AUTHORS: Ozair K. Meghani, BA and Manuel F. DaSilva, MD


DefinitionSpondyloarthropathies (SpAs) are a group of diverse interrelated systemic autoinflammatory conditions that are serologically negative for rheumatoid factor, connected by an underlying genetic risk (HLA-B27) with similar patterns of inflammation. This group encompasses ankylosing spondylitis, psoriatic arthritis, reactive arthritis, enteropathic arthritis, undifferentiated spondyloarthritis, and juvenile-onset spondyloarthritis (Table 1). SpAs are broadly classified by axial vs. peripheral joint involvement, and with or without radiographic progression.
TABLE 1 Comparison of Ankylosing Spondylitis and Related Disorders
| Feature | Ankylosing Spondylitis | Psoriatic Arthritis | Reactive Arthritis | Enteropathic Arthropathy |
|---|
| Sex (male:female) | 2-3:1 | 1:1 | 1:1 | 1:1 |
| Age of onset | <40 yr | 35-55 yr | 20-40 yr | Any age |
| Sacroiliitis or spondylitis (%) | 100 | ∼20 | ∼40 | <20 |
| Symmetry of sacroiliitis | Symmetrical | Asymmetrical | Asymmetrical | Symmetrical |
| Peripheral arthritis (%) | ∼25 | 95 | 90 | 5-20 |
| Distribution | Axial and lower limbs | Variable | Lower limbs | Variable |
| HLA-B27 positivity (%) | 85-95 | 25-60∗ | 30-70 | 7-70† |
| Uveitis | 0-40 | ∼20 | ∼50 | <15 |
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
SynonymsSpondyloarthritides
Spondylopathy
Spondylitis
| ICD-10CM CODES | | M46.80 | Other specified inflammatory spondylopathies, unspecified site | | M46.82 | Other specified inflammatory spondylopathies, cervical region | | M46.83 | Other specified inflammatory spondylopathies, cervicothoracic region | | M46.86 | Other specified inflammatory spondylopathies, lumbar region | | M46.87 | Other specified inflammatory spondylopathies, lumbosacral region | | M46.89 | Other specified inflammatory spondylopathies, multiple sites | | M46.81 | Other specified inflammatory spondylopathies, occipito-atlanto-axial region | | M46.88 | Other specified inflammatory spondylopathies, sacrococcygeal region | | M46.84 | Other specified inflammatory spondylopathies, thoracic region | | M46.85 | Other specified inflammatory spondylopathies, thoracolumbar region |
|
Epidemiology & DemographicsPrevalenceWorldwide prevalence of SpA is 0.2% to 1.6%, with approximately 1% of the U.S. population affected. Varies regionally with prevalence of HLA-B27. The most prevalent subtype is ankylosing spondylitis followed by psoriatic arthritis.
Predominant Sex & AgeMales younger than age 45 yr are predominantly affected. Previously, the male:female ratio was thought to be 10:1; more recently, approximately 3:1.
Patients >45 yr may present with chronic, severe disease due to diagnostic delays.
Risk FactorsHLA-B27 allele,∗ male sex,∗ smoking,∗ ethnic background, family history of SpA, and certain infections. (∗Associated with more severe disease.)
GeneticsAssociation with the HLA-B27 allele is the strongest known genetic risk factor; approximately 95% of patients with ankylosing spondylitis have the HLA-B27 allele.
Physical Findings & Clinical Presentation
- History:
- Inflammatory low back pain may be the primary presenting symptom:
- Pain and stiffness in the low back or buttocks that is worse in the morning, may awaken the patient from sleep, and improves with exercise
- Morning stiffness generally lasting longer than 1 h
- Improvement with NSAIDs
- Sensitivity up to 90% and positive likelihood ratio up to 2.2 for axial SpA
- Symptoms of systemic and peripheral inflammation are additional clues that can be elicited in a comprehensive review of systems:
- Uveitis: Painful ocular inflammation
- Psoriasis: Chronic skin inflammation with red patches and silvery scales
- Inflammatory bowel disease: Crohn disease and ulcerative colitis
- Synovitis: Inflammation of the synovial membrane of joints
- Enthesitis: Inflammation at the site of tendon or ligament insertion onto bone
- Dactylitis: Tenosynovitis of the digits causing classic sausage-like appearance
- Physical exam:
- Axial joints: Spine and sacroiliac (SI) joints.
- Inspect curvature, palpate for tenderness, and evaluate range of motion for cervical, thoracic, and lumbar spine. Measure degree of axial involvement with occiput wall, thoracic expansion. Patients with SpA may have an abnormal Schober test result (Fig. E1). This test is performed by having the patient stand erect and marking the distance between the midpoint of the posterior superior iliac spines (“dimples of Venus”) and 10 cm above that point. The patient is then asked to maximally flex forward while the more caudal spot is kept stationary. The more cephalad point on the tape measure should demonstrate at least 5 cm of excursion. This abnormality also can be seen with lumbar degenerative disk disease. Test for sacroiliitis with Patrick and Gaenslen tests.
