AUTHORS: Nathan Stanford, MD and Alan Taylor, MD
Chalazion is one of the most common, usually noninfectious inflammatory lesions of the eyelid, accounting for approximately 13% of all benign eyelid lesions. These lesions typically present as localized areas of painless swelling and feel like a rubbery nodule to palpation.1 Diagnosis is based on clinical appearance. Chalazia are formed due to a granulomatous inflammatory reaction secondary to leakage of the lipid content of an obstructed Zeis or meibomian gland into the surrounding tarsal plate. While it is possible that an infection can cause the obstruction that leads to chalazion, the chalazion itself is an inflammatory reaction. This results in a sterile, painless lesion, which grows over weeks to months. These can eventually become infected and painful if not treated.
| ||||||||||||||||||||||||||||||||||||
- Prior chalazion
- Recent conjunctivitis or poor lid hygiene
- Acne rosacea
- Chronic blepharitis
- Vitamin A deficiency
- With the 2020 COVID-19 pandemic, facemask use has been shown to be a risk factor for chalazion formation2
- Painless localized nodule on the eyelid (Fig. E1).
- Lesion will be firm and rubbery.
- Possible impaired vision depending on size of lesion.
- Increased swelling for weeks or months.
- Can become inflamed, painful, or infected.
- Can be visualized on the external eyelid or internal eyelid.
- Duration usually longer than 2 wk compared to styes, which usually have a shorter course.3
- Typically, benign and self-limited lesion. If persistent or recurrent, a chalazion should be evaluated for malignancy.
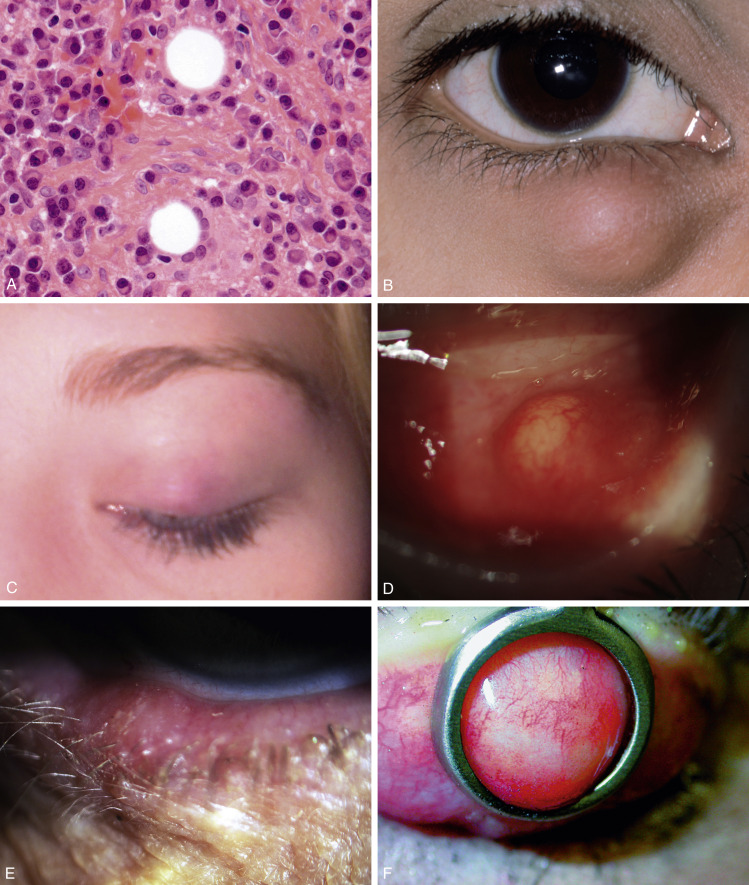
A, Histopathology Shows a Lipogranuloma; the Large Pale Cells are Epithelioid Cells and the Well-Demarcated Empty Space Contained Fat Dissolved Out During the Processing. B, Uninflamed Chalazion. C, Acutely Inflamed Lesion. D, Conjunctival Granuloma. E, Marginal Chalazion. F, Conjunctival View of Chalazion Clamp in Place Before Incision and Curettage.
A, Courtesy of J. Harry and G. Misson, from Harry J, Misson G: Clinical ophthalmic pathology: principles of diseases of the eye and associated structures, Boston, 2001, Butterworth-Heinemann. F, from Nerad J et al: Rapid diagnosis in ophthalmology: oculoplastic and reconstructive surgery, St Louis, 2008, Mosby. From Bowling B: Kanski’s clinical ophthalmology, a systemic approach, ed 8, Philadelphia, 2016, Elsevier.
Chalazia appear as small, red, rubbery nodules that are caused by local inflammation and obstruction of the sebaceous glands of the eyelids.1 Obstruction of the sebaceous glands results in lipid buildup and stasis. The lipid breakdown byproducts incite localized inflammation, which then recruits white blood cells to the area.