AUTHOR: Daniel K. Asiedu, MD, PhD, FACP
- Vitamin D is a hormone and a steroid and, by definition, not a vitamin. There are two forms of vitamin D: Vitamin D2 and vitamin D3.
- Vitamin D2 (ergocalciferol) is mainly found in some plant foods.
- Vitamin D3 (cholecalciferol) is produced in skin exposed to ultraviolet (UV) B radiation from sunlight (Fig. E1). Gloson, Whistler, and DeBoot independently described rickets in the mid-seventeenth century. Sniadecki first reported the association of rickets with inadequate exposure to sunlight in 1822.
- The major functions of vitamin D include:
- Increasing calcium, magnesium, and phosphorus absorption from the small intestines
- Promoting the maturation of osteoclast to resorb calcium from bones
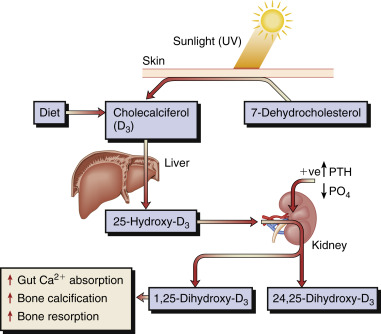
Figure E1 The metabolism and actions of vitamin D.
The primary source of vitamin D in humans is photoactivation in the skin of 7-dehydrocholesterol to cholecalciferol, which is then converted first in the liver to 25-hydroxyvitamin D and subsequently in the kidney to the much more active form, 1,25-dihydroxycholecalciferol (1,25[OH]2,D3). Regulation of the latter step is by parathyroid hormone (PTH), phosphate (PO4), and feedback inhibition by 1,25(OH)2,D3. This step can also occur in lymphomatous and sarcoid tissue, resulting in the hypercalcemia that may complicate these diseases. UV, Ultraviolet.
From Ballinger A: Kumar & Clark’s essentials of clinical medicine, ed 6, Edinburgh, 2012, Saunders.
Vitamin D deficiency is characterized by hypocalcemia and/or hypophosphatemia leading to impaired bone mineralization. It is classified as a serum 25-hydroxyvitamin D (25[OH]D) level of <20 ng/ml (50 nmol/L). This standard definition of vitamin D deficiency has been recently challenged, and some endocrinologists recommend a cutoff of 12 mg/ml for vitamin D deficiency. Vitamin D insufficiency is defined as a 25(OH)D between 12 and 20 ng/ml.
The consequences of vitamin D deficiency include:
- Bone disease (rickets, osteoporosis, low bone mass)
- May impair reproductive success
- Decrease the ability to combat infection (especially tuberculosis, influenza, viral infection)
- May induce or worsen autoimmune disorders
- May increase the incidence of death due to heart disease, inflammatory bowel disease, fracture, and cancer of the breast, colon, and prostate
- Subclinical vitamin D deficiency may occur in developed countries and be associated with increased fall risk and osteoporosis
- Vitamin D insufficiency is very high among older adults and hospitalized and institutionalized people.
- Worldwide deficiency and insufficiency affect about 1 billion people.
- Children and young adults: 40% to 50% of preadolescent Caucasian girls, and Hispanic and African American adolescents, are vitamin D deficient.
In the U.S., 40% to 100% of the elderly are vitamin D deficient.
Sixty percent of nursing home residents may be vitamin D deficient.
- Age (due to decreased ability to produce D3)
- Sunshine-deficient areas (geographic location, living in higher latitudes)
- Dark-skinned individuals (melanin competes with vitamin D3 precursors for UV photons and thus decreases pre-D3 formation)
- Obese individuals
- Institutionalized individuals
- Pregnant and lactating women
- Use of sunscreen (sun radiation that causes skin cancer also produces pre-vitamin D3 in skin)
- Patients on certain medications that antagonize vitamin D action (phenobarbital, phenytoin)
- Intestinal resection
- Severe chronic liver diseases (such as cirrhosis)
- Kidney disease (e.g., nephritic syndrome)
- Sarcoidosis and lymphomas (increased catabolism of 25[OH]D to 1,25[OH]2D)
- Intestinal malabsorption disease (caused by celiac sprue, cystic fibrosis, Whipple disease)
- Clinical presentation of vitamin D deficiency is dependent on the duration and severity of deficiency
- Most patients with mild to moderate vitamin D deficiency are asymptomatic
- Severe deficiency may lead to rickets (in children), osteomalacia (in adults), bone demineralization, hypokalemia, and phosphaturia
- Mild deficiency can lead to hypocalcemia and hyperparathyroidism
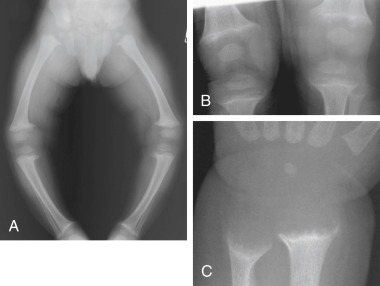
- Rickets: Seen in children; caused by defective mineralization in the skeleton (Fig. E2)
- Osteomalacia: Seen in adults with severe and prolonged vitamin D deficiency
- Fracture with very minimal trauma (brittle and easily broken bones)
- Severe hypocalcemia: Especially in late vitamin D deficiency leading to seizure tetany
- Hypophosphatemia
- Paresthesia
- Tetany
- Muscle cramps
- Inadequate exposure to sunlight, such as:
- Medications: Individuals on certain medications, such as phenobarbital, phenytoin, and rifampin (antagonize vitamin D action/increase vitamin D catabolism)
- Diseases and disease states: