AUTHORS: Erin Bishop, MD and Sarah Hall, MD
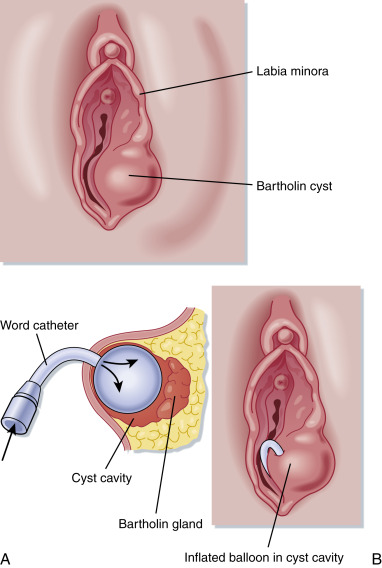
The Bartholin glands are located in the labia minora at 4 o’clock and 8 o’clock, lateral to the bulbocavernosus muscle. The glands are connected to ducts that lie between the labia minora and the hymenal edge. They are nonpalpable, approximately 0.5 cm in diameter, and are used for lubrication and moisturizing the vaginal vestibular mucosa.
| ||||||||||||||||||||
2% to 3% of reproductive age women may experience swelling of the Bartholin gland in their lifetime.
- The majority of Bartholin gland cysts and abscesses are found in women of reproductive age; involution often occurs by 30 yr of age.
- Any patient presenting after age 40 or with a history of vulvar cancer should be evaluated by a gynecologist, and biopsy is recommended to investigate for potential vulvar carcinoma of the Bartholin gland. The incidence of carcinoma is highest among women in their 60s.
- Patients with Bartholin gland cysts may have a painless, unilateral, medial-protruding vulvar swelling mass without signs of surrounding cellulitis (Fig. E1).
- Patients with infected cyst or abscess may present after having a painless cyst, but then new onset of symptoms will occur, including but not limited to:
- Painful, acute swelling of unilateral labia; tender, fluctuant labial mass (Fig. E2); erythema; edema; dyspareunia; lymphangitis; pain while sitting or walking; or sudden discharge from abscess resulting in relief of pain.
- Fever is rare but may be present in individuals who are immunocompromised.
- The provider will be able to visualize unilateral swelling of labia and palpate a fluctuant mass at the inferior labia majora or lower vestibule. Purulent discharge may be noted if the abscess is rupturing. Patients may present complaining of drainage of an abscess that has already ruptured, but if completely drained, there may be no observation of a mass.
- Patients with vulvar carcinoma may also present with swelling of the Bartholin gland in up to 5% of cases.
- Presenting symptoms of malignant lesions of the Bartholin gland include painless mass, bleeding, and pruritus, but rarely pain.
- Missed diagnosis of malignancy may result in poorer outcome for those patients due to the extensive vascular and lymphatic vessels present in the vulva.
- Drainage of cyst and biopsy of cyst wall site are generally adequate for excluding malignancy.
- Cyst formation in the glands commonly results from mucus buildup in gland ducts.
- For abscesses, the most common pathogens are Escherichia coli and Staphylococcus aureus. Less common causative pathogens include Streptococcus pneumoniae and Haemophilus influenzae. The cause of a Bartholin abscess is rarely a sexually transmitted infection such as gonorrhea or chlamydia.