AUTHORS: Benjamin E. Hook, MD and Marcin Byra, DO



DefinitionHypoglycemia refers to abnormally low blood glucose levels in circulating plasma. It is defined as a glucose value <70 mg/dl (3.9 mmol/L). “Serious hypoglycemia” refers to values <54 mg/dl (3.0 mmol/L). “Severe hypoglycemia” is any glucose value necessitating external assistance to correct it. “Reactive hypoglycemia” refers to symptoms of hypoglycemia with plasma glucose value >70 mg/dl. A multitude of scenarios can lead to this potentially fatal condition.1
SynonymsGlycopenia
Low blood glucose
Low blood sugar
HG
| ICD-10CM CODES | | E10.641 | Type 1 diabetes mellitus with hypoglycemia with coma | | E10.649 | Type 1 diabetes mellitus with hypoglycemia without coma | | E11.641 | Type 2 diabetes mellitus with hypoglycemia with coma | | E11.649 | Type 2 diabetes mellitus with hypoglycemia without coma | | E13.641 | Other specified diabetes mellitus with hypoglycemia with coma | | E13.649 | Other specified diabetes mellitus with hypoglycemia without coma | | E16.1 | Other hypoglycemia | | E16.2 | Hypoglycemia, unspecified |
|
Epidemiology & Demographics
- Most commonly seen in patients with diabetes mellitus (DM)1,2
- More common in type 1 DM. Estimated that glucose levels may be as low as 50 to 60 mg/dl ∼10% of the time in type 1 DM.1,3
- Although less prevalent than type 1, absolute cases of hypoglycemia is higher in patients with type 2 DM because of the significantly larger population of people with type 2 DM. Rates of severe hypoglycemic episodes in type 1 DM range from 115 to 320 episodes/100 patient years, whereas rates for type 2 DM range from 35 to 70 episodes/100 patient years.2,3
- Elderly adults with DM are at higher risk of hypoglycemia because of alterations in adaptive physiologic responses to low glucose levels. In addition, this patient population has comorbidities, including cognitive and functional decline, that interfere with rapid identification and response to hypoglycemic episodes. Elderly patients are more likely to be hospitalized for insulin-related hypoglycemia than younger cohorts.2
Physical Findings & Clinical Presentation1
- Symptoms are often nonspecific.
- Early symptoms include sweating, pallor, anxiety, palpitations, hunger, and tremor.
- Late symptoms with lower plasma glucose levels include seizures, altered mental status, and coma.
- Profound or prolonged hypoglycemic episodes can cause irreversible brain injury, cardiopulmonary arrest, and death.
- Older adults may present with atypical symptoms: Nausea, unsteadiness, falls, or transient ischemia that can delay diagnosis.2
Etiology (Box 1
- Systemic glucose balance and effects of circulating hormones on endogenous production and use of glucose are described in Table 1. Physiologic responses to decreasing plasma glucose concentrations are summarized in Table 2.
- Medications are the most common cause of hypoglycemia.1,2
- Most common causes include hyperinsulinemia due to therapeutic treatment with exogenous insulin and/or insulin secretagogues (sulfonylureas [SU] and meglitinides [MG]). Can also be exacerbated by medication use without proper exogenous glucose intake or increased insulin sensitivity due to weight loss.2
- Alcohol use leading to lack of endogenous glucose production1,2
- Critical illness
- Organ failure (hepatic, cardiac, or renal)
- Sepsis (urinary tract infection and pneumonia common sources in elderly population)
- Hormone deficiency (cortisol, glucagon, and epinephrine)
- Endogenous hyperinsulinism (insulinoma, functional β-cell disorders, insulin autoimmune hypoglycemia)
- Rare fatal episodes thought to be secondary to ventricular arrhythmias
TABLE 1 Systemic Glucose Balancea and Effects of Circulating Hormones on Endogenous Production and Use of Glucose
| Source of Glucose Influx or Efflux | Hormonal Effects |
|---|
| Insulin | Glucagon | Epinephrine |
|---|
| Glucose Influx into the Circulation |
| Exogenous glucose delivery | | | |
| Endogenous glucose delivery | | | |
| In liver: Glycogenolysis and gluconeogenesis | ↓ | ↑ | ↑ |
| In kidneys: Gluconeogenesis | ↓ | | ↑ |
| Glucose Efflux Out of the Circulation |
| Ongoing brain glucose utilization | | | |
| Variable glucose utilization by other tissues (e.g., muscle fat, liver, kidneys) | ↑ | | ↓ |
From Melmed S et al: Williams textbook of endocrinology, ed 14, Philadelphia, 2019, Elsevier.
