Mild photophobia, mild pain, localized red eye, chronic eyelid crusting, foreign body sensation or dryness. History of recurrent acute episodes, chalazia, or styes.
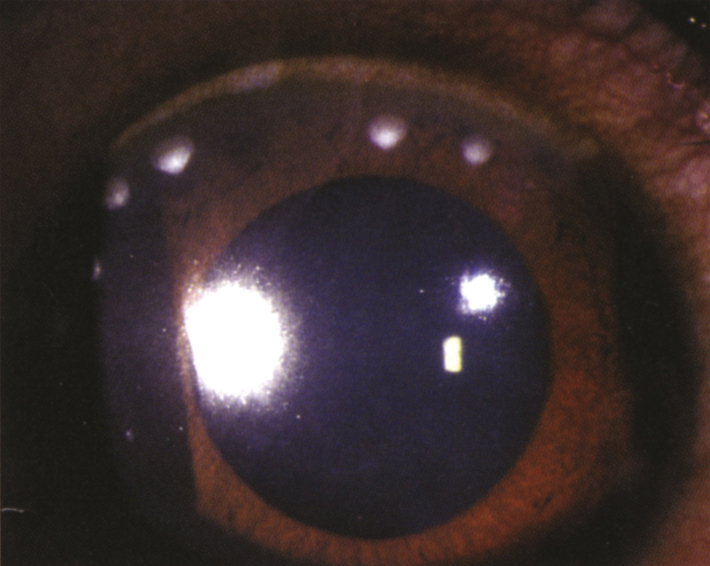
(See Figure 4.18.1.)
Critical
Singular or multiple, unilateral or bilateral, peripheral corneal stromal infiltrates often with a clear space between the infiltrates and the limbus. Variable staining with fluorescein. Minimal anterior chamber inflammation. Sectoral conjunctival injection typically occurs.
Other
Blepharitis, inferior SPK, phlyctenule (a wedge-shaped, raised, vascularized sterile infiltrate near the limbus, usually in children). Peripheral scarring and corneal neovascularization. Findings often present in the contralateral eye or elsewhere in the affected eye.
4-18.1 Staphylococcal hypersensitivity.
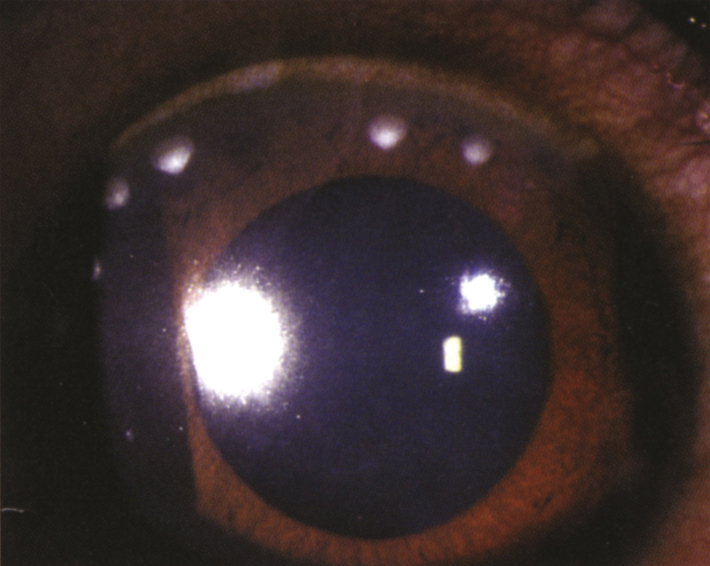
Infiltrates are believed to be a cell-mediated, or delayed, type IV hypersensitivity reaction to bacterial antigens in the setting of staphylococcal blepharitis.
 NOTE: NOTE: |
Patients with ocular rosacea (e.g., meibomian gland inflammation and telangiectasias of the eyelids) are especially susceptible to this condition. |
In 2 to 7 days, depending on the clinical picture. IOP is monitored while patients are taking topical steroids.