AUTHOR: Daniel K. Asiedu, MD, PhD, FACP
Vitamins are organic compounds that cannot be synthesized by humans but are required as nutrients in minute amounts for normal metabolism. Vitamins have several different functions: They may regulate cell growth and differentiation, as catalysts, as antioxidants, and as coenzymes. Vitamins are classified as either fat soluble (vitamins A, D, E, K) or water soluble (B group of vitamins and C). Deficiency of most vitamins is rare in Western countries. Certain groups may be prone to vitamin deficiency, and these are discussed here. Vitamin D deficiency is discussed in a separate topic.
Vitamin K: Phytonadione or menadiol
Vitamin B1: Thiamine
Niacin: Vitamin B3; nicotinic acid
Vitamin B6: Pyridoxine; pyridoxal phosphate
Folic acid: Vitamin B9; folate
Vitamin B12: Cyanocobalamin
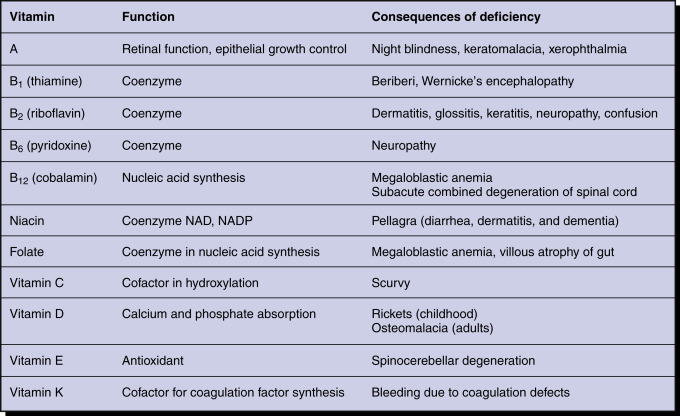
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
Deficiency can occur in all age groups but is most common in the elderly.
- Vitamin A deficiency: Affects 250 million preschool children worldwide.
- Vitamin E deficiency: Deficiency is rare in humans. Usually occurs in individuals with severe protein-energy malnutrition.
- Vitamin K deficiency: Varies by geographic regions; no race predilection; affects both sexes equally. Encountered often in infants. In normal healthy adults, 8% to 31% have vitamin K deficiency, but it rarely leads to significant bleeding.
- Vitamin B1 (thiamine) deficiency: Incidence is unknown; no sex, race, or age predilection. Deficiency is usually due to inadequate intake, especially if consuming diet made up of polished rice and grains.
- Vitamin B2 (riboflavin): More common than previously appreciated. Deficiency is referred to as ariboflavinosis.
- Vitamin B5 (pantothenic acid) deficiency: Rare, as it is present in all foods.
- Vitamin B12 (cobalamin) deficiency: Relatively common. Of patients with anemia, about 1% to 2% is due to B12 deficiency. Among patients with macrocytosis (mean corpuscular volume [MCV] >100) 18% to 20% is due to B12 deficiency. Occurs in all age groups but more common in the elderly. B12 deficiency due to pernicious anemia is common in Northern Europe.
- Vitamin B9 (folic acid) deficiency: Mandatory fortification started in 1998. Prevalence before fortification 16% and after 0.5%. Neural tube defect associated with low maternal folate status during pregnancy. Pregnant women and the elderly are at greatest risk of folic acid deficiency.
- Vitamin C (ascorbic acid) deficiency: Smokers and low-income persons are at increased risk. Vitamin C deficiency is associated with access to food and/or socioeconomic status. Prevalence vary worldwide, but the rate is about 7.1% in the U.S.
Fig. 1 shows environmental and nutritional factors in disease.
