NANDA-I approved*
Pathophysiologic
Genetic disorder
Heritability of interrelated factors (e.g., adipose tissue distribution, energy expenditure, lipoprotein lipase activity, lipid synthesis, lipolysis
Situational (Personal, Environmental)
Abnormal eating behavior patterns*
Abnormal eating perception patterns*
Average daily physical activity is less than recommended for age and gender*
Consumption of sugar-sweetened beverages*
Disordered eating behaviors
Disordered eating perceptions
Economically disadvantaged
Energy expenditure below energy intake based on standard assessment*
Excessive alcohol consumption*
Fear regarding lack of food supply*
Formula- or mixed-fed infants
Frequent snacking*
High disinhibition and restraint eating behavior score
High frequency of restaurant or fried food*
Insufficient dietary calcium intake by children*
Maternal diabetes mellitus
Maternal smoking
Overweight in infancy
Parental obesity
Portion sizes larger than recommended*
Premature pubarche
Rapid weight gain during childhood
Rapid weight gain during infancy, including the first week, first 4 months, and first year
Sedentary behavior occurring for ≥ 2 hours/day*
Shortened sleep time*
Sleep disorder
Solid foods as major food source at < 5 months of age*
Economically disadvantaged individuals
Individuals who experienced premature pubarche
Individuals who experienced rapid weight gain during childhood
Individuals who experienced rapid weight gain during infancy
Individuals who inherit interrelated factors
Individuals who were not exclusively breastfed
Individuals who were overweight during infancy
Individuals whose mothers had gestational diabetes
Individuals whose mothers have diabetes
Individuals whose mothers smoke during childhood
Individuals whose mothers smoke during pregnancy
Individuals with high disinhibition and restraint eating behavior score
Individuals with parents who are obese
Neonates whose mothers had gestational diabetes
Inborn genetic diseases
 AUTHOR'S NOTE
AUTHOR'S NOTEGiven the public health problem of Overweight and Obesity across the life span, the addition of these nursing diagnoses to the NANDA-I Classification (2018-2020) has proven to be very clinically useful.
The interventions for these diagnoses will focus on strategies to motivate and engage individuals/families to proceed to a healthy lifestyle.
Obesity is a complex condition with sociocultural, psychological, and metabolic implications. When the focus is primarily on limiting food intake, as with many weight-loss programs and bariatric surgery, the chance of permanent weight loss is slim. To be successful, a weight-loss program for in individual needs to focus on behavior modification and lifestyle changes through exercise, decreased intake, and addressing their emotional component of overeating.
CLINICAL ALERTThe National Institutes of Health-funded Longitudinal Assessment of Bariatric Surgery-2 (LABS-2), a prospective observational study of individuals undergoing weight-loss surgery at one of 10 hospitals across the United States found in the first year following maximum weight loss, 10 percent of participants experienced diabetes progression, 26% high cholesterol, and 46% high blood pressure. A clinically important decline in physical and mental health-related quality of life was experienced by 20 and 28 percent of participants, respectively, and 12% experienced a decline in their satisfaction with their weight-loss surgery (King, Hinerman, Belle et al., 2018).
If someone is at a healthy weight, but routinely eats foods low in nutrients refer to Risk-Prone Health Behavior related to intake of insufficient nutrients and/or inactivity in the presence of a healthy weight that does not meet recommended dietary intake. For some people with dysfunctional eating, Ineffective Coping related to increased eating in response to stressors would be valid and require a referral after discharge.
The individual will commit to a weight-loss program, as evidenced by the following indicators:
- Identify the patterns of eating associated with consumption/energy expenditure imbalance.
- Can give examples of nutrient-dense foods versus those with "empty calories."
- Can identify 3 ways to increase his/her activity.
- Commit to increasing foods with high nutrient density and less with "empty calories."
- Commit to making 3 to 5 changes in food/fluid choices, which are healthier.
The child (over 8) will verbalize what is healthy eating by the following indicators:
- Can describe the "MyPlate."
- Can describe what "empty calories" mean.
- Can name "empty calories" beverages and healthier substitutions.
- Can name foods high in nutrients.
- Can name food high in sugar and "empty calories" and healthier substitutions.
The pregnant woman will verbalize healthy eating and recommended weight gain during pregnancy by the following indicators:
- Can describe vitamin, mineral, protein, fat needs during pregnancy.
