemakers: In addition to explaining need, function, and expectations, give patients with permanent pacemakers the following:

- Teach how to care for the incision. Advise the patient to avoid tight clothing or other direct pressure over the pulse generator. The patient should observe the incision daily and notify the healthcare practitioner of redness or other signs of infection.
- Give the patient the manufacturer’s identification card and tell them to carry it at all times. They should show it to airport or law enforcement personnel as to avoid walking through strong metal detectors used by these staff.
- Inform the patient that they may want to wear a medical identification bracelet indicating that they have an implanted device in case they need medical attention and are unable to speak.
- Emphasize the importance of identifying pacemaker problems via routine remote and in-office checks.
- Explain the signs and symptoms of pacemaker malfunction, how to take a pulse, and what to do if any signs or symptoms exist, including notification of the healthcare practitioner.
- Advise the patient to avoid moving the arm on the side of the pacemaker in an extreme, exaggerated, or repetitive manner for 6 to 8 weeks or per the healthcare provider who cares for the permanent pacemaker.
- Advise the patient to speak to the practitioner who manages the pacemaker before having magnetic resonance imaging, radiation therapy, surgery, or diagnostic studies. The practitioner should also be consulted before use of power-generating equipment, equipment with antennas, or strong magnets.
- Tell the patient to follow normal routines and to increase exercise as tolerated and as allowed by the practitioner.
- Stress the importance of follow-up care and regular check-ups.
- Explain that a remote monitor is frequently used in the patient’s home to alert practitioners of rhythms and device function and to reduce the need for some office visits.
A Look at Biventricular Pacemakers
Biventricular pacing is used in the treatment of some patients with class III and IV heart failure, with both systolic heart failure and intraventricular conduction delay. Also called cardiac resynchronization therapy, biventricular pacing reduces symptoms and improves the quality of life of patients with advanced heart failure. It also records heart failure parameters such as those indicating the amount of fluid in the chest.
Two Ventricles, Three Leads
Unlike other pacemakers, a biventricular pacemaker usually has three leads rather than one or two: one to pace the right atrium, one to pace the right ventricle, and one to pace the left ventricle. Both ventricles are commonly either paced at the same time or the left ventricle is paced milliseconds before the right ventricle. This causes them to contract about the same time, increasing cardiac output.
Different Ventricles, Different Timing
Under normal conditions, the right and left ventricles contract simultaneously to pump blood to the lungs and body, respectively. However, in heart failure, the damaged ventricles can’t pump as forcefully and the amount of blood ejected with each contraction is reduced. If the ventricular conduction pathways are also damaged, electrical impulses reach the ventricles at different times, producing asynchronous contractions. This condition, called intraventricular conduction defect, further reduces the amount of blood that the heart pumps, worsening the patient’s symptoms.
An Important Tip
Unlike traditional lead placement, the pacing lead for the left ventricle is placed into a branch of a cardiac vein via the coronary sinus. This vein lies on the exterior of the left ventricle. The left ventricle is paced through the wall of the vein. Because this pacing lead isn’t anchored in place, lead displacement may be more likely to occur. (See Biventricular lead placement.)
Improves Symptoms and Quality of Life
Biventricular pacing produces an improvement in the patient’s symptoms and activity tolerance. Moreover, biventricular pacing improves left ventricular remodeling and diastolic function and reduces sympathetic stimulation. As a result, in many patients, the progression of heart failure is slowed and quality of life is improved.
Sympathetic Response

To compensate for reduced cardiac output, the sympathetic nervous system releases neurohormones, such as aldosterone, norepinephrine, and vasopressin, to boost the amount of blood ejected with each contraction. The resultant tachycardia and vasoconstriction increase the heart’s demand for oxygen, reduce diastolic filling time, promote sodium and water retention, and increase the pressure that the heart must pump against. The effect on the patient is a worsening of symptoms. Resynchronization therapy can reduce symptoms of heart failure, decrease hospitalizations and morbidity, and improve quality of life.
Who’s a Cand idate?
Not all patients with heart failure benefit from biventricular pacing. Cand idates should have both systolic heart failure and intraventricular conduction delay along with these characteristics:
- symptomatic heart failure despite maximal medical therapy
- moderate to severe heart failure (New York Heart Association class III or IV)
- QRS complex greater than 0.13 second
- left ventricular ejection fraction (EF) of 35% or less.