TABLE 2 Physiologic Responses to Decreasing Plasma Glucose Concentrations
| Response | Glycemic Thresholda (mmol/L [mg/dl]) | Physiologic Effects | Role in Prevention or Correction of Hypoglycemia (Glucose Counterregulation) |
|---|
| ↓Insulin | 4.4-4.7 (80-85) | ↑Ra (↓ Rd) | Primary glucose regulatory factor, first defense against hypoglycemia |
| ↑Glucagon | 3.6-3.9 (65-70) | ↑Ra | Primary glucose counterregulatory factor, second defense against hypoglycemia |
| ↑Epinephrine | 3.6-3.9 (65-70) | ↑Ra, ↓ Rc | Involved, critical when glucagon is deficient, third defense against hypoglycemia |
| ↑Cortisol and growth hormone | 3.6-3.9 (65-70) | ↑Ra, ↓ Rc | Involved, not critical |
| Symptoms | 2.8-3.1 (50-55) | ↑Exogenous glucose | Prompt behavioral defense (food ingestion) |
| ↓Cognition | <2.8 (50) | - | (Compromises behavioral defense) |
| ↓Brain glucose metabolism | <2.8 (50) | - | - |
Ra, Rate of glucose appearance, glucose production by the liver and kidneys; Rc, rate of glucose clearance by insulin-sensitive tissues; Rd, rate of glucose disappearance, glucose utilization by insulin-sensitive tissues such as skeletal muscle (no direct effect on central nervous system glucose utilization).
From Melmed S et al: Williams textbook of endocrinology, ed 14, Philadelphia, 2019, Elsevier.
BOX 1 Causes of Hypoglycemia
Postprandial Hypoglycemia (Reactive)
- Postoperative rapid gastric emptying (alimentary hyperinsulinism)
- Fructose intolerance
- Galactosemia
- Leucine intolerance
- Idiopathic
Fasting Hypoglycemia
- Overuse of glucose
- Elevated insulin levels
- Exogenous insulin (therapeutic, factitious)
- Oral hypoglycemic (therapeutic, factitious)
- Islet cell disorders (adenoma, nesidioblastosis, cancer)
- Excessive islet cell function (prediabetes, obesity)
- Antibodies to endogenous insulin
- Normal to low insulin levels
- Ketotic hypoglycemia
- Hypermetabolic state (sepsis)
- Rare extrapancreatic tumors
- Carnitine deficiency
Underproduction of Glucose
- Hormone deficiencies (growth hormone, glucagon, hypoadrenalism)
- Enzyme disorders
- Glycogen metabolism (glycogen phosphorylase, glycogen synthetase)
- Hexose metabolism (glucose-6-phosphatase, fructose-1,6-biphosphatase)
- Glycolysis, Krebs cycle (phosphoenolpyruvate carboxykinase, pyruvate carboxylase, malate dehydrogenase)
- Alcohol and probably other drugs
- Liver disease (cirrhosis, fulminant hepatic failure)
- Severe malnutrition
|
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia, 2022, Elsevier.
 Diagnosis1
Diagnosis1Characterized by Whipple triad:
- Symptoms potentially explained by hypoglycemia
- Low blood glucose levels during the symptoms
- Relief of symptoms with administration of glucose or glucagon

- Hypoglycemia can cause severe morbidity and death if not dealt with promptly and effectively.
- Hypoglycemia is very common in patients with DM, especially type 1 DM, and most commonly it is a side effect of medications.
- Elderly patients with DM are at higher risk for serious hypoglycemic episodes and can initially present with atypical symptoms.
- In patients who are hospitalized, the etiology is often multifactorial.
- Clinically important hypoglycemia is uncommon in nondiabetic patients, and evaluation for a hypoglycemic disorder in these patients should only occur if the Whipple triad is met.
- Pediatric hypoglycemia: A classification of hypoglycemia in infants and children is summarized in Table E3.