- Peripheral joints: Lower extremity predominance.
- Inspect for signs of inflammation, including dactylitis, synovitis, and enthesitis.
- Evaluate for systemic involvement manifesting as anterior uveitis and psoriasis:
- Slit lamp is necessary to diagnose anterior uveitis.
- Full skin exam is critical to detect occult psoriasis; look for nail changes.
- Musculoskeletal manifestations commonly affect weight-bearing joints with high mechanical stress; thus it is particularly important to examine the lumbar spine, SI joints, and lower extremities.
- Degree of axial involvement can be measured via specialized exam techniques, which are used to track disease activity and response to treatment over time.
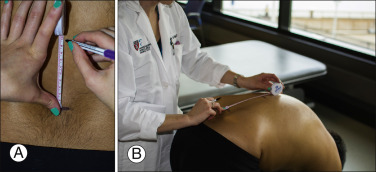
Figure E1 Schober test.
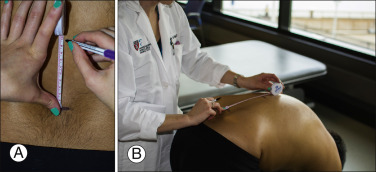
A, With the patient standing, measure 10 cm superior from the midpoint of the posterior superior iliac spine. B, Then, ask the patient to maximally flex forward while the more caudal spot is kept stationary. The total length between the lines should be greater than 15 cm.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
EtiologyThe exact etiology of SpAs is still unknown; however, evidence indicates a combination of genetics and environmental factors play an important role in susceptibility and pathogenesis.
- Genetic:
- The HLA-B27 allele has a strong association with SpA, through mechanisms that are not fully understood. The subset of HLA-B27 patients with SpAs are at an increased risk for axial skeleton involvement and earlier age of onset.
- Environmental:
- Microbial infections, disruptions in barrier defense mechanisms (skin and intestinal mucosa), and mechanical articular stressors may trigger an inflammatory response, which then develops into signs and symptoms specific to each type of SpA.
- Autoinflammatory:
- Key components of the inflammatory cascade involved in the pathogenesis of SpA are tumor necrosis factor (TNF), interleukin (IL)-12, IL-17, IL-23, and prostaglandins. Success in treatment with targeted therapies to each of these molecules has helped us understand their role in the etiology of SpA.

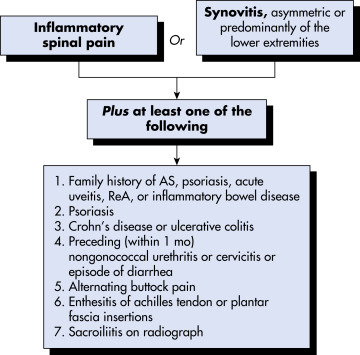
Several classification criteria now exist for the SpAs. In 1991, the European Spondyloarthropathy Study Group (ESSG) criteria were developed to establish criteria for the SpAs (Fig. 2). These criteria have been demonstrated to be 87% sensitive and specific for the diagnosis of SpA. They are somewhat less well suited for diagnosis of early disease but extremely useful for established disease.
Figure 2 European Spondyloarthropathy Study Group (ESSG) criteria for spondyloarthritis.

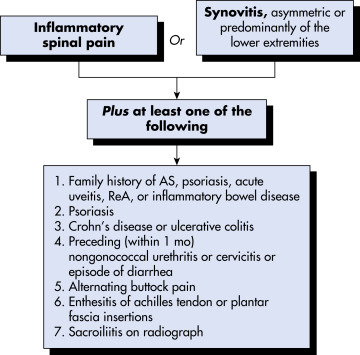
AS, Ankylosing spondylitis/axial spondyloarthritis; ReA, reactive arthritis.
From https://omicsgroup.org. Accessed September 29, 2014. In Firestein GS et al: Firestein & Kelley’s Textbook of Rheumatology, ed 11, Philadelphia, 2021, Elsevier.
Table 2 summarizes current diagnostic criteria for SpA.
