AUTHORS: Anthony Sciscione, DO, and Ella Stern, MD
Gonorrhea is a sexually transmitted bacterial infection with a predilection for columnar and transitional epithelial cells. It commonly manifests as urethritis, cervicitis, or salpingitis. Infection may be asymptomatic. It differs between males and females in course, severity, and ease of recognition.
| ||||||||||||||||||||||||||||||||||||||||
- The disease is common worldwide, affects both sexes and all ages, especially younger adults; highest incidence is in inner-city areas. Per CDC reports, approximately 1.6 million new cases were found in the U.S. in 2018, with more than half found in young people ages 15 to 24 yr. Gonorrhea is the second most-commonly reported communicable disease.
- Asymptomatic anterior urethral carriage may occur in 12% to 50% of cases in men.
- Asymptomatic in 50% to 80% of cases in women. Most common dissemination is by mucosal passage to fallopian tubes, resulting in pelvic inflammatory disease (PID) in 10% to 15% of infected women. Hematogenous spread may result in septic arthritis and skin lesions. Conjunctivitis rarely occurs but may result in blindness if not rapidly treated. Infection can occur in both men and women in oropharynx and anorectally.
- The World Health Organization (WHO) reported 78 million new cases of gonorrhea worldwide among adults in 2012.
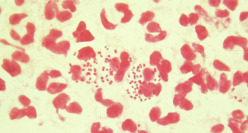
- Males: Purulent discharge from anterior urethra (Fig. E1), with dysuria appearing 2 to 7 days after infecting exposure. May have rectal infection causing pruritus, tenesmus, and discharge, or may be asymptomatic.
- Females: Initial urethritis or cervicitis may occur a few days after exposure, frequently mild. Infections may be asymptomatic or may not produce recognizable symptoms until complications have occurred. In approximately 20% of cases, uterine invasion occurs after menstrual period with signs and symptoms of endometritis, salpingitis, or pelvic peritonitis. The patient may have purulent discharge or inflamed Skene or Bartholin glands.
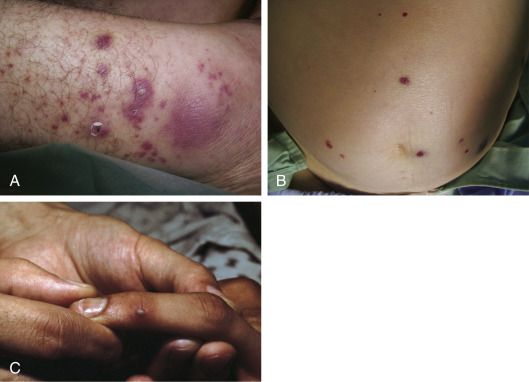
- Classic presentation of acute gonococcal PID is fever, abdominal and adnexal tenderness, and, often, absence of purulent discharge. Physical examination may be normal if asymptomatic. Disseminated gonococcal infection (DGI) may manifest with petechial or pustular acral skin lesions (Fig. E2), asymmetric polyarthralgia, tenosynovitis, or oligoarticular septic arthritis. The infection is occasionally complicated by perihepatitis and, rarely, endocarditis or meningitis.
Figure E1 Purulent urethral discharge from a man with gonococcal urethritis.
From Mandell GL et al: Principles and practice of infectious diseases, ed 6, Philadelphia, 2005, Churchill Livingstone.
Figure E2 Disseminated gonococcal infection: Skin lesions.
A, Macules, papules, and pustules over an ankle. B, Hemorrhagic papules localized in trunk. C, Hemorrhagic vessel over a distal interphalangeal joint.
Courtesy Dr. Peter Schlessinger. From Hochberg MC et al: Rheumatology, ed 5, St Louis, 2011, Mosby.
- Neisseria gonorrhoeae is also known as gonococcus. Plasmids coding for β-lactamase render some strains resistant to penicillin or tetracycline. There is an increasing frequency of chromosomally mediated resistance to penicillin, tetracycline, fluoroquinolones, and cefoxitin. In the Far East, high-level resistance to spectinomycin is endemic.
- There are a rising number of cases of quinolone-resistant N. gonorrhoeae worldwide, with the expected number to rise in the U.S. from importation.
- Men who have sex with men are vulnerable to the emerging threat of antimicrobial-resistant N. gonorrhoeae.