AUTHOR: Fred F. Ferri, MD
Thyroiditis is an inflammatory disease of the thyroid. It is a multifaceted disease with various etiologies, different clinical characteristics (depending on the stage), and distinct histopathology. Thyroiditis can be subdivided into three common types (Hashimoto, painful, and painless) and two rare forms (suppurative and Riedel). To add to the confusion, there are various synonyms for each form, and there is no internationally accepted classification of autoimmune thyroid disease.
Hashimoto thyroiditis: Chronic lymphocytic thyroiditis, chronic autoimmune thyroiditis, lymphadenoid goiter
Painful subacute thyroiditis: Subacute thyroiditis, giant cell thyroiditis, de Quervain thyroiditis, subacute granulomatous thyroiditis, pseudogranulomatous thyroiditis
Painless postpartum thyroiditis: Subacute lymphocytic thyroiditis, postpartum thyroiditis
Painless sporadic thyroiditis: Silent sporadic thyroiditis, subacute lymphocytic thyroiditis
Infectious thyroiditis: Acute suppurative thyroiditis, bacterial thyroiditis, microbial inflammatory thyroiditis, pyogenic thyroiditis
Riedel thyroiditis: Fibrous thyroiditis
| ||||||||||||||||||||||||
- Thyroiditis typically has three phases: Thyrotoxic and hypothyroid (each lasting approximately 3 mo) and return to euthyroidism.
- Hashimoto: Patients may have signs of hyperthyroidism (tachycardia, diaphoresis, palpitations, weight loss) or hypothyroidism (fatigue, weight gain, delayed reflexes) depending on the stage of the disease. Usually there is diffuse, firm enlargement of the thyroid gland; the gland may also be of normal size (atrophic form with clinically manifested hypothyroidism).
- Painful subacute: Exquisitely tender, enlarged thyroid, fever; signs of hyperthyroidism are initially present; signs of hypothyroidism can subsequently develop.
- Painless thyroiditis: Clinical features are similar to subacute thyroiditis except for the absence of tenderness of the thyroid gland.
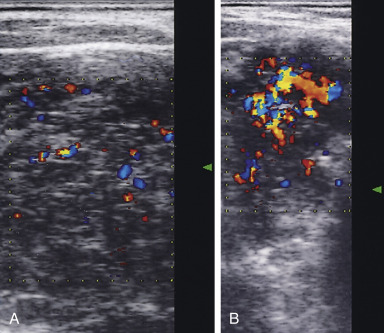
- Suppurative: Patient is febrile with severe neck pain, focal tenderness of the involved portion of the thyroid, erythema of the overlying skin.
- Riedel: Slowly enlarging hard mass in the anterior neck; often mistaken for thyroid cancer; signs of hypothyroidism occur in advanced stages.
- Hashimoto: Autoimmune disorder that begins with the activation of CD4 T-helper lymphocytes specific for thyroid antigens. The etiologic factor for the activation of these cells is unknown
- Painful subacute: Possibly postviral; usually follows a respiratory illness not considered to be a form of autoimmune thyroiditis
- Painless thyroiditis: Frequently occurs postpartum
- Infectious (suppurative): Infectious etiology, generally bacterial, although fungi and parasites have also been implicated; often occurs in immunocompromised hosts or after a penetrating neck injury
- Riedel: Fibrous infiltration of the thyroid; etiology unknown
- Drug induced: Typically painless due to lithium, interferon-alfa, amiodarone, interleukin-2
- Radiation thyroiditis: Occurs 5 to 10 days after treatment with radioactive iodine; it is painful and may result in transient exacerbation of hyperthyroidism