Many patients who meet criteria for biventricular pacing also meet criteria for a defibrillator. Therefore, patients having defibrillators with biventricular pacing (biventricular implantable cardioverter-defibrillator [ICD]) is very common.
Caring for the Patient
Provide the same basic care for the patient with a biventricular pacemaker that you would for a patient with a stand ard permanent pacemaker. Specific care includes these guidelines:
- Before the procedure, ask the patient if he/she has an allergy to iodine or shellfish because contrast medium is used to visualize the coronary sinus and veins. Notify the practitioner if an allergy exists.
- Because of the position of the left ventricular lead, watch for stimulation of the diaphragm and left chest wall. Ask patients if they feel any thumping in or on their chest. Notify the practitioner if this occurs because the left ventricular pacing lead output or configuration may need to be reprogrammed or the left ventricular lead may need repositioning.
- Observe the ECG for pacemaker spikes. Although both ventricles are paced, usually only one ventricular pacemaker spike is seen.
- Note the presence of positive R waves in lead V1, and negative R waves in leads I and aVL. Notify the practitioner if this isn’t the case or if the R-wave direction changes at any time.

What to Teach the Patient
Provide the same basic teaching that you would for the patient receiving a permanent pacemaker. Additionally, when a patient gets a biventricular pacemaker, be sure to cover these points:
- Explain to the patient and their family why a biventricular pacemaker is needed, how it works, and what they can expect. Include that it can take 6 months for a patient to notice heart failure symptom improvement and that heart failure medications are still necessary.
- Tell the patient and their family that it’s sometimes difficult to place the left ventricular lead and that the procedure can take 4 hours or more.
- Stress the importance of calling the practitioner immediately if the patient develops chest pain, shortness of breath, swelling of the hand s or feet, or a weight gain of 3 lb (1.4 kg) in 24 hours or 5 lb (2.3 kg) in 72 hours.
A Look at Implantable Cardioverter-Defibrillators
An ICD is an electronic device implanted in the body to provide continuous monitoring of the heart for bradycardia, VT, and ventricular fibrillation. The device then administers either override (antitachycardia) pacing beats or shocks to treat the dangerous arrhythmia. Implanted defibrillators are indicated for patients who have had a myocardial infarction and have an EF of 30% or less, or who have had nonsustained VT and an EF of 40% or less.
The placement and procedure for an ICD is usually similar to that of a permanent pacemaker and is usually inserted in an electrophysiology laboratory.
What It is
An ICD consists of a programmable pulse generator, a shocking lead, and one or more pacing leads. The pulse generator is a small battery-powered computer that monitors the heart’s electrical signals and delivers electrical therapy when it identifies an abnormal rhythm. The leads are insulated wires that carry the heart’s signal to the pulse generator and deliver the electrical energy from the pulse generator to the heart.
Storing and Retrieving Information
An ICD also stores information about the heart’s activity before, during, and after an arrhythmia, along with tracking which treatment was delivered and the outcome of that treatment. Devices also store electrograms (electrical tracings similar to ECGs). With an interrogation programmer, a specially trained practitioner can retrieve information to evaluate ICD function, battery status, and to adjust ICD system settings. Biventricular ICDs, like biventricular pacemakers, store information that aid in heart failure assessment.
Automatic Response
Today’s advanced devices can detect a wide range of arrhythmias and automatically respond with the appropriate therapy, such as bradycardia pacing (both single- and dual-chamber), biventricular pacing, antitachycardia pacing, cardioversion, and defibrillation. ICDs that provide therapy for atrial arrhythmias, such as atrial fibrillation, are also available. (See Types of ICD therapies.) All ICDs will temporarily pace postshock if necessary. Those with transvenous lead wires can also function as a typical pacemaker for chronic bradycardia needs and deliver antitachycardia pacing.
How It’s Programmed
When caring for a patient with an ICD, it’s important to know how the device is programmed. This information is available through a status report that can be obtained and printed when the specially trained practitioner interrogates the device. This involves placing a small piece of equipment on the skin, over the implanted pulse generator, to retrieve information. The stored information helps to evaluate any arrhythmias that the device was programmed to store, any therapy delivered, and device function.