- Vitamin A: Xerophthalmia, xerosis of the cornea, keratomalacia, Bitot spots (abnormal squamous cell proliferation and keratinization of the conjunctiva), nyctalopia (poor adaptation to darkness)/night blindness, poor bone growth, dry skin and hair, follicular hyperkeratosis (caused by blockage of hair follicles by keratin), pruritus, broken fingernails
- Vitamin K: Clinical manifestation usually occurs if hypoprothrombinemia is present. Major symptom is bleeding to minor trauma. Also can show easy bruisability, epistaxis, hematoma, gum bleeding, melena, hematuria, or splinter hemorrhage
- Vitamin E: Neuromuscular disorders (ataxia; hyporeflexia, peripheral neuropathy); bone weakness, hemolysis
- Vitamin B1 (thiamine): Beriberi, which has two subtypes (infantile and adult). Adult type is described below:
- Dry beriberi (affecting the nervous system): Symmetrical peripheral neuropathy (with sensory and motor impairments), Wernicke encephalopathy (nystagmus, ataxia, ophthalmoplegia, and confusion), Korsakoff syndrome (impaired short-term memory loss and confabulation but normal cognition)
- Wet beriberi (affecting the cardiovascular system): Cardiomegaly, cardiomyopathy, heart failure, tachycardia, hypotension, chest pain, peripheral edema
- Gastrointestinal (GI): Anorexia; constipation
- Vitamin B2 (riboflavin):
- Vitamin B3 (niacin):
- Pellagra (4 Ds-diarrhea, dermatitis, dementia, and ultimately death)
- Hyperpigmentation of sun-exposed skin
- “Raw beef” swollen and painful tongue
- Deficiency can be seen in prolonged use of Isoniazid, in carcinoid syndrome, and in Hartnup syndrome
- Vitamin B5 (pantothenic acid):
- Vitamin B6 (Pyridoxine): Rare to see overt deficiency
- Vitamin B12 (cyanocobalamin):
- Megaloblastic anemia (pernicious anemia)
- Neurologic symptoms including peripheral neuropathy, ataxia (shuffling gait), paresthesia; subacute degeneration of the spinal cord (demyelination of the dorsal column), visual disturbances due to optic atrophy
- Glossitis and GI symptoms such as nausea, vomiting, and anorexia are also common
- Patients may also have dementia/mental sluggishness, depression, and weakness
- Vitamin B9 (folic acid):
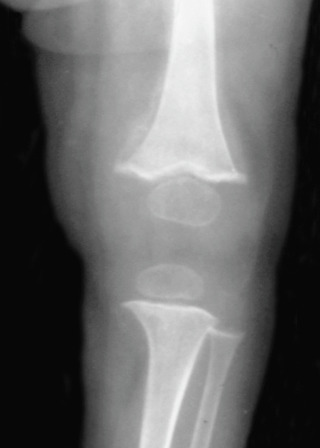
- Vitamin C: Scurvy (bruising, petechiae, follicular hyperkeratosis, perifollicular hemorrhage, corkscrew hairs), poor wound healing, fatigue, gingivitis/bleeding gums, weight loss, bone abnormalities (Fig. E2). Also, loss of teeth, abnormal nail (koilonychia and splint hemorrhages). Vitamin C deficiency may be associated with nonalcoholic fatty liver
The knee shows widened metaphyses with spurs and reduced bone density. The ossific centers have a typical “white pencil” outline. Faint periosteal reaction is visible in the distal femur secondary to periosteal hemorrhage. The end plate is still well defined, and the physis is not widened (compared with rickets). Fractures are rare.
From Pope TL et al: Musculoskeletal imaging, ed 2, Philadelphia, 2014, Saunders.
- Fat-soluble vitamins (vitamins A, D, E, K):
- Decreased ingestion, malnutrition, eating disorders
- Diseases that affect fat absorption decrease the absorption of fat-soluble vitamins-for example, cystic fibrosis, celiac sprue, inflammatory bowel disease, cholestasis, hepatobiliary disease, small bowel surgery
- Change in vitamin metabolism:
- Alcoholism
- Drugs such as cholestyramine, warfarin, anticonvulsants, antibiotics (e.g., cephalosporins)
- Chronic kidney disease
- Increased risk in:
- Water-soluble vitamins (the B group of vitamins and vitamin C)-there are several etiologic factors, including:
- Inadequate intake
- Decreased absorption
- Alcoholism
- Pregnancy/lactation
- Peritoneal dialysis
- Medications (e.g., isoniazid, phenothiazines, tricyclic antidepressants, metformin [vit B12])
- Malabsorption
- Low income
- Advanced age
- Vitamin B12 deficiency-caused by:
- Folic acid deficiency:
- Increased needs can lead to deficiency (e.g., pregnancy, lactation, malignancy)
- Derangement of folate metabolism by:
- Medication (e.g., methotrexate)
- Disease (e.g., hypothyroidism)
- Increased excretion: As seen in alcoholics