AUTHORS: Michael J. Farias, BS and John D. Milner, MD and Manuel F. DaSilva, MD
Rickets is a result of deficient mineralization of osteoid matrix before closure of the epiphyseal plate causing softening and weakening of bones in infants and children. The mineralization impairment may be secondary to abnormal calcium, phosphorus, or vitamin D metabolism leading to accumulation of osteoid before epiphyseal closure, compromising bone stability at sites of rapid bone growth.1 When this occurs in adulthood after epiphyseal closure, it is referred to as osteomalacia. Renal osteodystrophy is a term used to describe a similar condition in patients with chronic kidney disease. Certain forms of the disorder may respond only to high doses of vitamin D and are referred to as vitamin D-resistant rickets (VDRR).2
| ||||||||||||||||||||
- Children ages 6 to 24 mo
- Premature infants
- Residents of northern latitudes with inadequate sunlight exposure
- Solely breastfed infants
- Darker skin pigmentation
- Use of anticonvulsants3
The classic clinical presentation of children with rickets includes:
- Apathy, muscle weakness, muscle cramps, delayed growth and short stature
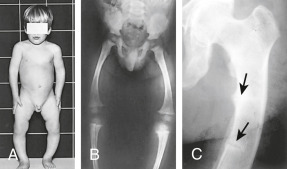
- Skeletal pain and swollen joints (Figs. E1 and E2)
- Protuberant abdomen due to muscle hypotonia4
- Widened sutures, delayed closure of fontanelles, and frontal bossing of head1
- Craniotabes (softening of skull bones)4
- Delayed eruption of teeth and poorly mineralized teeth4
- Bowing deformity of lower extremities, specifically femur and tibia (Fig. E3)
- Table E1 summarizes clinical features of rickets
- Rachitic rosary (enlargement and prominence of the rib head at the costochondral junctions)1
- Harrison groove (indentation of the lower ribs)1
- Breastbone that is pushed forward (pigeon chest)5
- Pathologic fractures
- Scoliosis or kyphosis
The less pronounced clinical presentation of adults with osteomalacia includes:4
- Skeletal pain and bone tenderness
- Muscle hypotonia and proximal muscle weakness
- Pathologic fractures and decreased bone density
- Gait disturbances
Figure E1 Rachitic “rosary” in a child with rickets.
Courtesy Dr. Thomas D. Thacher, Rochester, MN. In Kliegman RM: Nelson textbook of pediatrics, ed 21, Philadelphia, 2020, Elsevier.
From Bullough PG: Orthopaedic pathology, ed 5, St Louis, 2010, Mosby, Fig 8-31. In Kliegman RM: Nelson textbook of pediatrics, ed 21, Philadelphia, 2020, Elsevier.
Note the Bowing of the Femurs and Tibiae, Which May Result from Vitamin D Deficiency, Phosphate Deficiency, or Other Causes. (B) A Skeletal Radiograph of a Child with Rickets. Note that the Weight-Bearing Bones of the Lower Extremities are Bowed and that the Epiphyses are Open, Mottled, and Overgrown. (C) Looser Zones or Pseudofractures that are Characteristic of Osteomalacia or Rickets. Because the Epiphyses are Closed, the Patient is an Adult. This Radiograph is Diagnostic of Osteomalacia.
From Stewart A: Metabolic bone diseases. In Andreoli TE et al [eds]: Cecil essentials of medicine, ed 8, Philadelphia, 2010, Saunders.
TABLE E1 Clinical Features of Rickets
| General | |||
| Head | |||
| Chest | |||
| |||
| Back | |||
| Extremities | |||
| Hypocalcemic Symptoms† | |||
∗These features are associated most frequently with vitamin D deficiency disorders.
† These symptoms develop only in children with disorders that produce hypocalcemia.
The most common cause of rickets and osteomalacia is vitamin D deficiency. Insufficient calcium and phosphorus intake can also lead to rickets. Vitamin D and parathyroid hormone (PTH) play an important role in calcium homeostasis. Vitamin D is required for adequate calcium absorption in the gastrointestinal tract. Low vitamin D leads to reduced intestinal absorption of calcium, causing a compensatory increase in PTH and resorption of bone, leading to increased alkaline phosphatase levels.3 This may arise from various conditions including inadequate dietary intake, malabsorption, chronic parenteral nutrition, and the additional risk factors listed previously. Malabsorption that causes inefficient mineralization is observed in diseases such as cystic fibrosis, intestinal disorders such as celiac disease, and in many chronic illnesses, including severe liver disease.3
Chronic renal failure can produce bone mineralization deficiency due to electrolyte abnormalities causing hypocalcemia and renal osteodystrophy (renal rickets). This results in decreased excretion of phosphate, therefore elevating serum phosphorus, along with elevated PTH and low levels of 1,25-OH vitamin D.1
Other causes specifically include vitamin D-dependent rickets (VDDR type I and II) and VDRR, also known as hereditary hypophosphatemic rickets.4 (Table E2)
- VDDR type I (VDDR-1) results from mutations in the vitamin D 1-alpha hydroxylase enzyme that converts inactive vitamin D to the active metabolite of 1,25(OH)2D.
- VDDR type II (VDDR-II), also known as hereditary vitamin-D resistant rickets (HVDRR), results from defective vitamin D receptors due to a mutation in the vitamin D receptor gene (Table E3).
TABLE E2 Causes of Vitamin D-Deficiency Rickets or Osteomalacia, or Both
From Melmed S et al: Williams textbook of endocrinology, ed 14, 2019, Elsevier.
TABLE E3 Causes of Hypophosphatemic Rickets or Osteomalacia, or Both
| Genetic Autosomal dominant rickets Autosomal recessive rickets X-linked dominant rickets (X-linked hypophosphatemia) X-linked recessive Hypophosphatemic hypercalciuric hereditary rickets (or Dent disease) Neurofibromatosis Fibrous dysplasia Genetic Fanconi syndrome (may have renal failure) Acquired Tumor-induced osteomalacia (most common acquired cause) Renal tubular damage or nonfamilial Fanconi syndrome Drug induced |
From Melmed S et al: Williams textbook of endocrinology, ed 14, 2019, Elsevier.