Program information includes
- type and model of the ICD
- status of the arrhythmia detection device and therapy (on or off)
- heart rates and ECG morphology that result in a detected arrhythmia
- therapies that will be delivered: bradycardia pacing, antitachycardia pacing, cardioversion, and defibrillation.
Arresting Developments
Follow these guidelines if your patient experiences an arrhythmia:
- If the patient experiences cardiac arrest, initiate CPR and advanced cardiac life support.
- If the ICD delivers a shock while you’re performing chest compressions, you may also feel a slight shock. Wear gloves to prevent you feeling the shock.
- Externally defibrillating the patient is safe as long as the paddles aren’t placed directly over the pulse generator. The anteroposterior pad position is preferred.

Be Alert
Provide the same basic care for the patient with an ICD that you would for a patient with a permanent pacemaker. Frequently, patients who are biventricularly paced also have an ICD. Specific care for patients with ICDs includes the following:
- Monitor the patient’s rhythm for antitachycardia pacing or shocks.
- Patients post-ICD implant may be more sedated than postpacemaker because of the anesthesia administered so the patient does not feel or remember any testing shocks.
- Put the telemetry monitor in “Paced Mode.” All ICDs are programmed to pace once the patient’s own heart rate gets below the programmed set heart rate, for example, 40 bpm.
What to Teach the Patient
- Explain to the patient and their family why an ICD is needed, how it works, potential complications, and what they can expect. Make sure they also understand ICD terminology.
- Discuss signs and symptoms to report to the practitioner immediately.
- Explain actions patient should take if they receive a shock with and without symptoms or get multiple shocks. For example, call their cardiologist when they receive a shock and call 911 if they feel ill after a shock or get sequential shocks.
- Educate family members in emergency techniques (such as dialing 911 and performing CPR) in case the device fails to restore circulation.
- Advise patients to speak with their physician before operating a transport vehicle (e.g., car, bus, plane).
A Look at Radiofrequency Ablation
Radiofrequency ablation is an invasive procedure that may be used to treat arrhythmias in patients who haven’t responded to antiarrhythmic drugs or cardioversion or can’t tolerate antiarrhythmic drugs. In this procedure, bursts of radiofrequency energy are delivered through a catheter to the heart tissue to destroy the focus of the arrhythmia or block its conduction pathway.
Who’s a Cand idate?
Radiofrequency ablation is commonly used in treating patients with atrial tachycardia, atrial fibrillation, atrial flutter, AV nodal reentry tachycardia (AVNRT), inappropriate sinus tachycardia, bypass tracts like Wolff–Parkinson–White (WPW) syndrome, VT, and frequent premature ventricular contractions.
Understand ing the Procedure
The patient first undergoes an electrophysiology study to identify and map the specific areas of the heart that cause or support the arrhythmia. The ablation catheters are inserted into a vein, usually the femoral vein, and advanced into the heart where short bursts of radiofrequency waves destroy small targeted areas of heart tissue. The destroyed tissue can no longer conduct electrical impulses. Other types of energy may also be used, such as microwave, sonar, or cryo (freezing).
Hitting the Target
Arrhythmias can be categorized by being either focal or reentrant. Examples of focal arrhythmias include atrial tachycardia, inappropriate sinus tachycardia, premature atrial contractions, and right- or left ventricular outflow tract VT. The arrhythmia originates from one spot or foci. Reentrant arrhythmias include VT (other than outflow tract), atrial fibrillation, AVNRT, and accessory pathways like WPW syndrome. Reentrant arrhythmias are supported by abnormal conduction that typically is in a continuous circular path or circuit. Radiofrequency ablation is used to either destroy the source of a focal tachycardia or block the abnormal pathway of the reentrant conduction circuit. (See Destroying the source or the circuit)
If a rapid arrhythmia originates above the AV node, the bundle of His in the AV node may be purposefully damaged with ablation to block impulses from reaching the ventricles. This may be done to control the ventricular rate for patients whose intolerable atrial rhythm can’t be converted to sinus with chemical or electrical cardioversion or ablation. A permanent pacemaker would be necessary in tand em with this ablation. Also, anticoagulation therapy may be needed to reduce the risk of stroke.
