AUTHORS: Luca Katz, BA and Manuel F. DaSilva, MD
Polymyalgia rheumatica (PMR) is an inflammatory condition characterized by muscle pain and stiffness of the neck, shoulder, and pelvic girdle. PMR primarily affects the elderly and can occur alone or in conjunction with giant cell arteritis (GCA).1
Anarthritic rheumatoid syndrome
| ||||||||||||
- PMR almost exclusively occurs above age 50 with peak incidence between ages 70 and 79 with a female:male ratio 2:1.1
- In the U.S., incidence is 52.5 cases per 100,000, increasing with advancing age, with a prevalence of 0.5% to 0.7%. A recent literature review showed the global epidemiology of PMR is more limited with a greater variation in prevalence and estimates. Of note, GCA is higher in populations of Northern European ancestry.1
- Patients with PMR often have symptoms for 1 to 3 mo before a diagnosis is made.
- Onset of symmetric muscle pain and stiffness, which is worse in the morning (similar to other inflammatory disorders) and recurs with periods of inactivity.2
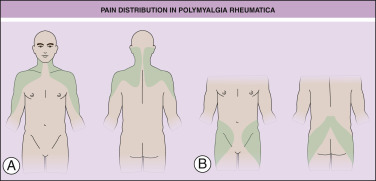
- Neck, shoulders, lower back, hips, thighs, and occasionally trunk and arms are involved. Shoulders are usually affected first. Pain distribution in PMR is illustrated in Fig. E1.
Figure E1 Typical distribution of pain in patients with polymyalgia rheumatica (PMR).
Shaded areas demonstrate typical sites of pain in individuals with PMR, including (A) shoulder girdle and neck pain distribution and (B) pelvic girdle pain distribution.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
- Constitutional symptoms of fatigue, malaise, weight loss, loss of appetite, and low-grade fever may accompany pain and stiffness.
- Physical exam may reveal limited range of motion of shoulder (most common), cervical spine, and hips. May have subdeltoid and subacromial bursitis and peripheral joint synovitis. Motor exam is normal, although can be limited by pain.
- High-spiking fevers, night sweats, visual disturbances, headaches, or jaw claudication should raise suspicion of giant cell arteritis and be further evaluated promptly.3
The cause is unknown, but both PMR and GCA are associated with HLA-DRB1 haplotype. With both conditions, also see elevated Th17 cells and decreased regulatory T-cells.2