AUTHORS: Betelhem Kifle, MD and Lekshmi Santhosh, MD, MAEd




DefinitionViral pneumonia is a lung infection caused by any of a large number of viral pathogens. Some of the most important viruses are discussed in this chapter.
SynonymsViral pneumonia
Nonbacterial pneumonia
| ICD-10CM CODES | | J12.9 | Viral pneumonia, unspecified | | J12.89 | Other viral pneumonia |
|
Epidemiology & DemographicsIncidence (in U.S.)
- COVID-19 (SARS-CoV-2 virus):
- The novel coronavirus disease (COVID-19) was first detected in December 2019 and became a worldwide pandemic in 2020. (See “COVID-19 Disease” and “COVID-19 Cardiac Effects” chapters for further information.)
- Influenza virus:
- The CDC estimated ∼13 million illnesses, ∼6.1 million medical visits, 170,000 hospitalizations, and ∼14,000 deaths caused by influenza in the 2021 to 2022 influenza season.1
- Secondary bacterial pneumonia develops in a small percentage of infected persons.
- Incidence of other important viral pathogens can vary widely depending on setting, geography, and testing modalities. With the more widespread use of rapid molecular testing of respiratory secretions, an increase in the detection of viral pathogens has been observed. However, determining causality of the identified virus to the suspected pneumonia remains challenging because respiratory viruses remain detectable for several weeks after initial infection, and the pneumonia may be due to secondary bacterial infection.
Prevalence (in U.S.)
- Often related to immune status of the population or presence of an epidemic/pandemic
- Normal hosts (estimates):
- Viral pneumonia requiring children’s hospitalization accounts for ∼66% cases.
- Viruses have been detected in ∼23% of adults with clinical pneumonia.
Predominant Sex
- Equal predominance.
- Male sex may predispose to more severe respiratory disease in RSV infection.
- Case fatality ratio of COVID-19 is greater among men than among women.
Predominant Age
- COVID-19:
- Hospitalizations and deaths increase with age
- More prevalent in adults >30 yr
- Influenza:
- Overall incidence greatest in children <5 yr
- In general, lower incidence with increasing age
- Hospitalizations are greatest in infants and children aged <5 yr and adults aged >64 yr
- Mortality is greater in adults >64 yr
- RSV and parainfluenza virus:
- Young children (as the major cause of pneumonia)
- Occurs throughout life
- Human metapneumovirus:
- Children: Peak incidence 11 mo
- Increasingly detected in adults (bronchitis, chronic obstructive pulmonary disease [COPD] exacerbation, pneumonia)
- Frequent cause of lower respiratory tract infection (LRTI) in lung transplant recipients
- Adenoviruses:
- Young children
- Adults, primarily military recruits
- Varicella:
- Approximately 16% of adults (not infected in childhood) who contract varicella develop pneumonia
- Acute varicella during pregnancy is more likely to be complicated by severe pneumonia
- 90% of reported varicella pneumonia cases are in adults (highest incidence ages 20 to 60 yr)
- Measles:
- Young adults and older children who only received a single vaccination (5% failure rate)
- Currently most cases are seen in unvaccinated individuals
- Measles during pregnancy more likely to be complicated by pneumonia
- Underlying cardiopulmonary diseases and immunosuppression predispose to serious pneumonia
- Before availability of measles vaccine, 90% of pneumonias in those <10 yr
- ∼6% of measles cases are complicated by pneumonia
- Cytomegalovirus (CMV):
- Neonatal through adult
- Immunosuppression is key predisposing factor
- Hematopoietic stem cell transplant recipients are at highest risk
Peak Incidence
- COVID-19:
- Onset in December 2019 without clear seasonal variation
- Influenza:
- Winter months for influenza A
- Year-round for influenza B
- Peak of pneumonia seen weeks into the outbreak of infection
- Respiratory syncytial virus (RSV) and parainfluenza virus: Winter and spring
- Human metapneumovirus: Winter months
- Adenovirus: Endemic (military)
- Varicella: Spring in temperate zones
- Measles: Year-round
- Cytomegalovirus (CMV): Year-round
GeneticsFamilial disposition:
- Close contact, not genetics, is important in acquisition
- Congenital anomalies and immunosuppression worsen course of RSV pneumonia
Congenital infection:
- CMV is the most common intrauterine infection in the U.S.
