AUTHOR: Corey Elam Goldsmith, MD, FAAN
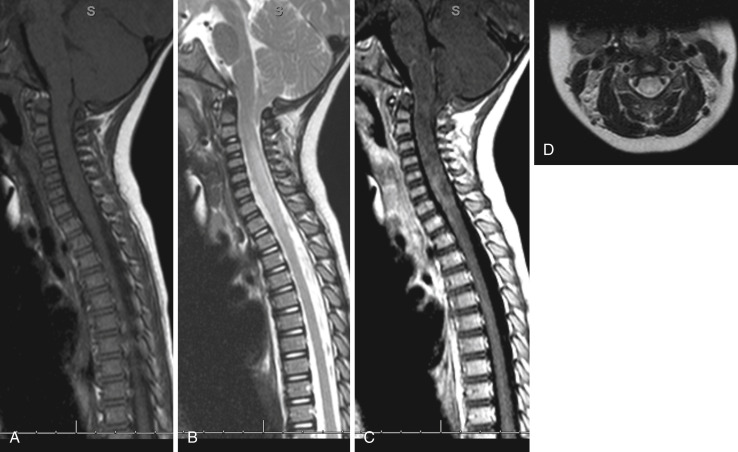
Demyelination in a transverse region of the spinal cord due to an inflammatory process that leads to sensory and motor changes below the lesion and autonomic dysfunction. The term “transverse myelitis” (TM) of late refers to any cause of inflammatory myelopathy, irrespective of severity or degree of structural or functional interruption of pathways through a transverse spinal cord section. TM that extends across three or more segments of the cord is referred to as longitudinally extensive TM. The pathologic hallmark of TM is the presence of focal collections of lymphocytes and monocytes with varying degrees of demyelination, axonal injury, and astroglial and microglial activation within the spinal cord.
Idiopathic transverse myelitis (ITM)
| ||||||||||||
Annual incidence ranges from 1.3 to 8 cases per million. The incidence increases to 24.6 cases per million annually if causes of acquired demyelination such as multiple sclerosis (MS) or neuromyelitis optic spectrum disorder are included.1,2
None, but female preponderance seen in cases associated with MS and neuromyelitis optica spectrum disorder (NMOSD).
- Rapid onset of symmetric or asymmetric paraparesis or paraplegia of the lower extremities over a few days, ascending paresthesia, sensory level at the trunk, back pain, sphincter dysfunction, and positive Babinski, which can be bilateral. The arms may also be involved if the cervical cord is involved, but cervical involvement is less common than thoracic involvement. In the acute phase the weakness is flaccid, with diminished deep tendon reflexes mimicking a peripheral neuropathy such as Guillain-Barré syndrome.
- One third to half of patients present with localizing back pain or a bandlike area of altered sensation, usually at the dermatomal level corresponding to the lesion within the cord.
- There is progression to nadir of clinical deficits between 4 h and 21 days after symptom onset.
- Urinary incontinence or retention, GI disturbances (incontinence or constipation), and sexual dysfunction are common.
- Acute flaccid myelitis is a subtype of myelitis in which patients present with acute limb weakness and have primarily involvement of gray matter on spinal cord imaging.
- The clinical signs are caused by an interruption in ascending and descending sensory, motor, and autonomic pathways in the transverse plane of the spinal cord, resulting in sensory-level weakness and autonomic dysfunction at and below the level of the lesion due to demyelination or inflammation of the spinal cord.
- Can be idiopathic demyelination (15% to 30%) that is a monophasic one-time event or demyelination secondary to neurologic or systemic conditions (Box 1).
- Secondary causes include postinfection, postvaccination, acute demyelinating encephalomyelitis (where TM tends to be monophasic), and others such as MS, NMOSD, connective tissue disorders such as systemic lupus, Sjögren syndrome, antiphospholipid antibody syndrome, sarcoidosis, and paraneoplastic conditions, which can be progressive or relapsing.1-4
- Infectious causes of myelitis include HIV, syphilis, varicella zoster (associated with shingles), human T-cell leukemia virus type 1, Lyme disease, COVID-19, arboviruses such as West Nile virus (typically causing a poliomyelitis-type acute flaccid paralysis), or enteroviruses (typically causing acute flaccid paralysis mainly in children).4
- About 50% of patients have had a recent upper respiratory infection.