TABLE E3 Classification of Hypoglycemia in Infants and Children
| NEONATAL TRANSITIONAL (ADAPTIVE) HYPOGLYCEMIA |
Associated With Inadequate Substrate or Immature Enzyme
Function in Otherwise Normal Neonates
Prematurity
Small for gestational age
Normal newborn
Transient Neonatal Hyperinsulinism
Infant of diabetic mother
Small for gestational age
Discordant twin
Birth asphyxia
Infant of toxemic mother |
| NEONATAL, INFANTILE, OR CHILDHOOD PERSISTENT HYPOGLYCEMIA |
Hyperinsulinism
Recessive KATP channel HI
Recessive HADH (hydroxyl acyl-CoA dehydrogenase) mutation HI
Recessive UCP2 (mitochondrial uncoupling protein 2) mutation Hl
Focal KATP channel HI
Dominant KATP channel HI
Atypical congenital hyperinsulinemia (no mutations in ABCC8 or KCN11 genes)
Dominant glucokinase HI
Dominant glutamate dehydrogenase HI (hyperinsulinism-hyperammonemia syndrome)
Dominant mutations in HNF-4A and HNF-1A (hepatocyte nuclear factors 4α and 1α) HI with monogenic diabetes of youth later in life
Dominant mutation in SLC16A1 (the pyruvate transporter)-exercise-induced hypoglycemia
Activating mutations in the calcium channel CACNA1D (permit calcium influx and thus unregulated insulin secretion)
Acquired or familial islet adenoma associated with mutations in MEN1 gene
Beckwith-Wiedemann syndrome
Kabuki syndrome
Insulin administration (Munchausen syndrome by proxy)
Oral sulfonylurea drugs
Congenital disorders of glycosylation
Counter-Regulatory Hormone Deficiency
Panhypopituitarism
Isolated growth hormone deficiency
Adrenocorticotropic hormone deficiency
Addison disease (including congenital adrenal hypoplasia, adrenal leukodystrophy, triple A syndrome, ACTH receptor deficiency, and autoimmune disease complex)
Epinephrine deficiency
Glycogenolysis and Gluconeogenesis Disorders
Glucose-6-phosphatase deficiency (GSD la)
Glucose-6-phosphate translocase deficiency (GSD lb)
Amylo-1,6-glucosidase (debranching enzyme) deficiency (GSD III)
Liver phosphorylase deficiency (GSD VI)
Phosphorylase kinase deficiency (GSD IX)
Glycogen synthetase deficiency (GSD 0)
Fructose-1,6-diphosphatase deficiency
Pyruvate carboxylase deficiency
Galactosemia
Hereditary fructose intolerance
Lipolysis Disorders
Fatty Acid Oxidation Disorders
Carnitine transporter deficiency (primary carnitine deficiency)
Carnitine palmitoyltransferase-1 deficiency
Carnitine translocase deficiency
Carnitine palmitoyltransferase-2 deficiency
Secondary carnitine deficiencies
Very-long-, long-, medium-, short-chain acyl-CoA dehydrogenase deficiency |
| OTHER ETIOLOGIES |
Substrate-Limited Causes
Ketotic hypoglycemia
Poisoning-drugs
Salicylates
Alcohol
Oral hypoglycemic agents
Insulin
Propranolol
Pentamidine
Quinine
Disopyramide
Ackee fruit (unripe)-hypoglycin
Litchi-associated toxin (toxin hypoglycemic syndrome)
Vacor (rat poison)
Trimethoprim-sulfamethoxazole (with renal failure) L-Asparaginase and other antileukemic drugs
Liver Disease
Reye syndrome
Hepatitis
Cirrhosis
Hepatoma |
| AMINO ACID AND ORGANIC ACID DISORDERS |
Maple syrup urine disease
Propionic academia
Methylmalonic academia
Tyrosinosis
Glutaric aciduria
3-hydroxy-3-methylglutaric aciduria |
| SYSTEMIC DISORDERS |
Sepsis
Carcinoma/sarcoma (secreting-insulin-like growth factor II)
Heart failure
Malnutrition
Malabsorption
Antiinsulin receptor antibodies
Antiinsulin antibodies
Neonatal hyperviscosity
Renal failure
Diarrhea
Burns
Shock
Chiari malformation
Postsurgical complication
Pseudohypoglycemia (leukocytosis, polycythemia)
Excessive insulin therapy of insulin-dependent diabetes mellitus
Factitious disorder
Nissen fundoplication (dumping syndrome)
Falciparum malaria |
GSD, Glycogen storage disease; HI, hyperinsulinemia; KATP, regulated potassium channel.
From Kliegman RM, St Geme J, eds: Nelson textbook of pediatrics, ed 21, Philadelphia, 2020, Elsevier.