- Pneumonia occurs occasionally in infants with symptomatic congenital infection
Neonatal infection:
- Severe RSV pneumonia
- Adenovirus pneumonia
- 5% to 20% mortality rate
- Can lead to residual restrictive or obstructive functional abnormalities
- “Varicella neonatorum”
- Disseminated visceral disease including pneumonia
- May develop in neonates whose mothers develop peripartum chickenpox
- CMV pneumonia:
- Generally fatal
- Associated with severe cerebral damage in this population
Physical Findings & Clinical Presentation
- COVID-19: Wide range, from mild symptoms to severe illness
- Fever, chills, fatigue, myalgias, headache
- Cough, shortness of breath, sore throat, congestion, rhinorrhea
- Loss of taste or smell
- Nausea, vomiting, diarrhea
- Influenza:
- Fever, cough, or sore throat (referred to as influenza-like illness [ILI])
- Uncomfortable or lethargic appearance
- Prominent dry cough (rarely hemoptysis)
- Flushed skin and erythematous mucous membranes
- Rales or rhonchi
- RSV, parainfluenza, and human metapneumovirus:
- Fever
- Tachypnea
- Prolonged expiration
- Wheezes and rales
- Diarrhea2
- Adenoviruses:
- Hoarseness, pharyngitis
- Conjunctivitis
- Tachypnea
- Cervical adenitis
- Measles:
- Conjunctivitis
- Rhinorrhea
- Koplik spots (white lesions on the buccal mucosa)
- Exanthem (maculopapular rash that starts on the head, then moves down to rest of body)
- Pneumonitis (coincident with rash, may also develop after apparent recovery from measles)
- Fever
- Dry cough
- Varicella:
- Fever
- Maculopapular or vesicular rash (all lesions at the same stage) becomes encrusted
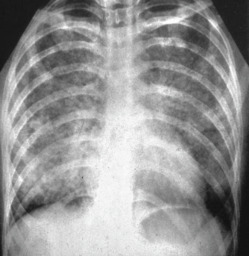
- Pneumonia typically 1 to 6 days after rash appears. Pneumonia (Fig. E1) may be accompanied by cough and occasionally hemoptysis
- Few auscultatory abnormalities noted on examination of the lungs
- CMV:
- Fever
- Paroxysmal cough
- Occasional hemoptysis
- Diffuse adenopathy when pneumonia occurs after transfusion
- Severe immunosuppression associated with symptomatic CMV pneumonia (may be reactivation of latent infection or in previously seronegative recipients from the donor)
Figure E1 This Chest Radiograph Demonstrates Bilateral Nodular and Interstitial Pneumonia Characteristic of Varicella Pneumonia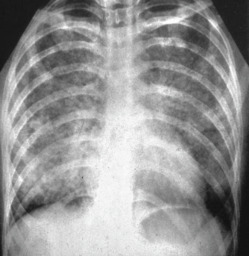
The patient, a 27-yr-old gravida 6, para 2, abortus 3, was exposed to varicella infection in her two children. Characteristic skin vesicles of varicella occurred several days before the development of pulmonary symptoms. She required endotracheal intubation and mechanical ventilation for 6 days. She was treated with intravenous acyclovir and ceftazidime for possible superimposed infection. The patient recovered fully and delivered a healthy infant at term.
From Gabbe SG: Obstetrics, ed 6, Philadelphia, 2012, Saunders.
EtiologyViral infection can lead to pneumonia in both immunocompetent and immunocompromised hosts.