AUTHOR: Kathleen Doo, MD, MHPE
Hepatopulmonary syndrome (HPS) is defined by the presence of (1) liver disease (usually chronic), (2) reduced arterial oxygenation, and (3) evidence of intrapulmonary vascular dilations (IPVDs).1
4% to 47% of patients with cirrhosis;2 the wide range is due to lack of diagnostic criteria.
HPS occurs with any degree or etiology of liver disease but is more prevalent in patients with established cirrhosis and portal hypertension.
New data suggest that polymorphisms in genes involved in the regulation of angiogenesis are associated with increased HPS risk.3
- Dyspnea
- Platypnea: Increased dyspnea when sitting upright and relieved when supine
- Orthodeoxia: Decreased PaO2 (by more than 4 mm Hg) when sitting upright and improved when supine
- Increased spider nevi (spider angiomata)
- Signs of severe hypoxemia (e.g., cyanosis and clubbing of the digits)
- Table E1 describes a severity grading for HPS
TABLE E1 Grading of Severity of Hepatopulmonary Syndrome∗
| Stage | Alveolar-Arterial Po2 Difference | Arterial Partial Pressure of Oxygen |
|---|---|---|
| Mild | ≥15 mm Hg or >20 mm Hg if age >64 yr | ≥80 mm Hg |
| Moderate | ≥15 mm Hg or >20 mm Hg if age >64 yr | <80 to ≥60 mm Hg |
| Severe | ≥15 mm Hg or >20 mm Hg if age >64 yr | <60 to ≥50 mm Hg |
| Very severe | ≥15 mm Hg or >20 mm Hg if age >64 yr | <50 mm Hg |
∗All with positive contrast-enhanced echocardiography, breathing room air at rest and at sea level. From Broaddus VC et al: Murray & Nadel’s textbook of respiratory medicine, ed 7, Philadelphia, 2022, Elsevier.
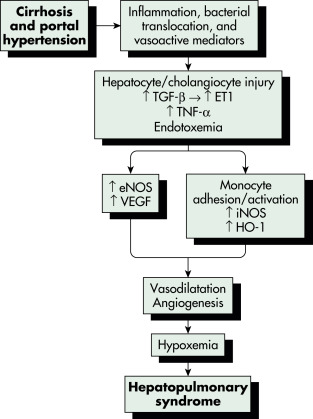
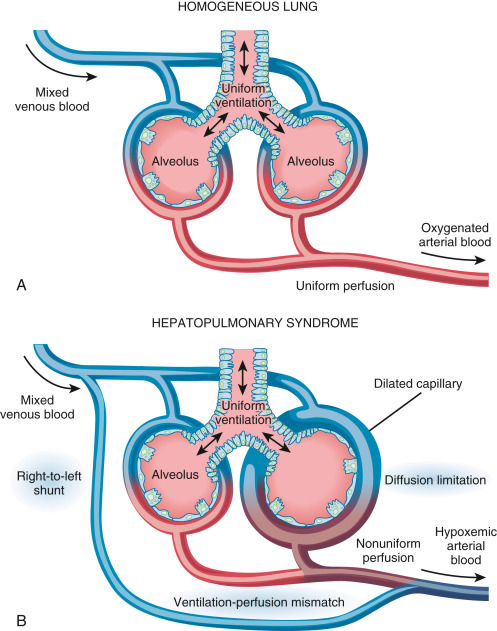
Dilation of intrapulmonary arterioles and dilated vascular channels between pulmonary arteries and veins leads to a ventilation-perfusion mismatch and right-to-left shunting. Research shows that nitric oxide (NO) plays a role in vasodilation.4 The relationship of vasodilation to liver disease is unclear. Fig. E1 illustrates a proposed pathophysiology of hepatopulmonary syndrome. In some patients, intrapulmonary shunting via dilated intrapulmonary vessels and pulmonary and pleural-based arteriovenous malformations can develop, resulting in worse hypoxemia and a blunted response to supplemental oxygen. A diffusion limitation has been postulated to be due to a “diffusion-perfusion defect” for oxygen in dilated pulmonary capillaries (Fig. E2). New areas of research include endothelin-1, which is produced by proliferating cholangiocytes, pulmonary angiogenesis, and opiate receptors’ influence on NO production.
Enos, Endothelial Nitric Oxide Synthase; Et1, Endothelin-1; Ho-1, Heme Oxygenase; Inos, Inducible Nitric Oxide Synthase; Tgf-, Transforming Growth Factor-; VEGF, Vascular Endothelial Growth Factor.

From Feldman M et al: Sleisenger and Fordtran’s gastrointestinal and liver disease, ed 10, Philadelphia, 2016, Elsevier.
(A) In the homogeneous lung of a healthy individual, with uniform alveolar ventilation and pulmonary blood flow, the capillary ranges between 8 and 15 μm in diameter, and oxygen diffuses properly into the capillary while ventilation-perfusion is well balanced. (B) In hepatopulmonary syndrome, where many capillaries are dilated and blood flow is nonuniform, alveolar ventilation-to-pulmonary perfusion mismatch emerges as the predominant mechanism at any clinical stage, either with or without the presence of intrapulmonary shunt and coexistent with oxygen diffusion limitation into the center of the dilated capillaries in the most advanced stages.
From Broaddus VC et al: Murray & Nadel’s textbook of respiratory medicine, ed 7, Philadelphia, 2022, Elsevier.