- Can give examples of nutrient-dense foods versus those with "empty calories."
- Can identify 3 ways to increase his/her activity.
- Will relate the weight gain appropriate specific to her weight prior to pregnancy.
- Can explain why "dieting" is problematic.
 Level 1 Fundamental Focused Assessment (all nonacute settings)
Level 1 Fundamental Focused Assessment (all nonacute settings)
NICSelf-Efficacy Enhancement, Self-Responsibility Enhancement, Nutritional Counseling, Weight Management, Teaching: Nutrition (age appropriate), Behavioral Modification, Exercise Promotion, Coping Enhancement
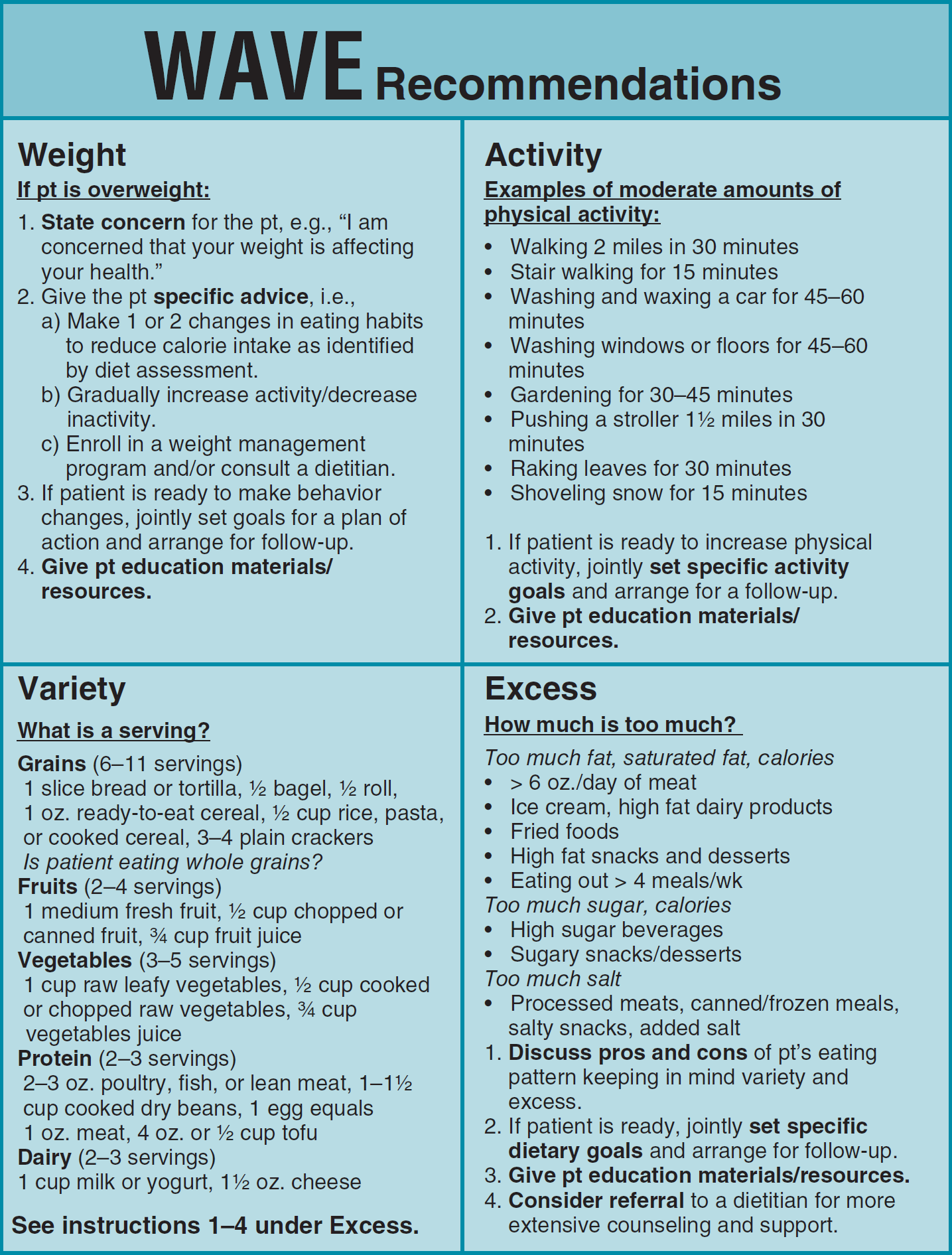
Review the WAVE Figure (Figure 2-4) and Address Weight, Activity, Variety, and Excess (WAVE) if Individual Is Interested in Learning More about Healthier Eating (*Barner et al., 2001; *Gans et al., 2003)
Data from Gans, Kim & Ross, Elizabeth & Barner, Claudia & Wylie-Rosett, Judith & McMurray, Jerome & Eaton, Charles. (2003). REAP and WAVE: New tools to rapidly assess/discuss nutrition with patients. The Journal of Nutrition. 133. 556S-62S. 10.1093/jn/133.2.556S.
Figure 2-4 Interventions
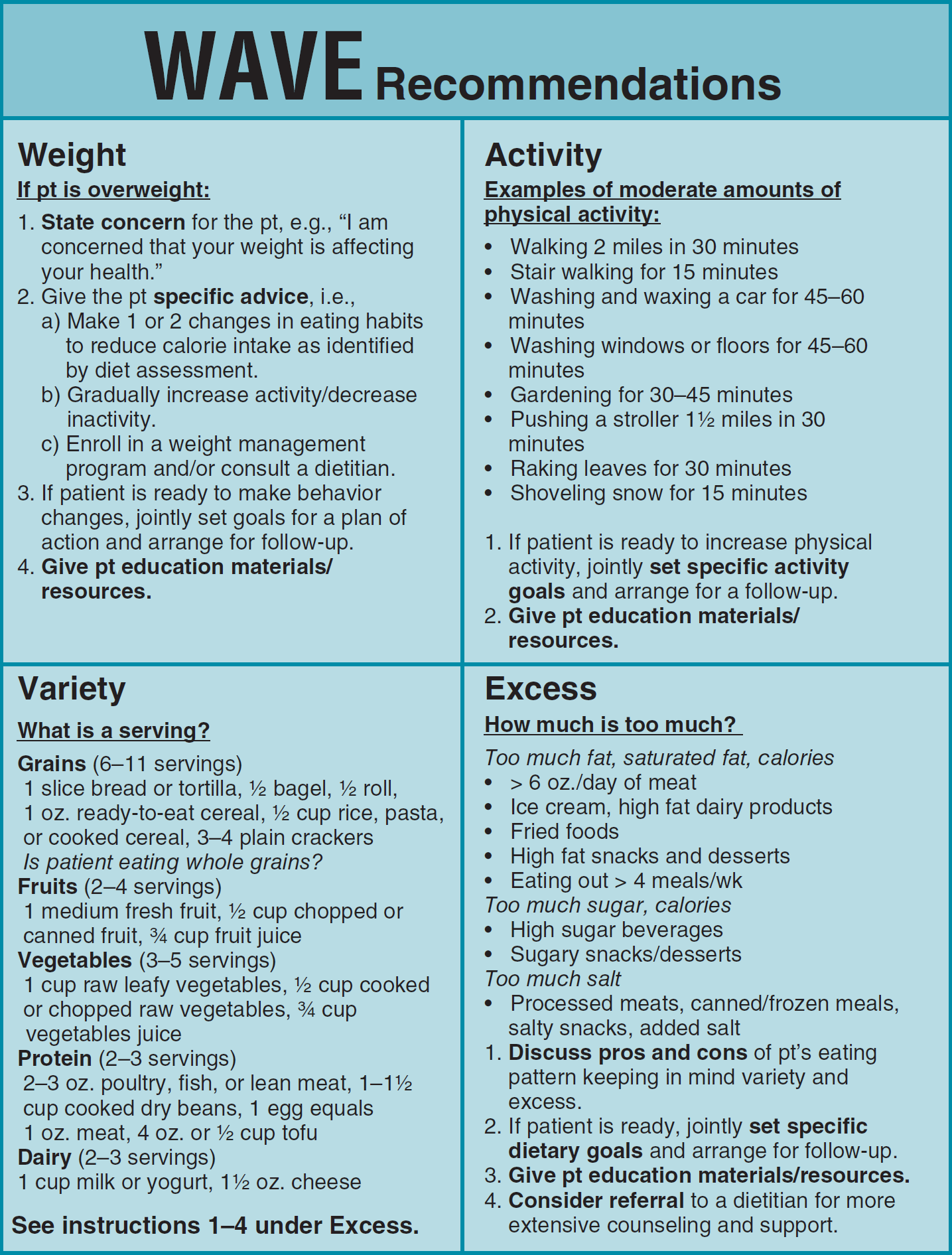
Wave is an abbreviated model for addressing nutrition in an individual and achieving healthy weight. With assessment questions and targeted interventions. It was designed to be utilized in healthcare settings as a brief intervention to activate an individual to evaluate their nutritional intake and activity level. It also can be useful with the family member responsible for food shopping and preparation, to evaluate food groups served, frequency and serving sizes eaten. For children refer to MyPlate under Imbalanced Nutrition: Less Than Body Requirements.
