Sudden, painless visual loss. Initially unilateral, but may rapidly become bilateral. Occurs in patients ≥55 years of age. Antecedent or simultaneous headache, jaw claudication (pain with chewing), scalp tenderness especially over the superficial temporal arteries (e.g., tenderness with hair combing), proximal muscle and joint aches (polymyalgia rheumatica), anorexia, weight loss, or fever may occur.
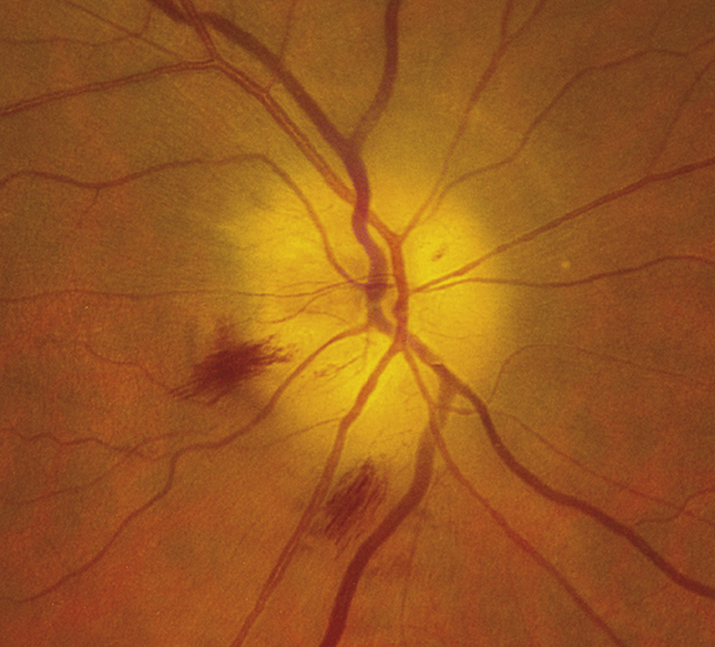
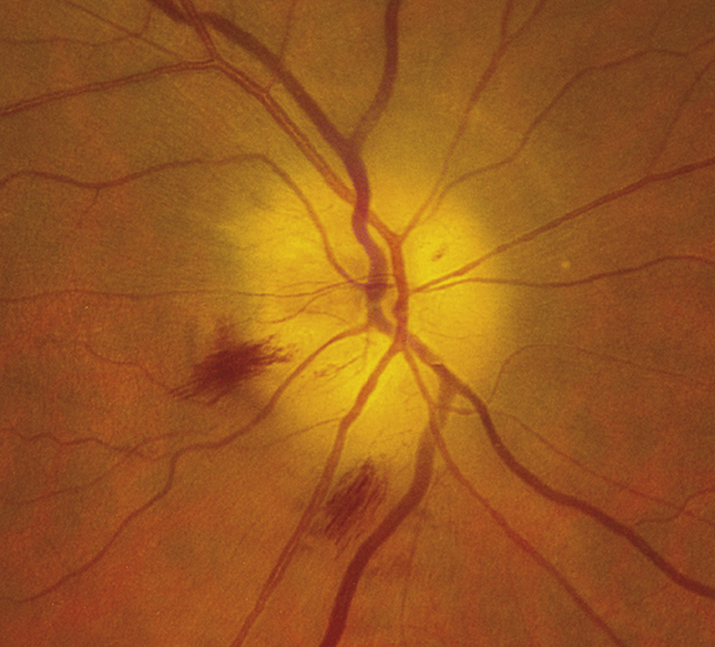
(See Figure 10.17.1.)
Critical
Afferent pupillary defect; visual loss (often counting fingers or worse); pale, swollen disc, at times with flame-shaped hemorrhages. Later, optic atrophy and cupping occur as the edema resolves. The ESR, CRP, and platelet count may be markedly increased.
Other
Visual field defect (commonly altitudinal or involving the central field); a palpable, tender, and often nonpulsatile temporal artery; and a central retinal artery occlusion or a cranial nerve palsy (especially a sixth cranial nerve palsy) may occur.
10-17.1 Chalky, pale, swollen optic disc with flame-shaped hemorrhages in giant cell arteritis.
- Patients suspected of having GCA must be evaluated and treated immediately.
- After the diagnosis is confirmed by biopsy, the initial oral steroid dosage is maintained until the symptoms resolve and lab values normalize. The dosage is then tapered slowly, repeating bloodwork with each dosage change and/or monthly (whichever appropriate based on disease stability) to ensure that the new steroid dosage is enough to suppress the disease.
- If the ESR or CRP increase or symptoms return, the dosage must be increased.
- Treatment should last at least 6 to 12 months. The smallest steroid dose that suppresses disease is used.
Tocilizumab, a novel humanized IL-6 receptor antagonist, has been recently approved by the FDA for long-term management of GCA. Addition of subcutaneous tocilizumab to standardized steroid regimens helps achieve remission faster and significantly reduces the dose and toxicity of corticosteroids.