If the patient has an accessory pathway as in WPW syndrome, electrophysiology studies are used to locate the accessory pathway and ablation can destroy the circuit.
After an ablation, one’s heart rate and /or rhythm should return to normal. Thus, ablation can prevent tachycardia-mediated cardiomyopathy and may restore ventricular pumping function that has been damaged by the effects of prolonged tachycardia. Some ablations can be lifesaving, like VT ablations.
How You Intervene

When caring for a patient after radiofrequency ablation, follow these guidelines:
- Provide continuous cardiac monitoring, assessing for arrhythmias and ischemic changes.
- Place the patient on bed rest as ordered and keep the affected extremity straight. For example, when a figure-of-eight suture is used, patients usually remain flat for 4 hours after the suture is placed. Maintain the head of the bed between 15 and 30 degrees.
- Assess the patient’s vital signs every 15 minutes for the first hour, then every 30 minutes for 4 hours, unless the patient’s condition warrants more frequent checking.
- Assess peripheral pulses distal to the catheter insertion site as well as the color, sensation, temperature, and capillary refill of the affected extremity.
- Check the catheter insertion site for pain, bleeding, bruit, and hematoma formation.
- Medicate for pericardial discomfort.
- Monitor the patient for complications, such as hemorrhage, retroperitoneal bleed, access site hematoma or pseudoaneurysm, stroke, perforation of the heart, cardiac tamponade, phrenic or vagus nerve damage, pericarditis, atrial–esophageal fistula, pulmonic vein stenosis, heart failure, thrombosis, arrhythmias, and sudden death.
What to Teach the Patient
When a patient undergoes radiofrequency ablation, be sure to cover these points:
- Discuss with the patient and their family why radiofrequency ablation is needed, how it works, and what they can expect.
- Warn the patient and their family that the procedure can be lengthy: an average of 6 hours.
- Explain that the patient may be hospitalized for 24 hours to monitor their heart rhythm and monitor and /or remove intravascular and potential pericardial fluid.
- Advise the patient to continue prescribed medication exactly as directed, especially anticoagulation for stroke prevention. Postdischarge calls to patients can confirm this.
- Have the patient (1) return demonstrate taking their pulse, (2) describe what an irregular, fast, or slow pulse feels like, (3) state actions to take with an abnormal pulse.
- Advise the patient to call the team who performed the ablation with any signs or symptoms of complications, such as shortness of breath or edema caused by fluid overload. An extremely rare but often fatal complication of atrial fibrillation ablation is an atrial–esophageal fistula that can cause hemoptysis, fever, malaise, or dysphagia.
- Explain rationale for temporary limitations per the cardiology team, such as in driving, upper endoscopy, or vigorous activity.
- Provide implanted device teaching if the patient had a pacemaker or ICD inserted. (For more information about pacemaker teaching, see What to teach the patient, page 205.)
Subcutaneous implantable cardioverter-defibrillator
- Subcutaneous system that defibrillates VT and ventricular fibrillation
- Main advantage is avoidance of vascular access and associated complications
- Patients must meet selection criteria prior to implant: ECG morphology and no need for bradycardia pacing, antitachycardia pacing or resynchronization therapy
Test Strip
Time to try out a test strip. Ready? Go!
In the following ECG strip, the pacemaker is pacing and sensing the ventricles with 100% capture. The mode of response can’t be evaluated because of lack of intrinsic activity. You would determine that the patient probably has:
a VVI pacemaker.
a DDD pacemaker.
an AAI pacemaker.
an AOO pacemaker.
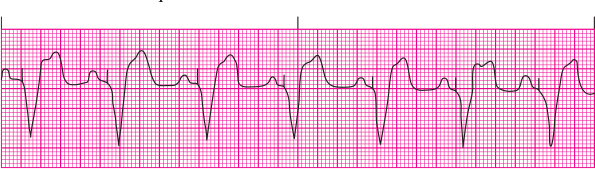
Answer: B. The patient has a DDD pacemaker. It senses atrial activity and therefore inhibits atrial pacing. The P wave then triggers the pacemaker to try to sense a QRS complex. Because there is no intrinsic QRS complex after the P wave, the pacemaker paces the ventricle.