AUTHOR: Fred F. Ferri, MD
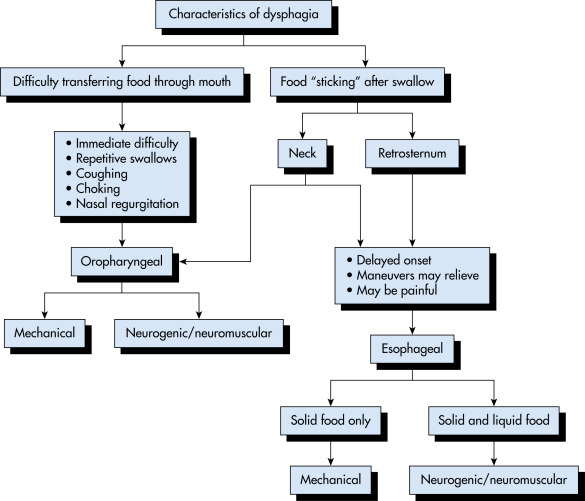
The term “dysphagia” is derived from the Greek words dys (with difficulty) and phagia (to eat). It is characterized by abnormal transfer of food from mouth to the stomach, which may involve the oral, pharyngeal, or esophageal stages of swallowing.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- This is seen in 10% of individuals above the age of 50 yr. Its prevalence increases with advancing age.
- Nearly 12% of hospitalized patients have symptoms of dysphagia.
- Up to 30% to 60% of nursing home patients have some form of dysphagia.
- Special populations, including patients with head injury, stroke, or Parkinson disease, have 30% to 50% prevalence of oropharyngeal dysphagia.
- Oropharyngeal:
- Esophageal:
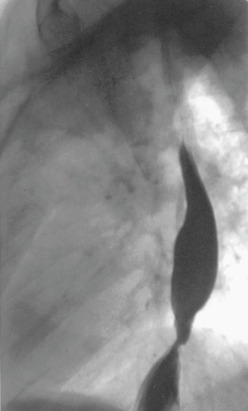
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia, 2022, Elsevier.
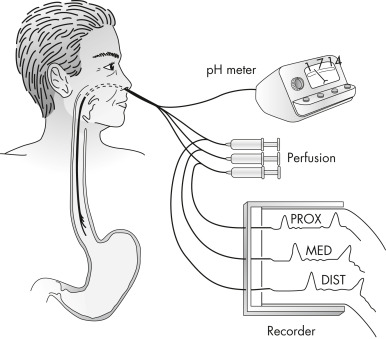
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia, 2022, Elsevier.
The inability to swallow is caused either by a problem in strength or coordination of the muscles required to move material from the mouth to stomach or by a fixed obstruction somewhere between the mouth and the stomach.
Oropharyngeal dysphagia (transfer dysphagia):
- The patient is unable to transfer the food bolus from the mouth to the upper esophagus. Problem arises within 2 sec of initiating the voluntary phase of swallowing.
- Typical symptoms include drooling, spillage of food, postnasal regurgitation, difficulty in initiation of swallowing, sialorrhea, sensation of food stuck in the neck, coughing or choking during swallowing, the need to swallow repeatedly to clear food or fluid from the pharynx, dysphonia, nasal speech, hoarseness of voice, and dysarthria.
- A thorough physical examination including that of the nervous system, oral cavity, and the head/neck is very important in patients with oropharyngeal dysphagia.
- Problem usually arises several seconds after swallowing.
- Patients often complain of food being stuck in lower substernal area.
- Dysphagia to solids suggests mechanical obstruction whereas dysphagia with liquids or combination of solids and liquids favors a motility disorder.
- Neuromuscular causes result in dysphagia to both solids and liquids. Particularly, patients with achalasia tend to drink a lot of fluids while eating or apply maneuvers such as straightening the back, raising their arms over their heads, or standing to increase intraesophageal pressure to facilitate the emptying of food into the stomach.
- Oftentimes, ingestion of very cold or very hot foods precipitates the dysphagia associated with neuromuscular disorder.
- Delayed regurgitation of food, heartburn, and chest pain are usually present.
- Weight loss is usually associated with malignancy or achalasia.
- Symptoms are intermittent in patients with esophageal dysphagia from benign causes of structural obstruction or diffuse esophageal spasm. However, it is progressive in patients with peptic stricture, esophageal carcinoma, scleroderma, and achalasia.
- In patients with structural obstruction, when the luminal diameter is more than 18 to 20 mm, they are rarely symptomatic, whereas those with a diameter of less than 13 mm are nearly always symptomatic.
- These patients with esophageal dysphagia usually do not have any characteristic physical findings.