NOCNutritional Status: Nutrient Intake, Weight Control, Exercise Participation, Infant Nutritional Status, Weight Body Mass, Adherence Behavior: Healthy Diet, Weight Loss Behavior
NICSelf-Efficacy Enhancement, Self-Responsibility Enhancement, Nutritional Counseling, Weight Management, Teaching: Nutrition (age appropriate), Behavioral Modification, Exercise Promotion, Coping Enhancement
 Level 1 Fundamental Focused Interventions (all nonacute settings)
Level 1 Fundamental Focused Interventions (all nonacute settings)
CLINICAL ALERTBefore the first encounter to help the individual to become interested and motivated refer to Appendix C: Strategies to Promote Engagement of Individual/Support Persons for Healthier Outcomes for specific techniques to improve motivation and engagement.
 Level 1 Basic Focused Interventions (all nonacute settings)
Level 1 Basic Focused Interventions (all nonacute settings)
R:The following Level 1 Interventions are appropriate for beginning students, experienced students, and nurses to prompt the person to think of a healthier lifestyle.
Initiate Discussion: "How Can You Be Healthier?"
- Focus on the person's response (e.g., stop smoking, exercise more, eat healthier, and cut down on drinking).
- Refer to index for interventions for the targeted lifestyle change.
R:Individuals can be malnourished even though they are a healthy weight, obese, or overweight due to intake of foods high in fat and carbohydrates, and which are low in nutrients per calorie intake. The nurse should be cautioned against applying a nursing diagnosis for an overweight or obese person who does not want to participate in a weight-loss program. Instead refer to Risk-Prone Behavior.
If Appropriate, Gently and Expertly Discuss the Hazards of Obesity but Respect a Person's Right to Choose, the Right of Self-Determination
"How do you think being overweight affects you?
Focus on what the person tells you, e.g., my sugar is high, my knees hurt. Do not overload him/her with information.
 Level 2 Extended Focused Interventions (all nonacute settings)
Level 2 Extended Focused Interventions (all nonacute settings)
Before a Person Can Change, They Must (*Martin, & DiMatteo, 2010):
- Know what change is necessary (information and why).
- Desire the change (motivation).
- Have the tools to achieve and maintain the change (strategy).
- Trust the healthcare professional, who has a sympathetic presence (*Pelzang, 2010).
R:Empathic communication involving a thorough understanding of the patient's perspective improves adherence. Individuals who are informed and affectively motivated are also more likely to adhere to their treatment recommendations (*Zolnierek, & DiMatteo, 2010).
To Help to Activate Engagement in an Individual, Ask Them One of the Questions Below. Pick the Best Question That Applies to This Person. Use Language They Understand, e.g., Blood Veins or Veins That Carry Blood
- Do your legs swell during the day and go back to normal during the night?
- Explain fat tissue compresses tubes in your legs and prevents fluids from circulating well. Eventually the swelling will be permanent, 24 hours a day, causing difficulty walking and wearing shoes.
- Do you have high blood pressure, or is it getting a little higher each year?
- Explain that blood vessels are damaged when excess weight puts pressure on them and they stretch, become thinner, and lose their strength. Your heart now has to pump harder, causing high blood pressure. Over time the heart enlarges and cannot pump well. This is heart failure.
- Is your cholesterol level increasing each year?
- Explain that stretching of your blood vessels damages the inside of the blood tubes. Cholesterol sticks to the damaged tubes and slows the blood flow to your kidneys, eyes, brain, and legs. This can cause strokes, renal failure, vision problems, and blood clots in your legs.
