AUTHOR: Fred F. Ferri, MD
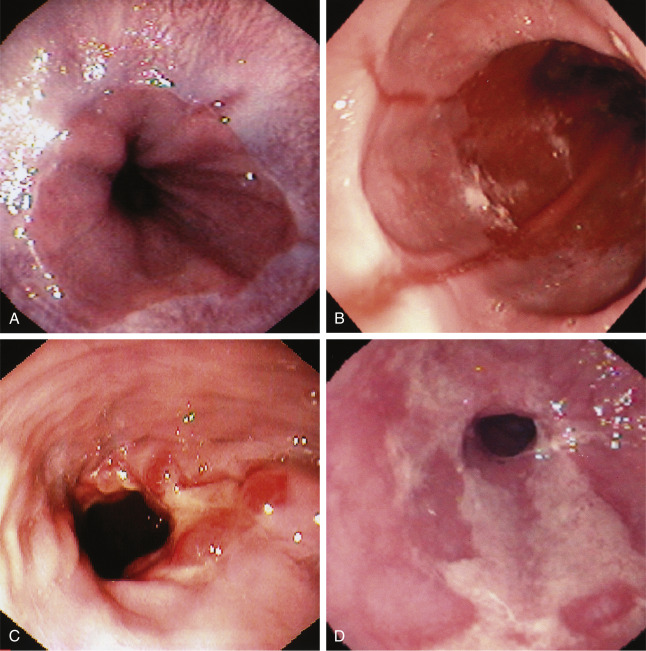
Gastroesophageal reflux disease (GERD) is a motility disorder characterized primarily by heartburn and caused by the reflux of gastric contents into the esophagus. A current definition is a condition that develops when the reflux of stomach contents causes at least two heartburn episodes per week and/or complications. Table 1 describes a classification system for esophagitis.
TABLE 1 Los Angeles Endoscopic Classification System for Esophagitis
| Grade A | One or more mucosal breaks confined to folds, ≤5 mm | ||
| Grade B | One or more mucosal breaks >5 mm confined to folds but not continuous between the tops of mucosal folds | ||
| Grade C | Mucosal breaks continuous between tops of two or more mucosal folds but not the circumferential | ||
| Grade D | Circumferential mucosal break |
From Feldman M et al: Sleisenger and Fordtran’s gastrointestinal and liver disease, ed 10, Philadelphia, 2016, Elsevier.
- GERD is one of the most prevalent gastrointestinal disorders. It is the most common GI diagnosis recorded during visits to outpatient clinics. From 18% to 28% of adults are affected.
- The estimated prevalence of GERD is 13.3% of the population worldwide and 15.4% in North America. Costs related to GERD in the U.S. are estimated at $10 billion annually.1
- Nearly 7% of persons in the United States have heartburn daily, 20% have it monthly, and 60% have it intermittently. Incidence in pregnant women exceeds 80%.
- Nearly 20% of adults use antacids or over-the-counter H2 blockers at least once a week for relief of heartburn.
- The phenotypic presentations of GERD include nonerosive reflux disease (in 60% to 70% of patients), erosive esophagitis (in 30%), and Barrett esophagus (in 5% to 12%).1
- Physical examination: Generally unremarkable
- Clinical signs and symptoms: Heartburn, dysphagia, sour taste, regurgitation of gastric contents into the mouth
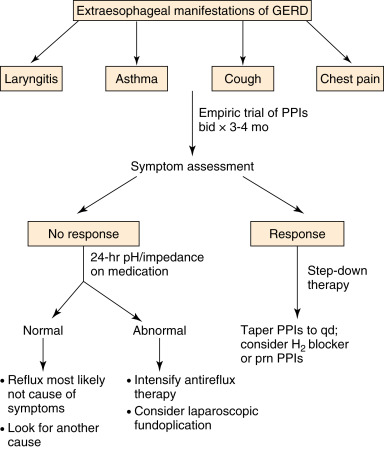
- Chronic cough and bronchospasm
- Chest pain, laryngitis, early satiety, abdominal fullness, and bloating with belching
- Dental erosions in children
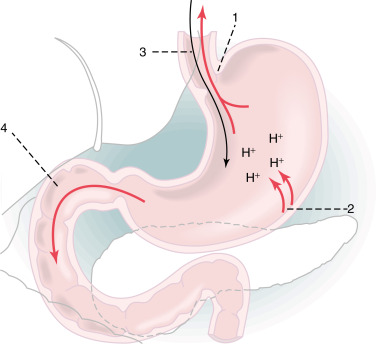
- Incompetent lower esophageal sphincter (LES) (see Fig. E1)
- Medications that lower LES pressure (calcium channel blockers, alpha-adrenergic antagonists, nitrates, theophylline, anticholinergics, sedatives, prostaglandins)
- Foods that lower LES pressure (chocolate, yellow onions, peppermint). Table 2 summarizes modulators of lower esophageal sphincter (LES) pressure
- Tobacco abuse, alcohol, coffee
- Pregnancy
- Gastric acid hypersecretion
- Hiatal hernia (controversial) present in >70% of patients with GERD; however, most patients with hiatal hernia are asymptomatic
- Obesity is associated with a statistically significant increase in the risk for GERD symptoms, erosive esophagitis, and esophageal carcinoma
TABLE 2 Modulators of Lower Esophageal Sphincter (LES) Pressure
| Increase LES Pressure | Decrease LES Pressure | |
|---|---|---|
| Hormones/peptides | Gastrin | CCK |
| Motilin | Secretin | |
| Substance P | Somatostatin | |
| Vasoactive intestinal peptide | ||
| Neural agents | α-Adrenergic agonists | α-Adrenergic antagonists |
| β-Adrenergic antagonists | β-Adrenergic agonists | |
| Cholinergic agonists | Cholinergic antagonists | |
| Foods and nutrients | Protein | Chocolate |
| Fat | ||
| Peppermint | ||
| Other factors | Antacids | Barbiturates |
| Baclofen | Calcium channel blockers | |
| Cisapride | Diazepam | |
| Domperidone | Dopamine | |
| Histamine | Meperidine | |
| Metoclopramide | Morphine | |
| Prostaglandin F2α | Prostaglandins E2 and I2 | |
| Serotonin | ||
| Theophylline |
CCK, Cholecystokinin.
From Feldman M et al: Sleisenger and Fordtran’s gastrointestinal and liver disease, ed 10, Philadelphia, 2016, Elsevier.
From Andreoli TE et al: Andreoli and Carpenter’s Cecil essentials of medicine, ed 8, Philadelphia, 2010, WB Saunders.