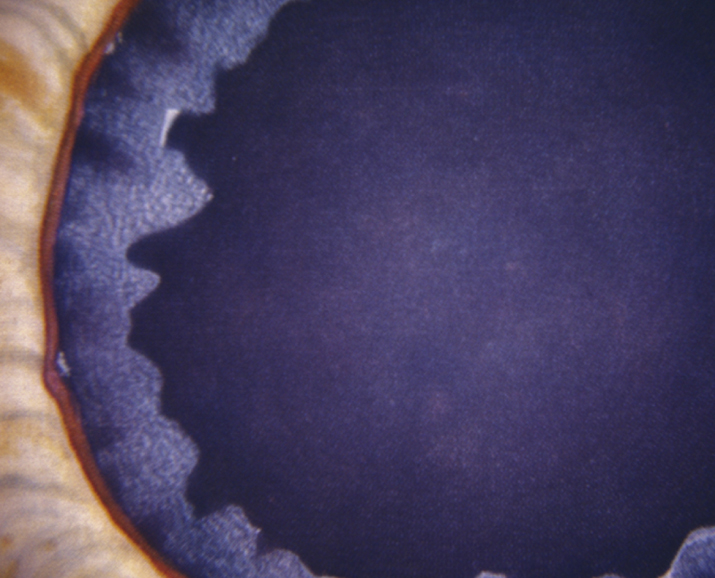
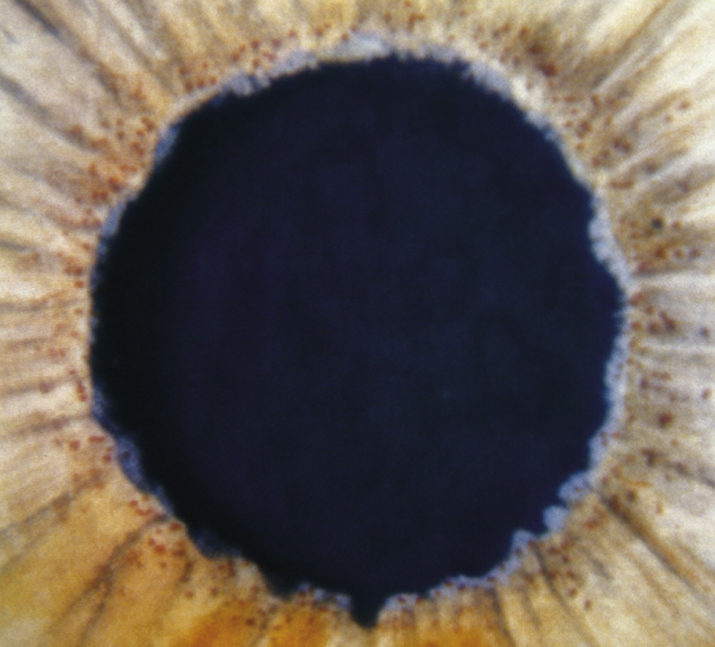
(See Figures 9.11.1 and 9.11.2.)
Critical
White, flaky material on the pupillary margin; anterior lens capsular changes (central zone of exfoliation material, often with rolled-up edges, middle clear zone, and a peripheral cloudy zone); peripupillary iris TIDs; and glaucomatous optic neuropathy. Bilateral, but often asymmetric.
Other
Irregular black pigment deposition on the TM more marked inferiorly than superiorly; black scalloped deposition of pigment anterior to Schwalbe line (Sampaolesi line) seen on gonioscopy, especially inferiorly. White, flaky material may be seen on the corneal endothelium, which often has a lower than normal endothelial cell density; can look like angular, irregular KP. Iris atrophy. Poor pupillary response to dilation (with more advanced cases, believed to be secondary to iris dilator muscle atrophy). Incidence increases with age. Zonular laxity can lead to anterior lens dislocation, angle narrowing, and secondary angle closure.