TABLE 2 Criteria for Spondyloarthritis (SpA)∗
| Amor Criteria | ESSG Criteria |
|---|
| Past or current clinical manifestations: | Inflammatory back pain or synovitis: |
- Back pain at night and/or back stiffness in the morning (1 point)
| - Asymmetric synovitis or
- Predominantly lower limb synovitis
|
- Asymmetric oligoarthritis (2 points)
| AND |
- Gluteal pain without other details (1 point) or alternating gluteal pain (2 points)
| One or more of the following:
- Positive family history
- Psoriasis
|
- Sausage-like digit or toe (2 points)
| - Inflammatory bowel disease
|
- Heel pain or other enthesopathy (2 points)
| - Urethritis, cervicitis, or acute diarrhea within 1 mo before arthritis
|
- Iritis (2 points)
- Nongonococcal urethritis within 1 mo before the onset of arthritis (1 point)
| - Buttock pain alternating between right and left gluteal areas
- Enthesopathy
- Sacroiliitis (radiography)
|
- Acute diarrhea within 1 mo before the onset of arthritis (1 point)
| |
- Past or current psoriasis and/or balanitis and/or inflammatory bowel disease (2 points)
| |
| Radiographic changes: |
- Sacroiliitis grade 2 or more if bilateral, grade 3 or more if unilateral (3 points)
| |
| Predisposing genetic factors: |
- Presence of HLA-B27 antigen and/or family history of ankylosing spondylitis, Reiter syndrome, psoriasis, uveitis, or chronic bowel disease (2 points)
| |
| Responsiveness to treatment: |
- Improvement within 48 hr after initiation of an NSAID and/or recurrence within 48 hr after discontinuation of an NSAID (2 points)
| |
ESSG, European Spondyloarthropathy Study Group; NSAID, nonsteroidal antiinflammatory drug.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
Differential Diagnosis
- Seronegative rheumatoid arthritis (peripheral presentation)
- Degenerative disc disease (axial presentation) or DISH
- Inflammatory osteoarthritis (axial or peripheral presentation)
- Hypertrophic osteoarthropathy (peripheral presentation)
Workup
- Young patients, particularly men <45 yr, with chronic inflammatory low back pain responsive to NSAIDs should be screened.
- Patients with psoriasis, inflammatory bowel disease, or recent gastrointestinal or genitourinary infections presenting with new-onset low back or peripheral joint pain should also be screened.
- Screening begins with a comprehensive history and physical exam.
- HLA-B27 testing and imaging of SI joints and/or lumbar spine are indicated based on clinical suspicion.
Laboratory Tests
- HLA-B27:
- Negative test does not rule out SpA.
- Sensitivity: 95% for ankylosing spondylitis, 80% for reactive arthritis, 70% for psoriatic arthritis, and 50% for enteropathic arthritis.
- Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), anemia of chronic disease, leukocytosis, and thrombocytosis may reflect active inflammation. A normal CRP or ESR does not rule out spondyloarthropathies.
- Testing for rheumatoid arthritis antibodies is generally negative (rheumatoid factor, cyclic citrullinated peptide).
- Synovial fluid is inflammatory and nonspecific, with white blood cell>2,000/mm2.
Imaging Studies
- X-Ray: SI joints and lumbar spine:
- May not detect early inflammation
- 20% to 80% have nonradiographic disease at time of presentation
- May show signs of structural damage such as erosions, syndesmophytes, sclerosis, and ankylosis in chronic axial disease
- MRI: SI joints and lumbar spine:
- Subchondral bone marrow edema in early disease
- Useful when x-ray and clinical findings are nondiagnostic but clinician’s suspicion for axial SpA remains high

Improvement in symptoms, preservation of function, and prevention of structural damage can be achieved through a multidisciplinary approach.
Nonpharmacologic Therapy
- Physical and occupational therapies improve functional outcomes.
- Surgery:
- Joint replacements (high-impact joints such as hips)
- Spinal wedge osteotomy (advanced axial disease)
- Colectomy (advanced enteropathic arthritis)
Acute General Rx
- NSAIDs are first line.
- Avoid steroids in psoriatic arthritis due to risk of life-threatening pustular psoriasis and erythroderma.
Chronic Rx
- NSAIDs:
- Up to 35% of patients may achieve remission.
- Best response in early disease.
- Continuous dosing may prevent radiographic progression of axial disease.
- Disease-modifying antirheumatic drugs (DMARDs): Effective for peripheral involvement only, not effective in axial disease
- Methotrexate, leflunomide, sulfasalazine
- TNF inhibitors: NSAID or DMARD failure
- Infliximab, adalimumab, golimumab, etanercept, certolizumab pegol
- IL-17 and IL-12/23 inhibitors: 2nd TNF inhibitor failure
- Recent studies show similar efficacy compared to TNF inhibitors.
- Ixekizumab (IL-17 inhibitor) recently approved for ankylosing spondylitis.
- Ustekinumab (IL-12/23 inhibitor) and secukinumab (IL-17 inhibitor) are effective in psoriatic arthritis. Secukinumab also is approved for ankylosing spondylitis.
- Ustekinumab is also effective in Crohn-enteropathic arthritis.
- Janus kinase inhibitors: Phase II clinical trial
Tofacitinib (JAK 1, 2, 3 inhibitor) was shown to improve clinical and imaging outcomes in axial SpA, with phase III trial data pending.
Tofacitinib is approved to treat both UC and psoriatic arthritis.
Disposition
- Function and mobility may be limited in advanced axial disease.
- Psoriatic arthritis is an independent risk factor for cardiovascular disease.
Complementary & Alternative Medicine
- Strong clinical trials are lacking.
- Small studies have shown Pilates, t’ai chi, deep tissue massage, and hydroelectric therapy can be beneficial in axial SpA.
ReferralRheumatology, dermatology, ophthalmology, gastroenterology, infectious disease