Differential DiagnosisHypoglycemic symptoms in the presence of normal plasma glucose levels (>70 mg/dl) point to other etiologies: Postprandial syndrome, stroke, sepsis, seizure/postictal state, cardiac disease, psychiatric disease, metabolic disorders (hyperthyroidism, pheochromocytoma), drug intoxication.1
Workup- If Whipple triad is positive, the next step is to consider a patient’s medical status.1
- Iatrogenic factors are the most common causes of hypoglycemia in hospitalized patients (review the NPO status, timing of feeding, glucose-lowering medications, and interactions between medications).1
- Detailed history, including past medical history, a thorough medication history, and timing of hypoglycemia (in regard to meals and medications).
- Special attention should be given to chronic diseases that can precipitate hypoglycemia such as chronic renal disease with a glomerular filtration rate <60.2
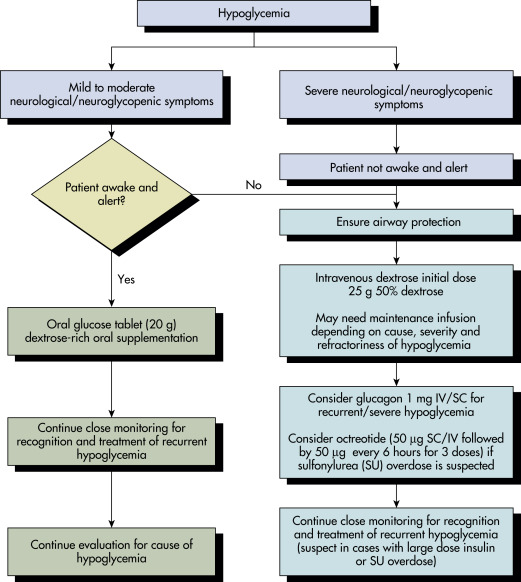
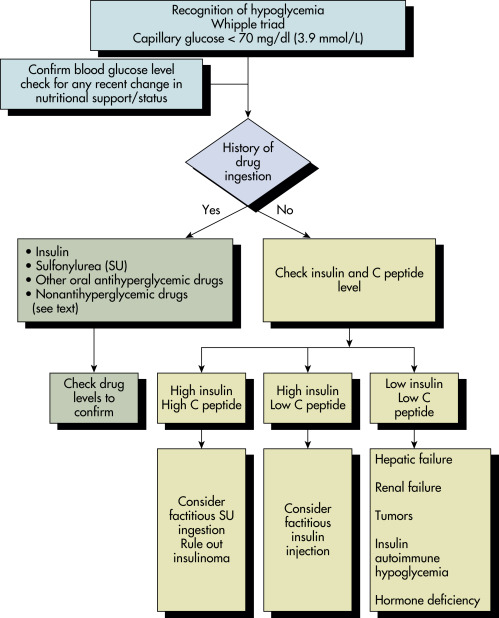
Laboratory Tests- An algorithm for recognition and evaluation of hypoglycemia is described in Fig. E1.
- If the cause is not apparent after a thorough history, the following is appropriate:
Figure E1 Recognition and evaluation of hypoglycemia.
From Vincent JL et al: Textbook of critical care, ed 7, Philadelphia, 2017, Elsevier.
FastingIf symptoms witnessed when fasting, with verified low blood glucose levels, consider the following laboratory tests: Plasma glucose, β-hydroxybutyrate (BHOB), insulin, C-peptide, proinsulin, screen for SU and MG metabolites.1
Postprandial- Plasma glucose, insulin, C-peptide, and proinsulin before ingestion of the meal and every 30 min thereafter for 5 h.1
- Only evaluate the samples drawn when glucose levels are <60 mg/dl.
- If a patient has a presentation consistent with Whipple triad, then measure SU, MG, and antibodies to insulin.1
72-H Fast1- Collect blood specimens for measurement of plasma glucose, insulin, C-peptide, proinsulin, and BHOB every 6 h until the glucose concentration is <60 mg/dl.
- Increase frequency of sampling to every 1 to 2 h.
- Insulin, C-peptide, and proinsulin are only relevant in those specimens in which the plasma glucose concentration is <60 mg/dl.
- The fast should be ended when any of the following occurs:
- The plasma glucose concentration is <45 mg/dl.
- The patient has symptoms or signs of hypoglycemia.
- 72 h has elapsed.
- The plasma glucose concentration is <55, and Whipple triad has been documented on a prior occasion.
- Insulin antibodies are also measured but do not need to be measured during the hypoglycemic state.
Imaging Studies1If hypoglycemia is suspected secondary to an insulinoma or malignancy, transabdominal ultrasound (US), computed tomography scan, or endoscopic US can be used to help with diagnosis as well as for staging purposes.