- So you may not feel that anything is wrong, but high blood pressure can permanently damage your heart, brain, eyes, and kidneys before you feel anything. Even losing 10 pounds can reduce your blood pressure.
- Is your blood glucose test getting a little higher each year? Is there diabetes in your family?
- Explain that the more fatty tissue you have, the more resistant your cells become to insulin.
- Insulin carries sugar from blood to the cells. When you are overweight, the cells are damaged and will not absorb the insulin, so your blood sugar goes up. High blood sugars damage blood vessels in the eyes, kidneys, and heart.
- Does your back, your knees, or other joints hurt?
- Explain that extra weight puts pressure on your joints and bones. This pressure wears away the cartilage, the cushion at the ends of your bones. This causes the bone to rub against another bone causing pain.
- Do you think people who are overweight have problem healing from injuries or surgery?
- Explain that fat tissue has less blood supply, which is needed for healing. The incision has more pressure against it when you are overweight, which can cause the wound to open up. If antibiotics are needed for infection, the medicine will not work well because of poor circulation to the wound.
If the person does not identify any negative effects of excess weight that they feel, explain the effects of excess weight are insidious and often not felt by the person until the effects threaten their health or cause pain, e.g., joint pain or the onset of diabetes mellitus.
Review Usual Daily Intake to Identify Patterns that Contribute to Excess Weight
- Usual breakfast, usual lunch, usual dinner
- Snacks, nighttime eating
- Skipping meals
 CARP'S CUES
CARP'S CUES"Before you eat or drink something with "empty calories,"** ask yourself "Is this worth it?" If so, ENJOY it. There is no such thing as "bad foods," only bad amounts.
**"Empty calories" are foods/drinks that are high in calories but have little or no nutritional value, such as soda, chips, and French fries.
Promote Activation to Engage the Individual in Healthier Behavior. Focus on What the Person Wants to Change. Limit to Three Changes
R: *Activation refers to a person's ability and willingness to take on the role of managing their health and health care (*Hibbard & Cunningham, 2008).
Address What Excesses or Deficiencies Exist, Using the Information He/She Gave, for Example:
- "I ate fried chicken wings last night for dinner."
- "Anything else?" "No."
- How could you change what you ate to improve nutrients and decrease fat?
- Listen. If no response:
- Suggest 1 or 2 pieces of fried chicken instead of 12 wings. One piece of fried chicken with no batter has 158 calories/thigh or 131 calories/breast. One medium fried chicken wing with no batter has 102 calories. Ten wings have 1020 calories.
- What could you eat in addition to the fried chicken that is a vegetable (e.g., salad)?
R:Chicken wings have more fat before frying than a chicken thigh or breast. White meat has less calories than dark meat.
Avoid Describing Foods as Bad or Good. Explain Nutrient Density of Foods (*Hunter & Cason, 2006)
R:The nutrient density of foods can be high, medium, low, or none. Foods with high nutrient density are low in calories and high in nutrients.
R:Nutrient dense foods give the most nutrients for the fewest amount of calories.
- Foods that are nutrient dense (low in calories), such as:
- Fruits and vegetables that are bright or deeply colored
- Foods that are fortified
- Lower fat versions of meats,* milk, dairy products, and eggs
- Foods that are less nutrient dense (high in calories, low or no nutrients)
- Are lighter or whiter in color
- Contain a lot of refined sugar
- Contain refined products (white bread as compared to whole grains)
- Contain high amounts of fat for the amount of nutrients compared to similar products (fat-free milk vs. ice cream* *). For example:
- An apple is a better choice than a bag of pretzels with the same number of calories, but the apple provides fiber, vitamin C, and potassium.
- An orange is better than orange juice because it has fiber.
- Water is better than any sugar drink even 100% fruit juice.
Keep a List of Positive Outcomes and Health Benefits (e.g., Sleep Better, Lower Blood Pressure)
R:Weight loss in the range of 2 to 4 kg is associated with systolic blood pressure declines in the range of 3 to 8 mm Hg, a clinically significant impact (*Harsha & Bray, 2008).
Initiate Health Teaching and Referrals, as Indicated
Refer to support groups (e.g., Weight Watchers, Overeaters Anonymous, TOPS). Suggest that the individual plan to walk or exercise with someone.
R:Weight loss strategies are lifelong and may require assistance from programs, support groups, and/or exercise partner.
 AUTHOR'S NOTE
AUTHOR'S NOTE